Stomatitis is an inflammation of the mouth (but can also develop on the tongue and lips) that is most often diagnosed in children. Stomatitis in adults is usually a consequence of the introduction of viruses into the oral mucosa. In addition, this disease can occur in the presence of a number of other diseases, due to decreased immunity. For dentists, diagnosing and treating stomatitis in the mouth does not cause any difficulties, while attempts to get rid of the disease on their own can lead to unpleasant consequences
How does stomatitis manifest in adults?
Local symptoms include redness, swelling of the mucous membrane, spots, ulcers or wounds in case of mechanical damage1,3. They cause pain or burning5. Plaque may form in the area of inflammation. Sometimes a person complains of bad breath3. The listed symptoms can be severe or minor - it all depends on the depth of the lesion and the duration of the disease3.
In addition to local symptoms, in severe cases there are general ones, similar to those that appear with a cold - increased body temperature, general weakness and lack of appetite2.
to come back to the beginning
Symptoms of the disease
Symptoms depend on the type of pathology, but there are common clinical manifestations. As a rule, the disease does not begin acutely. The mucous membranes become red, swelling, pain, and a burning sensation appear in the affected area. You can see what stomatitis looks like in the photo.
If it is a bacterial infection, then after a day an ulcer appears at the site of infection with a red halo radiating from the center. The ulcer is covered with a white coating. During this period, salivation increases and an unpleasant odor appears. Pain bothers the patient not only when eating, but also at rest.
Pimples and ulcers appear anywhere in the oral cavity; in severe cases, stomatitis develops in the throat. Stomatitis on the tongue is especially painful, since there are many nerve endings there. Some types are characterized by bleeding gums.
With further development of the pathology, the temperature may rise, the lymph nodes may enlarge, and symptoms of intoxication may appear - weakness, nausea, lack of appetite.
Causes
Among the causes of stomatitis in adults, general and local ones are distinguished1. The latter include any damaging factors that act directly on the mucous membrane (too hot food, chemicals, mechanical damage), the general ones include chronic diseases of internal organs not related to the oral cavity (infectious, allergic, systemic), as well as metabolic disorders substances1.
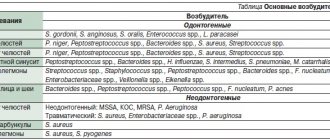
In the first place in terms of prevalence are infectious stomatitis - viral, fungal or bacterial2.
The presence of various microorganisms in the oral cavity is normal. In a healthy, intact state, the mucous membrane can resist infection. However, with a decrease in local immunity, injury or poor hygiene, pathogens can penetrate deeper layers and cause inflammation1,3,4.
The soft tissues of the oral cavity can be injured by improperly fitted dentures, pieces of food or sharp chips on the teeth. Inflammation is often provoked by thermal or chemical factors, for example, very hot or spicy food, cosmetics3.
The following factors also contribute to the development of stomatitis3,4,6:
- allergic reactions1;
- poor oral hygiene;
- dental diseases;
- heredity;
- stress;
- hormonal disorders;
- diseases of the gastrointestinal tract;
- smoking.
A drug can become an irritant that provokes inflammation; for example, stomatitis in patients with bronchial asthma occurs during the use of inhalers with glucocorticosteroids (hormonal anti-inflammatory drugs)3. Also, the protective barrier of the mucous membrane is exposed to harmful substances in the air with which a person comes into contact due to professional activities3,5.
First aid
If the temperature rises, you can take an antipyretic drug. In the future, before visiting a doctor, nothing should be done. Do not take antibiotics yourself or try to get into the ulcer with any object.
How to relieve symptoms of ulcers
- do not eat sour and salty foods
- food should be warm, no hot dishes or drinks
- Care should be taken to ensure that the child does not put dirty hands in his mouth
- teeth should be brushed, but make sure that the bristles do not touch the gums with ulcers
- It is recommended to rinse your mouth with herbal solutions (oak bark, chamomile) 3-4 times a day
You should be careful when using antibacterial solutions. They must be prescribed by a doctor. If such solutions are used incorrectly, they can provoke the development of thrush. The antibacterial agent will “kill” the beneficial microflora, which can result in a fungal infection.
Prevention of ulcers
- professional oral hygiene at least 2 times a year
- Regularly replacing your toothbrush
- Proper brushing of teeth at least 2 times a day
- using additional hygiene techniques such as irrigators, dental floss, and tongue scrapers
- Children should be monitored for bad habits such as putting dirty fingers and other objects into their mouths
- It is important to treat your teeth in a timely manner. Microbes that are found in carious teeth and rotten roots can serve as a source of infection for ulcers
If you have problems in the oral cavity, contact the specialists of the Center for Family Dentistry!
