Brownish sputum is a mixture of saliva and mucus that appears in the respiratory tract. In addition, it contains dust, immune system cells, harmful microorganisms, blood components and lung decay products. Experts say if you cough up brown mucus in the morning, it's a sign of lung disease. Any change in its color is evidence of a bacterial or viral infection.
Type of sputum
Doctors call sputum a substance that is formed from saliva, mucus and bronchial cells. In the absence of diseases, it should be transparent, and its amount should not exceed a tablespoon per day. It can occur in people who smoke, those who work in hazardous workplaces, and those who inhale dry air for a long time.
The color can vary from light to dark, it all depends on what disease has affected the human body.
The discharge of yellow sputum indicates diseases such as:
- bronchitis;
- pneumonia;
- sinusitis;
- hepatitis;
- various tumors;
- cirrhosis of the liver;
- gallstones.
Yellow sputum may be a sign of hepatitis.
A yellow-greenish tint may indicate the presence of:
- acute bronchitis, and purulent;
- pneumonia;
- tuberculosis.
The rusty color indicates vascular injuries, that is, the blood, having reached the oral cavity, has had time to oxidize and turn into clots. This can happen for several reasons:
- painful cough;
- pneumonia, which led to vascular injury;
- pulmonary embolism.
If you produce yellow-green sputum, you may suspect inflammation in the lungs.
Brown or dark sputum may also indicate the presence of blood. This is possible in the following situations:
- if a person has a congenital pathology in the form of a bulla, and it was close to the lungs and for some reason suddenly ruptured, in such a situation brown sputum is expectorated through the oral cavity without coughing;
- gangrene of one or two lungs can be accompanied not only by brown discharge with an unpleasant odor, but also by fatigue, vomiting, and elevated body temperature;
- development of bronchitis;
- with lung cancer, in addition to brown mucus, there is a cough, weight loss, and increased sweating;
- During tuberculosis, a paroxysmal cough with brown sputum occurs, increased sweating at night, loss of appetite, weight loss.
The cause of brown sputum may be a cancerous tumor in the lungs.
Gray sputum when coughing can be observed with:
- gangrene of the lung;
- oncological diseases;
- smoking;
- pulmonary edema.
White color is characteristic of the following pathologies:
- with ARVI, thick sputum with mucus occurs;
- in case of cancer (especially lungs), it has a white color with blood impurities, in addition there is weight loss and rapid fatigue;
- asthma, during attacks of which light or clear sputum is released.
Any color other than clear or white is considered pathological.
The discharge of white sputum is characteristic of asthma
Signs that accompany brown sputum
Symptoms that are observed along with brown sputum serve as additional signs, with the help of which you can add up the clinical picture.
Dark sputum is not a definitive indicator of the presence of a particular disease.
Associated symptoms include:
- Breathing becomes impaired, shortness of breath and a feeling of suffocation appear, varying in intensity.
- Regular pain in the chest area, aggravated by inhaling and exhaling air.
- The man's skin changed color to gray. The symptom indicates severe intoxication, which manifests itself with prolonged smoking.
- Increased body temperature. If the high temperature does not go down, this may be a sign of infection, tuberculosis, or cancer.
What does brown sputum tell us when coughing?
In a healthy person, the glands of the trachea and bronchi secrete about 100 ml of tracheobronchial secretion daily. It covers the mucous membrane of the airways, thereby creating protection from dust and pathogenic bacteria.
In the presence of a pathogen or other provoking factor, the physical characteristics of this fluid change: the volume and viscosity increase so that as many irritating elements as possible are removed from the bronchial tree. Thickening of the secretion leads to a slowdown in its excretion and accumulation on the surface of the mucous membrane. Subsequently, this substance is expectorated during coughing.
Changes in the transparency and color of sputum occur due to the presence of macrophages and lymphocytes - immune cells capable of neutralizing foreign organisms. They penetrate the tracheobronchial mucus from the blood by increasing the permeability of the walls of blood vessels. Together with them, red blood cells penetrate into the mucous secretion, which, when disintegrating, turn it brown.
The color of sputum may change when coloring substances contained in the inhaled air enter it. “Smoker's Bronchitis” is a prime example of this. Then the expectorated dark clot of mucus, in addition to dead blood cells, contains tobacco tar. They also tint the discharged secretion brown.
What diseases cause such sputum?
Brown sputum when coughing indicates congestion in the respiratory system. Their development is promoted by inflammatory respiratory diseases, viral infections and other pathogenic factors that affect the viscosity of tracheobronchial secretions.
People with diseases characterized by:
- inflammation of the bronchi and lungs;
- necrosis of tissues of the respiratory organs;
- blockage of pulmonary blood vessels;
- the presence of pathological neoplasms in the respiratory tract.