Types of stomatitis in adults
The disease can be acute or protracted. Often the process becomes chronic1. If the symptoms of stomatitis recur, it is called recurrent1.
Depending on the depth of the lesion, stomatitis occurs 1:
- superficial - occurs in catarrhal or aphthous form;
- deep - characterized by the formation of ulcers.
Let's look at each form in more detail.
Catarrhal stomatitis
If the inflammatory process is limited to the most superficial layer of the mucosa, it is called catarrhal. In addition to the typical symptoms - swelling, redness and pain in the mouth - a white or yellow coating may be observed3.
Aphthous stomatitis
This form is characterized by the formation of single or multiple aphthae - these are small defects of the mucous membrane, similar to ulcers. Aphthae of various sizes form on the lips, inner surface of the cheeks, gums, lateral surfaces of the tongue, and in severe cases even in the larynx and nasopharynx4. They have clear boundaries in the form of a narrow red rim, and in the center they are covered with a grayish-yellow coating3. The ulcers are painful4, which is why the person often refuses to eat.
Local symptoms are sometimes accompanied by general manifestations - high fever and lymphadenitis (enlarged and painful lymph nodes). If not treated in a timely manner, acute aphthous stomatitis can develop into a chronic recurrent form4.
Ulcerative stomatitis
With this form, the entire thickness of the mucous membrane is affected - deep ulcers form on it. In severe cases, body temperature rises, headache, weakness appear, and local lymph nodes become enlarged and painful3. This type of stomatitis often occurs against the background of cardiovascular diseases, infections, poisoning or diseases of the gastrointestinal tract3.
Diagnosis and treatment
To avoid the spread of the inflammatory process and its transition to a chronic form, you should not self-medicate, you should consult a doctor. First you need to make an appointment with the dentist. He examines the oral cavity and helps eliminate local factors that lead to stomatitis, for example, dentures that injure the mucous membrane or a broken tooth.
If no dental diseases are detected, the doctor may refer you for a consultation to a therapist or specialists - a gastroenterologist, allergist or endocrinologist.
If necessary, additional examination is prescribed, which may include6:
- bacterioscopic examination - scraping of plaque from the surface of the oral mucosa is needed to detect the causative agents of stomatitis;
- general blood test - required to identify the inflammatory process in the body and some signs of chronic diseases;
- allergological studies - help to identify the connection between symptoms and a specific (causal) allergen;
- immunological studies - used to assess general and local immunity.
to come back to the beginning
Treatment of stomatitis at home
I would like to immediately note that treating stomatitis with folk remedies at home is possible, but you need to understand that in many cases it is impossible to do without a visit to a specialist and the use of antibiotics. Ignoring these points can lead to worsening of the disease and longer rehabilitation. In addition, on the Internet you can find a whole lot of “revolutionary” recipes for stomatitis, so you need to be able to separate the wheat from the chaff and understand which remedies can really help, and which are the fruit of the inflamed imagination of “couch healers”. Below we publish the most common methods of preventing and treating stomatitis with folk remedies, but please note that only an experienced specialist can draw up an optimal treatment plan.
In the case of children, treatment of stomatitis with folk remedies at home is used quite often. This is especially justified as a preventive measure, since the child’s body is more susceptible to the influence of the external environment. The most popular remedies are considered to be all kinds of decoctions, for the production of which chamomile, calendula, burdock, propolis and blackberry leaves are used. A homemade ointment is also used to treat stomatitis, which is made from novocaine, egg white and honey. Be that as it may, if your child shows signs of stomatitis, it is best to immediately take him to a specialist who can make the correct diagnosis and plan treatment.
How is stomatitis treated in adults?
Complex treatment should be carried out only under the supervision of a doctor. On the one hand, it is important to eliminate the cause of the disease, on the other hand, to alleviate the symptoms and stimulate the restoration of the oral mucosa. The doctor prescribes both local and general therapy, depending on the form of stomatitis.
The following groups of drugs may be used in treatment5:
- antibacterial, antiviral or antifungal (depending on the pathogen);
- antiallergic drugs;
- anti-inflammatory drugs;
- enzymes;
- agents that stimulate the restoration of the oral mucosa;
- drugs that enhance immunity and improve metabolism.