The appearance of brown sputum during a sore throat indicates that the infection has spread down the larynx and invaded the trachea.
Bronchitis as a cause
The most common cause of brown sputum is bronchitis. On the bronchial mucosa there are many cells that are responsible for the functions of the body, and each has its own significance. The goblet is responsible for protecting the lungs and cleansing them. Cilia, moving upward, help the body get rid of dust and other impurities. The mucus closes the bronchi so that no negative factors can affect the body as a whole. In this case, the expectorated sputum is brown in color.
When the bronchi become inflamed, the cilia are unable to protect them, and dust, along with the infection, enters the bronchi, resulting in obstruction. This is exactly what the mechanism of development of bronchitis looks like, in which the cough attacks mainly in the morning.
Tuberculosis
The disease can be identified using the following symptoms:
- general malaise;
- fast fatiguability;
- shiver;
- dry painful cough, especially at night and in the morning.
One of the reasons for the appearance of brown sputum may be tuberculosis.
If the disease progresses, the skin may change to a pale color. There is weight loss and pain in the chest. Body temperature can reach 39-40 degrees.
We recommend reading: Ginger for coughs - a recipe for adults for colds and bronchitis, does milk with the root help, how to prepare it with lemon and honey?
Pneumonia
If shortness of breath, difficulty breathing, or pain in the sternum appears, this means that the process of infection of the lung tissue has begun. In this case, there is rapid fatigue, pain in muscle tissue, first a dry and then a wet cough, and at the same time coughing up brown sputum.
A complication of pneumonia can be an abscess, which appears due to infection of the lung tissue. This creates a cavity in the lungs where sputum collects.
In what cases is sputum normal?
The bronchial mucosa, consisting of cells, is covered with cilia. They are constantly on the move. The basis of sputum is mucus, which is produced by goblet cells. It is necessary to cleanse the body of all impurities in the form of dust, dirt, and microbes.
The release of clear sputum in a small amount is not a deviation and is necessary for the normal functioning of the bronchi
Without secretion, the bronchi would become covered with dust, soot and other harmful impurities, and accordingly, the tissues would be constantly inflamed. Therefore, a small amount of light-colored sputum should be gradually released from the body and come out.
Smoking
Tobacco smoking is fraught with a host of pathological changes in the upper and lower respiratory tract. If you believe medical statistics, numerous genetic mutations are found in the oral cavity, on the epithelium of the mucous membrane of the bronchi and lungs in smokers.
Smoking causes problems for many reasons. First of all, capillary permeability increases, blood leaves the vessels and settles in the sputum.
The body perceives the substance as a pathogenic organism and begins more active mucus synthesis. The result is oxidation of the hematological fluid.
In addition, destruction of small blood vessels is detected due to their stenosis or occlusion by cholesterol plaques.
This is a dangerous condition. Over time, the destruction of large main vessels and the development of malignant tumors occurs.
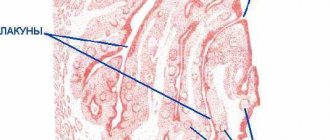
Bronchiectasis
Bronchiectasis of the lungs
Bronchiectasis is rarely primary. Those most at risk are representatives of hazardous professions, athletes, smokers, children who have had pneumonia and bronchitis.
The essence of the pathological process is the formation of sac-like structures in the area of the bronchial alveoli. They expand and are filled with serous-purulent exudate. The pus is multi-layered, multi-colored.
The condition is extremely dangerous, as it is fraught with the development of secondary infectious lesions of the lungs of an extensive type.
Oncological diseases
They occur frequently. Lung cancer, in its own way, holds the record for mortality and incidence.
The nature of the process is the degeneration of healthy lung tissue into atypical forms, followed by proliferation and infiltrative penetration into surrounding and distant organs and tissues through metastasis. The mortality rate of lung cancer is high.
There are other reasons not indicated in this list, but their proportion is so small that it is not of great importance. Brown sputum is always a warning sign.
Cough is a symptom that is familiar to everyone
It accompanies both the common cold and serious diseases, including diseases of the lungs, heart and even stomach.
Most people prefer to treat their cough on their own. But not everyone knows that it is not the cough itself that needs to be treated, but the disease that led to its occurrence. A little anatomy A person takes about 20,000 breaths a day. At the same time, approximately 8000 liters of air enter the respiratory tract. The respiratory tract is divided into upper and lower: upper respiratory tract
- this is the nasal cavity
- pharynx (nasal, oral and laryngeal parts)
- larynx
lower respiratory tract
- these are the trachea and bronchi
Normally, about 2 liters of mucus are formed in the respiratory tract per day, which contributes to the natural cleansing of the respiratory tract. The mucous membrane of the bronchi is designed in such a way that the mucus, with the help of special cilia, rises up into the pharynx and is then swallowed. And from the upper respiratory tract (nose and nasopharynx), mucus freely flows down and is also swallowed.