For some forms of stomatitis, the doctor may prescribe combination medications. For example, Metrogyl Denta®, which is indicated for the treatment of aphthous stomatitis7,8,10.
Metrogyl Denta® is a dental gel that contains metronidazole, which has an antibacterial effect, and the antiseptic chlorhexidine8. This combination can suppress the activity of various types of microorganisms and helps fight infection7,8.
Metrogyl Denta® is widely used in dentistry; it is approved by the Dental Association of Russia (StAR)9. The duration of treatment, dose and frequency of use is determined by the doctor, depending on the degree of damage and severity of the disease.
The appearance of stomatitis may mean that a person has a weakened immune system or that the mucous membrane has been affected by some damaging factor. And sometimes redness and painful sores in the mouth are symptoms of a chronic disease1. A dentist helps to understand the causes and cope with inflammation, and if stomatitis has “deeper roots,” specialized specialists are involved in the treatment. After therapy, it is important to do everything to prevent the disease from occurring again. You need to regularly visit the dentist, replace dentures if they cause mechanical injury, monitor oral hygiene and give up bad habits1,5.
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
to come back to the beginning
Prevention of stomatitis
Consists of the following items:
- strengthening the immune system, giving up bad habits, hardening, playing sports, eating with a sufficient amount of macros and vitamins (especially vitamin C)
- regular visits to the dentist
- adequate brushing of teeth at home, as well as removal of dental plaque in the dentist’s office once every 6 months
- identifying the allergen and avoiding contact with it
- undergoing medical examination for timely detection of diseases
- treatment of systemic diseases
- taking antibiotics only as prescribed by a doctor, together with a course of probiotics, to avoid dysbiosis
- vaccination (against measles, chickenpox)
Tantum® Propolis
It is worth paying attention to Tantum Propolis, since propolis has an immunostimulating effect, promotes healing, and vitamin C, which is part of it, is responsible for regeneration, participating in the synthesis of collagen.
Propolis also has antiviral and antifungal effects. Therefore, vitamin therapy Tantum Propolis is an effective means of preventing stomatitis.12 Find out more
Literature:
- Fungal, viral and traumatic stomatitis in a therapeutic dentistry clinic. Tutorial. Edited by Dr.Med.Sc. K.G. Karakova - Stavropol. Publishing and information, 2013. – 100 p.
- Pankrusheva T.A., Maravina I.N., Chekmareva M.S. Research on the development of the composition and technology of tablets for the treatment of stomatitis // Scientific result. Medicine and pharmacy. – T.4, No. 1, 2022, pp. 78-88.
- Tilis S.Yu. Stomatitis. Nurse, 2010, No. 2.
- Glukhmanyuk D.S., Malinovsky V.A. Aphthous stomatitis. Proceedings of the scientific and practical conference “Modern problems of pharmacology, cosmetology and aromology.” International Humanitarian University, Odessa Medical Institute, 2015. (Current problems of pharmacology, cosmetology and aromology: Materials of the scientific and practical conference dedicated to the 160th birthday of a prominent Ukrainian pathologist, endocrinologist, immunologist , microbiologist, professor Volodymyr Valerianovich Pidvysotsky and Pharmacist Day. m. Odessa, June 15, 2022 – Odessa: International Humanitarian University, 2015. – 48 p.)
- Volkova, M.N. Diseases of the oral mucosa: educational and methodological manual / M.N. Volkova, Yu.P. Chernyavsky, N.A. Sakharuk, Yu.R. Elenskaya. – Vitebsk: VSMU, 2016. – 236 p.
- Therapeutic dentistry: textbook: in 3 hours / ed. G.M. Barera. - M. : GEOTAR-Media, 2005. - Part 3. - 288 p.
- Galizina O.A. Main aspects of the occurrence, clinical manifestations, treatment and prevention of chronic recurrent aphthous stomatitis. Russian Dental Journal, 2014, No. 6, pp. 39-43.
- Instructions for the medical use of the drug Metrogyl Denta® Dental gel // Registration number P N015982/01 // State Register of the Russian Federation. – URL: https://grls.rosminzdrav.ru/Grls_View_v2.aspx?routingGuid=9bc9a05c-d28b-…
- Dental gel for gums Metrogyl Denta® in the treatment of periodontal diseases and oral mucosa. Practical medicine, No. 1(33), March, 2009, pp. 105-106.
- Strakhova S.Yu., Drobotko L.N. Chronic recurrent aphthous stomatitis (lecture). RMZh, No. 29 from December 27, 2006, p. 2096