If there is a violation of the mucous membrane (for example, smokers have no cilia in the bronchial mucosa) or any factors cause thickening of the mucus, then it cannot be excreted freely and stagnates. All this leads to irritation of the so-called. cough receptors (special cells that are involved in the cough reflex). It turns out that cough receptors are present not only in the respiratory tract, but even in the heart and stomach. Those. diseases not only of the respiratory tract will be accompanied by a cough.
Thus, a cough that occurs as a result of severe arrhythmia helps the patient not to lose consciousness and even helps restore the normal rhythm of heart contractions. What is a cough like? The cough can be constant and short, barking and silent... Coughs are also divided into wet (doctors call it “productive”) and dry (“unproductive”).
A wet cough produces sputum. It can be liquid or thick, mucous (transparent) or purulent (yellow, green). If the sputum is red or brown, contains streaks or blood clots, then this symptom is called hemoptysis. The amount and nature of sputum gives the doctor information about the cause of the cough. For example, thick green sputum indicates severe inflammation that should be treated with antibiotics.
And depending on whether sputum comes out at all, it will depend on what medications need to be prescribed. For example, if you have hemoptysis, you should not take expectorants, because they may increase the amount of blood in the sputum. And with a dry cough, the use of expectorants can intensify the cough, even to the point of suffocation. A cough that takes up to 3 weeks to cure is an “acute” cough; it most often accompanies ARVI. If the cough persists for more than 3 weeks, it is called “chronic.” Chronic cough is a sign of a serious illness.
Different diseases - different coughs.
Diseases of the upper respiratory tract The most common cause of cough is the familiar acute respiratory disease (ARI). The cough is usually dry, accompanied by pain and sore throat. A runny nose during acute respiratory infections can also cause coughing due to mucus draining down the back wall of the throat.
Bronchial asthma In approximately 10% of cases, the only manifestation of bronchial asthma is a cough.
With an exacerbation of bronchial asthma, a narrowing of the lumen of the bronchi occurs, which complicates the passage of air mainly during exhalation and leads to coughing, wheezing or attacks of suffocation. A typical cough is that it occurs at night and in the early morning hours.
Inflammatory diseases of the bronchi and lungs: bronchitis and pneumonia Inflammation and the presence of mucus in the respiratory tract leads to irritation of cough receptors during bronchitis and pneumonia. With these diseases, the cough is very rarely dry and is always accompanied by an increase in body temperature.
Smoker's cough Smokers are characterized by a cough in the morning with the discharge of thick sputum and frequent coughing throughout the day. If smoking has not led to the development of a chronic disease, then it is enough to give up the bad habit for the cough to disappear on its own.
Gastroesophageal reflux disease This disease causes the valve that separates the esophagus from the stomach to relax. Reflux is the reflux of food from the stomach back into the esophagus. Heavy eating, bending the body, and even singing can provoke the contents of the stomach to enter the esophagus. The acid contained in the gastric juice irritates the esophagus and can lead not only to heartburn, but also to cough. Sometimes a cough is the only sign that something is wrong with your stomach.
Cardiac cough Most heart diseases result in the heart not being able to pump the required amount of blood. Blood “stagnates” in organs, incl. and in the lungs. This leads to irritation of the cough receptors. A dry cough occurs, worsening in a horizontal position. The cough may be accompanied by palpitations, a feeling of shortness of breath, and shortness of breath. There is no treatment for such a cough; it will disappear on its own if the signs of heart failure are eliminated.
Cough due to medications Taking a number of medications can lead to side effects such as coughing. The reasons for this effect of drugs have not yet been sufficiently studied. It helps to recognize that medication has led to the development of a cough if there was no cough before the medication was prescribed. The cough bothers you mainly in the daytime, it is dry, and more often it is a small but debilitating cough. 3-7 days after discontinuation of the drug, the cough disappears. Cough with tumors Some lung tumors for a long time can manifest themselves only as a cough: dry or with the release of a small amount of light sputum. No changes are detected on radiographs of the lungs. Only visiting a doctor and carrying out special research methods helps make a diagnosis at an early stage.
Cough with whooping cough Whooping cough is an infectious disease that occurs with a prolonged paroxysmal spasmodic cough. In the first 2 weeks, the cough is similar to the cough of a common cold and may be accompanied by a runny nose and a slight increase in body temperature. Starting from the third week, a period of debilitating cough begins. The cough comes in attacks that are repeated from 2 to 15 times in a row. Such a cough must be treated, because... it leads to serious complications. Complications that a cough can lead to. Frequent persistent cough, especially in the form of prolonged attacks, leads to an increase in intrathoracic pressure and can contribute to the development of: - pulmonary emphysema - cardiac complications (arrhythmias, increased ischemia, development of cor pulmonale) - hemorrhage in the sclera of the eyes - dizziness - fainting - deterioration of cerebral blood circulation (especially if there have been previous strokes) - lung rupture
In addition, cough can lead to headache, vomiting, sleep disturbances, and urinary and fecal incontinence in an elderly, debilitated patient. Chronic cough can lead to the formation or enlargement of existing hernias (diaphragmatic, inguinal, scrotal, etc.). Chronic cough can cause depression, which complicates the patient's relationships with others, which ultimately significantly worsens the quality of life. What research needs to be done.
In order to avoid serious complications and make a timely diagnosis, you must consult a doctor.
Depending on the characteristics of the cough, its duration, and based on the results of the examination, the doctor will prescribe an examination. As a rule, this is a clinical blood test, fluorography and a study of external respiratory function. If the results of these studies do not help determine the diagnosis or even during the examination one can suspect that they will not be enough, the doctor prescribes more complex studies (for example, bronchoscopy, computed tomography, lung scintigraphy) and consultations with specialists. You can hardly find a person who has never coughed. And, of course, there is no need to consult a doctor every time at the first sign of a slight sore throat or slight cough. These disorders are transient. However, it should be remembered that only a doctor can reliably recognize the cause of cough and prescribe the necessary treatment.
Symptoms that should alert you and prompt immediate medical attention: - hemoptysis (sputum is uniformly red or with red/brown streaks) - increased body temperature for more than 3 days - choking or shortness of breath - cough for more than 3 weeks - chest pain - nausea and vomit"
Smokers
Mostly brown sputum appears in a smoker in the morning. When a person sleeps, mucus accumulates, and when he wakes up, phlegm begins to leave the bronchi naturally. A person who smokes for a long time eventually develops so-called smoker's bronchitis. Moreover, the cough becomes his constant companion. Naturally, smokers do not monitor their health, so they do not pay due attention to the color of the discharge. They are accustomed to a morning cough and do not consider this a cause for concern. However, brown sputum is considered an ideal breeding ground for bacteria.
Thus, by introducing harmful smoke into the body, smokers slowly poison it with heavy elements. Therefore, it is better to give up such a bad habit in order to exclude more serious diseases and complications in the future. People who have continuously consumed harmful cigarette smoke for several years in a row need to cleanse their lungs. To do this, you can use breathing exercises, which are popular today, with which you can improve the health of the entire body. The doctor may also prescribe you expectorant medications or a more gentle healing option using inhalations. Visit the clinic and the doctor will tell you which method is best for you. The doctor will monitor your health throughout the course of therapy, so no complications will arise.
And if phlegm is felt only in the morning, what is it?
In some pathologies, the secreted tracheobronchial secretion is expectorated only in the morning. This is explained by the fact that the fluid released during sleep accumulates in the lower parts of the nasopharynx, and then, when the body position changes, it begins to move down the trachea, simultaneously irritating the cough receptors. In a healthy person, the result of a morning cough is usually clear mucus.
However, this indicator changes due to the presence of foreign impurities:
- Brown sputum in the morning becomes one of the signs of “smoker's bronchitis.” The coloring of the secretion occurs due to the accumulation of tar and other combustion products of tobacco.
- The appearance of a morning cough with the release of a small amount of mucus may be a consequence of reflux esophagitis. With it, due to the weakness of the sphincter muscles, the contents of the stomach are thrown into the esophagus and throat. This provokes inflammation of the mucous membrane of the digestive tract, and then the trachea.
- Chronic inflammation of the bronchi. In this case, in the morning hours, a small amount of sputum is coughed up, the color of which becomes yellow or yellow-green during exacerbation. It occurs against the background of prolonged inhalation of caustic chemical compounds contained in the air (tobacco smoke, dust, exhaust gases, toxic fumes).
- Exacerbation of bronchiectasis. The patient complains of the appearance of sputum with pus in the morning, loss of strength, low-grade body temperature, shortness of breath, and bluish discoloration of the skin.
- Congestion in the bronchi and lungs is a specific symptom of heart disease.
Morning cough in children is considered a characteristic sign of adenoiditis - chronic inflammation of the pharyngeal tonsil of the lymphopharyngeal ring. Develops due to frequent ARVI.
Causes of changes in the color of bronchial secretions
Brown sputum when coughing occurs due to the ingress of red blood cells - red blood cells, which oxidize and undergo breakdown in the lower respiratory tract. This determines the characteristic color of the discharge. There are certain reasons for such pathological changes:
- Smoking cigarettes. This addiction has an extremely negative effect on the organs of the respiratory system, causing a cascade of pathological reactions there. According to special studies, in people who systematically inhale tobacco smoke, the epithelial cells of the intima of the bronchi and oral cavity undergo mutational changes.
Under the influence of harmful substances released during the combustion of tobacco, the vascular wall of the bronchial capillaries becomes permeable. As a result of this, red blood cells from the vascular bed enter the lumen of the bronchi and mix with sputum, undergoing decay and oxidation. The body tries to quickly get rid of red blood cells that have entered the respiratory tract. Because of this, secretion production increases and a cough appears.
A cough with a large amount of sputum is especially bothersome for smokers in the morning. This is due to the fact that during sleep it accumulates and stagnates. When a person wakes up and moves actively, copious discharge of accumulated secretions begins.
The admixture of red blood cells in sputum is a breeding ground for pathogenic microflora, which causes inflammatory diseases of the respiratory tract in smokers. Also, with the help of bronchial exudate, the body tries to remove toxic substances coming from tobacco smoke.
Associated symptoms
They occur as additional, optional signs that make up the clinical picture.
It is important to keep in mind: dark mucus is never the only sign. The fact that you cough up brown mucus in the morning is not an indicator.
Accordingly, we can talk about the following characteristic symptoms:
- Increase in body temperature to subfebrile-febrile values. Indicates either an infectious process, or tuberculosis, or oncology, if elevated thermometer values are constantly maintained.
- An alarming symptom is constant pain in the chest when inhaling and exhaling. This is a direct indication of the presence of a pathological process in the lower respiratory tract. This phenomenon may be absent in the presence of focal small-segmental lesions.
- Breathing problems in the form of shortness of breath or suffocation are common. One differs from the other in intensity.
We recommend reading: How not to get confused about body temperature standards in children?
The described symptoms need to be considered in conjunction with the main manifestation - brown sputum when coughing and its shade. A specific diagnosis can only be made by a doctor based on the results of an objective study.
How to get rid of this phlegm at home
Treatment of any cough should be carried out under the supervision of a doctor, since incorrect diagnosis and abuse of traditional medicine can provoke a worsening of the patient’s condition. For example, acute bronchitis can be complicated by pneumonia, and whooping cough can be complicated by the formation of mucous-epithelial plugs.
Infusions and decoctions of herbs will help induce a productive cough when fluids stagnate in the respiratory organs. Such properties are found in the leaves of coltsfoot, marshmallow root, oregano and licorice.
Sage, calamus, thyme (thyme), plantain and fennel can be used as natural antiseptics for bacterial infections. In addition to the antimicrobial effect, they also have antispasmodic, vasodilating, analgesic, enveloping, hemostatic and tonic properties.
When you cough, brown mucus comes out much more intensely if you drink a lot of warm liquid. For example, it could be a mixture of milk and mineral water in a ratio of 3/1. You need to consume it in small sips throughout the day.
If cough is difficult and there is no elevated body temperature, inhalations based on mineral water or saline are indicated. solution. With their help, the viscous secretion will become more fluid. It should be remembered that it is recommended to do the procedure a maximum of 2 hours before bedtime.
What to do if brown sputum appears?
A pulmonologist treats diseases associated with inflammation of the airways. You can get to him through a therapist who will give you a referral. Before visiting a specialist, it would be advisable to do a sputum test.
To do this, you need to purchase 2 sterile containers. The day before the test, drink plenty of warm water. In the morning, before hygiene procedures, you need to collect material for research: take 2-3 deep breaths and cough up sputum. Then spit approximately the same amount into each of the jars separately: for the clinical and bacteriological laboratory.
Diagnosis of some diseases will require testing several times.
Diagnosis of sputum by consistency and smell
In order to evaluate this criterion, it is necessary to expectorate sputum into a transparent glass container, evaluate it immediately, and then remove it, cover it with a lid, and let it sit (in some cases, the sputum may separate, which will help in diagnosis).
- Mucous sputum: it is released mainly during ARVI;
- Liquid colorless is characteristic of chronic processes developing in the trachea and pharynx;
- Foamy white or pinkish sputum is released during pulmonary edema, which can accompany both heart disease and inhalation gas poisoning, pneumonia, and inflammation of the pancreas;
- Sputum of a mucopurulent nature can be released with tracheitis, sore throat, bacterial bronchitis, complicated cystic fibrosis and bronchiectasis;
- Vitreous: characteristic of bronchial asthma and COPD.
An unpleasant odor is characteristic of complicated bronchiectasis or lung abscess. A fetid, putrid odor is characteristic of lung gangrene.
If the sputum separates into two layers when standing, it is probably a lung abscess. If there are three layers (the top one is foamy, then liquid, then flaky), this may be gangrene of the lung.
Treatment
Help before diagnosis
In case of acute inflammatory damage to the respiratory system, unimpeded discharge of mucous sputum should be ensured. To improve the drainage function of the bronchial tree, it is recommended to drink plenty of warm drinks and maintain optimal air humidity in the room. All drug treatments can only be used after a visit to a doctor.
Conservative therapy
Mucous sputum as a symptom does not require special treatment, since it disappears after affecting the underlying disease. In cases where there is too much mucus and its expectoration is difficult, postural drainage techniques are recommended, and medications with mucolytic and secretomotor effects are prescribed. Physiotherapy methods are effective - alkaline and oil inhalations, UHF and electrophoresis on the anterior surface of the chest.
To influence the root causes of the discharge of mucous sputum, antiviral and antiallergic drugs are used. Antibiotics are not indicated; they are used only when the bronchial discharge is mucopurulent. Anti-inflammatory medications speed up recovery and relieve subjective symptoms. For chronic bronchitis, therapeutic bronchoscopy is performed for lavage and targeted administration of medications.
Possible complications
Over time, smokers may develop malignant neoplasms in the oral cavity, upper and lower respiratory tract. With the progressive course of pneumonia, there is a risk of developing severe respiratory failure, which is treated in an intensive care unit with the help of artificial ventilation. If large vessels are damaged, pulmonary hemorrhage may occur - this condition requires urgent hospitalization in the intensive care unit.
Treatment methods
Therapy is specific and depends on the symptom of which disease is cough with brown secretion. The most commonly prescribed medications are:
- Non-steroidal anti-inflammatory analgesics. They suppress the activity of the inflammatory process and relieve pain. These include “Depiofen”, “Ibuprofen”, “Ketanov”, “Arthrocol”.
- Expectorants and mucolytics – “Mukolvan”, “Lazolvan”. They dilute mucus and facilitate the process of its removal.
- Bronchodilators - dilate the bronchi, making breathing easier.
Surgical interventions are indicated for some forms of tuberculosis, as well as for oncological pathologies.
Drug therapy
The choice of treatment depends on the specific disease, the symptom of which is the production of brown sputum. In most cases, the doctor prescribes the following medications:
- Expectorant, mucolytic agent: Lazolvan, Mukolvan. Taking them helps to liquefy and remove brown mucus.
- Taking bronchodilators helps expand the bronchi, ease breathing, and relieve shortness of breath.
- Suppression of the activity of the inflammation process and pain relief occurs due to non-steroidal analgesics: Ketanov, Nise, Ibuprofen.
- Surgical intervention is required for oncology, tuberculosis, bronchiectasis.
Traditional medicine
Taking some folk remedies will help facilitate the process of mucus discharge, as well as improve its dilution. An infusion of pine buds in milk, which must be kept for about one hour, has worked well. It has a softening and moisturizing effect on the mucous membrane of the bronchial tree.
A decoction of marshmallow grass, mint leaves and plantain, prepared in a water bath, is good for removing phlegm. It must be taken at least three times a day, preheated. You can drink onion broth with sugar, but it does not taste very good.
If a symptom such as a cough with brown sputum appears, it is better not to self-medicate, but to seek help from a doctor! He will prescribe the necessary examinations to identify the cause of such a cough and recommend effective treatment methods.
Prevention
Coughing up brown mucus is one of the symptoms of the disease. Therefore, when it first appears, you need to consult a doctor. Only a specialist will be able to correctly interpret it and prescribe the necessary treatment.
After undergoing therapeutic measures, in order to avoid relapse of the pathology, you should adhere to some rules:
- stop smoking;
- competently organize the environment - observe the temperature and humidity conditions of residential premises;
- prevent air pollution from dust;
- carry out work with pesticides only with personal protection;
- adhere to doctor's orders.
Possible causes of sputum without cough and additional symptoms
Sputum is mucus that is secreted by glandular cells of the trachea, nasal cavity, paranasal sinuses and bronchi. Normally, no more than 100 ml of mucus accumulates in the tracheobronchial tree per day. It has bactericidal properties and is involved in the removal from the respiratory tract:
- dust;
- allergens;
- pathogenic agents.
When the mucous membrane is irritated, the activity of glandular cells increases 10 times or more. Therefore, in case of illness, up to 4 liters of pathological sputum are produced per day.
Expectoration of mucus without coughing is a nonspecific symptom that accompanies pathologies of various systems:
- respiratory;
- digestive;
- endocrine;
- nervous.
To find out the cause of the condition, you need to determine:
- the nature of sputum - elasticity, transparency, color, smell;
- associated symptoms – chest pain, sore throat, burning sensation in the nose;
- factors that provoke exacerbation are strong odors, physical activity, drinking hot drinks, etc.
Expectoration of mucus without coughing in half of the cases indicates damage to the nasopharynx or bronchopulmonary system.
Worm infestation
If a child or adult does not cough up clear or white sputum, the cause may be helminthiasis. In the acute phase, parasite larvae circulate in the blood and enter the bronchi. They irritate the mucous membrane, causing a productive cough. A person complains about:
- chest pain;
- swelling of the mucous membranes;
- shortness of breath;
- nausea.
When the mucus is swallowed, the worms enter the intestines, where they develop into adults. In the later stages, helminthiasis manifests itself:
- abdominal pain;
- unstable stool;
- weakness;
- sleep disturbance;
- elevated temperature;
- convulsions.
We recommend reading: Herpes (cold) on the tongue in adults and children: causes, symptoms, treatment
With a chronic disease, immunity decreases, so rhinitis, tracheitis, and influenza often recur.
Esophageal diverticulum
An esophageal diverticulum is a saccular bulge in the wall of the esophagus. It manifests itself as dysphagia, bad breath, and a feeling of a lump in the throat. Many people experience hypersalivation - excessive production of saliva, so they complain of copious sputum discharge without coughing attacks.
Associated symptoms depend on the location of the diverticulum. The most striking clinical picture when a protrusion forms in the clavicle area:
- change in voice timbre;
- nausea;
- scratching in the throat;
- expectoration of thin sputum;
- regurgitation of food;
- backflow of mucus from the esophagus into the throat.
Large diverticula put pressure on the respiratory system, causing coughing. It is combined with chest pain and dizziness.
Inflammation of the adenoids
Sputum without cough in a child appears against the background of adenoiditis. This is the name for inflammation of an enlarged nasopharyngeal tonsil. The adenoids block the nasal passages, so viscous secretions accumulate in the nasal cavity. During sleep, it flows into the throat through the back wall of the pharynx.
Manifestations of adenoiditis:
- night snoring;
- violation of nasal breathing;
- coughing up yellow mucus;
- restless sleep;
- headache;
- elevated temperature.
There is no cough while awake. It occurs in the morning or immediately after waking up due to irritation of the throat by nasal secretions. If left untreated, the Eustachian tube becomes inflamed (eustachitis), so the child complains of decreased hearing acuity and ear pain.
Sjögren's syndrome
Sputum without fever and cough is one of the signs of Sjögren's disease. It is characterized by damage to connective tissue and exocrine glands. Accompanied by sinusitis and tracheobronchitis, separation of rusty sputum.
Symptoms of Sjögren's disease:
- muscle and joint pain;
- dry eyes;
- seizures in the corners of the mouth;
- violation of the act of swallowing;
- prostration;
- dry tongue;
- formation of crusts in the nose;
- enlargement of the parotid glands.
The mucous membrane of the throat dries out and acquires a bright red tint. If the glands are insufficient, the saliva becomes viscous.
Due to dysphagia (impaired swallowing), the patient cannot swallow it. Therefore, there is a feeling of mucus accumulation in the throat.
Allergy
Sputum production without coughing is one of the signs of a respiratory allergy. Irritants (allergens) are:
- medicines;
- plant pollen;
- Food;
- fumes from household chemicals;
- dust mites.
Manifestations of respiratory allergies:
- labored breathing;
- redness of the throat mucosa;
- nasal congestion;
- lacrimation (with hay fever);
- pain when swallowing;
- hoarseness of voice.
Depending on the location of the inflammation, the allergy occurs with or without a cough.
Patients complain of expectoration of clear, viscous sputum, which sometimes becomes glassy. In the absence of treatment, the clinical picture is supplemented by new symptoms - spasmodic cough, shortness of breath, swelling of the mucous membranes.
Pharyngitis, laryngitis, tonsillitis
Phlegm in the throat without cough in children and adults occurs due to inflammation:
- palatine tonsils – tonsillitis;
- pharynx – pharyngitis;
- larynx - laryngitis.
If the secretion is transparent, this indicates the onset of the disease or the attenuation of inflammation. In the absence of complications, the cough does not bother you, and small amounts of sputum are expectorated. If it becomes thick and green, purulent inflammation is possible.
The release of viscous mucus without coughing after laryngitis is a sign that the inflammation has become chronic.
Sinusitis and rhinitis
Thick mucus is released without coughing in case of inflammation of the nasopharynx and paranasal sinuses. Copious sputum is expectorated in the following diseases:
- Rhinitis (runny nose). Inflammation of the nasal mucosa is accompanied by the secretion of viscous mucus. Its transparency and elasticity depend on the form of the disease. An infectious runny nose produces yellow or green mucus. In people with insufficient tone of blood vessels, vasomotor rhinitis occurs, in which a transparent secretion is formed. With atrophic rhinitis, foul-smelling green sputum occurs.
- Sinusitis. When the maxillary sinuses become inflamed, sinusitis occurs, the ethmoid sinuses - ethmoiditis, the sphenoid sinuses - sphenoiditis, and the frontal sinuses - frontal sinusitis. If you cough up white, thick mucus without coughing, the cause of the illness is a viral infection or allergy. With bacterial and fungal inflammation, it acquires a yellow or green tint and an unpleasant odor.
Expectoration of mucus without coughing occurs mainly in the morning, as during the night it flows down the back wall of the throat into the hypopharynx.
Other reasons
Foul-smelling mucus without coughing is a dangerous symptom that occurs against the background of purulent inflammation of the ENT organs. Without treatment, complications are possible - abscess and gangrene of the lung, sepsis (blood poisoning).
Possible causes of expectoration:
- lungs' cancer;
- pulmonary syphilis, disintegration of syphilitic gum;
- bronchopulmonary carcinoma;
- cystic fibrosis;
- pulmonary mycosis;
- actinomycosis;
- bullous disease;
- pleural empyema;
- COPD
Yellow sputum without cough is a sign of bacterial diseases of the nasopharynx. If clots of dried blood are found in it, this indicates mucopurulent inflammation. Brown sputum in the morning without cough occurs with bronchiectasis and cardiac pathologies.
What to do if you produce sputum without coughing?
If sputum is produced for a long time, consult a physician or pulmonologist. During the interview, the doctor will clarify:
- how long ago the symptom appeared;
- presence of bad habits and occupational hazards;
- tendency to allergic reactions.
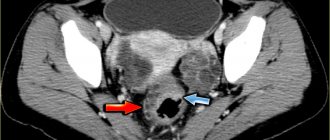
To determine the cause of expectoration of mucus without coughing, a diagnosis is carried out:
- physical examination - examination of the throat, listening to the lungs;
- endoscopic examinations – broncho-, rhino- and pharyngoscopy;
- hardware methods - MRI of the chest, radiography of the lungs, ultrasound of the pleural cavity;
- laboratory tests - microscopic examination of sputum, general blood test, allergy tests.
To exclude helminthiasis, fungal infection of the lungs and syphilis, an enzyme-linked immunosorbent test is prescribed to determine antibodies to the pathogen. If tuberculosis is suspected, the quantiferon test and the Mantoux test are recommended.
Treatment options depend on the cause of excessive mucus production. Conservative therapy involves taking medications, physical procedures - magnetic therapy, inhalations, chest massage, UHF therapy. The basis of pharmacotherapy is:
- antibiotics – Doxycycline, Amoxiclav, Augmentin;
- anthelmintics – Vermox, Trichlorophen, Piperazine;
- anti-tuberculosis drugs - Pyrazinamide, Ethionamide, Isoniazid;
- antifungal drugs - Itraconazole, Fluconazole, Isavuconazole.
To facilitate the removal of sputum, mucolytic and expectorant drugs are used - Mucaltin, Tussin, Bronkatar, ACC.
There are several dozen diseases in which sputum is expelled without coughing. Some of them do not pose a threat to health, while others are fraught with dangerous complications. Therefore, if such a symptom appears, you should not postpone a visit to a therapist or pulmonologist.
Diagnostics
The initial examination of a patient with complaints of mucous sputum is often performed by a general practitioner, who, if necessary, gives a referral to an otolaryngologist or pulmonologist. To make a preliminary diagnosis, it is enough to collect complaints, auscultate the lungs, and visually examine the tonsils and pharynx. The plan for clarifying diagnostic studies includes the following methods:
- ENT examination.
With direct and indirect laryngoscopy, the doctor assesses the condition of the laryngeal mucosa, identifies signs of inflammation and hypertrophy. Using a fibrolaryngoscope, a biopsy of atypical areas is performed. If a chronic runny nose is suspected, anterior and posterior rhinoscopy provides valuable information. - X-ray of the OGK.
Carrying out an x-ray in two projections allows us to identify changes typical of inflammatory or tumor processes of the bronchopulmonary system. To clarify the diagnosis, targeted studies are prescribed: fluoroscopy and MRI of the chest organs. - Endoscopic diagnostics.
During bronchoscopy, the mucous membrane of large and medium-caliber bronchi is visualized. The method is used to diagnose chronic bronchitis, neoplasia, fibrotic changes. Using endoscopy, biopsies for histological examination and bronchial lavage water are taken. - Sputum analysis.
Culture of bronchial mucus is necessary to identify viral or atypical bacterial infections. When microscopy of mucous sputum, attention is paid to pathognomonic crystals and spiral-shaped accumulations of mucus. To exclude tuberculosis, microscopy of the material after special staining is required.
Among laboratory methods, a general blood test is informative, allowing one to differentiate inflammatory and other pathologies of the respiratory system. In a biochemical study, acute-phase indicators are studied. Serological tests aimed at searching for antibodies to pathogenic microorganisms are recommended. To measure the function of external respiration and diagnose chronic diseases, spirometry and peak flowmetry are indicated.
Sputum analysis