Severe periodontitis
At this stage, the treatment of periodontitis is no longer limited to conservative measures; here it is necessary to resort to surgical methods of treatment - removal of the most damaged teeth, open curettage, and flap operations.
In addition, in case of severe periodontitis, targeted regeneration (building) of bone tissue is used with the help of osteogenic preparations, membranes, etc., which strengthen and compact the bone and create the prerequisites for its restoration where possible.
Causes of periodontitis.
Inflammatory processes, known as periodontitis and gingivitis, occur in periodontal tissues and are interrelated forms of the same disease. Their main difference is in localization. Pathologically, the process can be inflammatory or dystrophic in nature.
Gingivitis (early stage of periodontitis) is an inflammation of the gums (the process affects only the tissues of the gingival margin, while affecting only the upper gum tissues) without compromising the integrity of the periodontal junction.
Risk factors: tobacco smoking; poor oral hygiene; acute lack of vitamins and minerals; problematic fillings; nasal breathing disorder.
Main symptoms: redness and swelling of the gums; the appearance of soft and hard deposits on teeth; bleeding gums when brushing teeth; weakened immunity.
As for periodontitis, it affects all periodontal structures. It is characterized by chronic inflammation of the gums and destructive changes - destruction of the periodontium and bone tissue of the alveolar process. The dentogingival attachment is disrupted, periodontal pockets are formed and, in the future (with an active course), due to the rapid destruction of the alveolar processes, teeth fall out.
The rate of spread of periodontitis is greater, the more numerous the risk factors are: immunosuppressive conditions; there are deviations in the development of the dental system (occlusion pathology); any diseases of internal organs have been diagnosed.
Features of the chronic form of generalized periodontitis
Any other oral disease can be a provoking factor in the development of the disease. Gingivitis, neglect of personal hygiene rules, mechanical damage - all these are obvious reasons for the development of a chronic form of pathology. It occurs in two stages:
- exacerbation, accompanied by throbbing pain in the gums, excessive bleeding, pus discharge, abscesses, fever, inflammation of the lymph nodes (such symptoms often make themselves felt against the background of pneumonia, stressful situations, ARVI);
- remission, which occurs during therapeutic measures; during this time, symptoms do not appear, and nothing bothers the patient.
The further the pathology develops, the longer the exacerbation lasts, and the time of remission gradually decreases.
Classification of periodontitis.
The course of the disease, area of distribution and severity - these are the classification criteria.
According to the course of periodontitis there are:
- Spicy;
- Chronic;
- Periodontitis with abscess formation.
Periodontitis in the area of distribution can be local (focal) - individual parts of the periodontium are affected, and generalized (diffuse) - diffuse damage to the periodontal complex. The pathological process involves all periodontal tissues of one tooth, a group or all teeth: gums, circular ligament of the tooth, periodontal tissue, bone tissue (compact and spongy substance), the vascular system of these formations and the dental pulp.
According to its manifestation, periodontitis can be mild, moderate and severe.
The most important clinical sign of periodontitis is the presence of a periodontal pocket of varying depth (this can be used to judge the degree of damage).
The stronger the inflammation, the greater the pathological mobility of teeth becomes. As a rule, mobility is accompanied by the appearance of gaps between teeth and the overlap of one tooth over another. When determining the severity of periodontitis, the specialist evaluates the position of each tooth in the dental arch.
The degree of periodontal atrophy and the functional value of teeth underlie the choice of treatment for periodontitis.
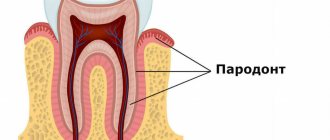
What is periodontium, its features
In dental practice, the term “periodontium” is used. It includes a whole complex of tissues surrounding the teeth. They all have a common nerve origin and a single blood supply, therefore they are closely related to each other. The periodontium forms several constituent elements: gums, bone tissue, periodontium, cement of the root system of the teeth. Its functions include providing support, maintenance, and protection of the entire dental system. Pathologies associated with periodontal damage include conditions such as gingivitis, periodontal disease, tumors, and periodontitis.
Treatment of periodontitis.
Removal of dental plaque and professional teeth cleaning in combination with medications (massages, lotions and rinses) - this is the treatment at the initial stage of periodontitis.
More severe periodontitis requires surgical intervention (to remove deep deposits of tartar, specialists perform curettage, bone tissue augmentation, splinting, implantation) and drug treatment. Anti-inflammatory and antiseptic drugs are used (they are also injected into periodontal pockets). There are non-steroidal anti-inflammatory drugs in the form of gels and pastes, which greatly facilitates their administration; in addition, tissue regeneration stimulants are often used, which are applied topically. In the complex therapy of periodontitis, vitamins are prescribed that strengthen the vascular walls.
Rational treatment and systematic hygienic oral care can achieve remission.
In the treatment of periodontitis, physiotherapy is successfully used: electrophoresis with painkillers and vitamin preparations, laser radiation, fluctuarization (therapeutic currents of medium frequency), darsonvalization (pulse currents). The latest modern methods of treating periodontitis, such as ultrasound and laser beams, are also widely used in dental practice. The laser beam painlessly removes tissue affected by inflammation and closes not too deep periodontal pockets. Ultrasound is an excellent way to get rid of pathogenic microflora accumulated in gum pockets.
It is strictly necessary to visit a doctor for consultation; he will determine the symptoms and prescribe treatment for periodontitis. Preventing periodontitis and regularly visiting the dentist is the best way to maintain oral health.
Directions of therapy for mild periodontitis
The chronic form of mild periodontitis is treated in stages, here is an approximate diagram.
- First, plaque and deposits formed on the tooth enamel are removed.
- Subsequently, the doctor prescribes topical antibacterial agents. They need to be applied in the form of applications to the affected areas. An important role is played by rinsing the mouth with solutions containing antiseptic components.
- The key to successful therapy is compliance with hygiene procedures (purchase and use of special healing pastes, professional toothbrushes, dental floss).
By providing thorough daily oral care and learning to visit the dentist regularly, you can avoid this sore and prevent worsening if it progresses.
Periodontal measures for moderate disease
If the disease has become moderately severe, selective therapy is added to the above measures. It is aimed at grinding the surface of teeth that have undergone occlusion, removing deposits under the gums, applying therapeutic dressings and compresses. Along with this, questions are being resolved about whether it makes sense to remove roots or individual teeth, and whether it is worth carrying out splinting and orthopedic therapy. Local anti-inflammatory procedures are usually complemented by general therapy.
Forecast and preventive measures
If treatment is started in the early stages of the pathology, this leads to remission and the possibility of its extension. In restoration measures and in the process of preserving tissue functions, compliance with recommendations related to the implementation of preventive measures plays an important role. If the disease is advanced, the prognosis is unfavorable. This may be due not only to the loss of almost all teeth, but also to the fact that severe systemic complications will begin to develop, especially in the cardiovascular system.
The preventive complex involves compliance with a number of care and hygiene measures:
- timely brushing of teeth;
- a competent choice of cleaning products and tools - toothpastes, powders, brushes, threads;
- regular implementation of professional hygiene;
- timely treatment of emerging diseases;
- removal of deposits from the teeth;
- carrying out treatment of concomitant pathologies.
With these simple measures you can prevent illness and feel great.
Thus, generalized periodontitis is a serious disease that tends to constantly develop and progress. In this regard, it is necessary to diagnose it in a timely manner and take therapeutic measures. This approach will prevent complications and keep all teeth normal, eliminating unpleasant symptoms and improving the patient’s well-being.
Laser gingivotomy - surgical treatment of complex forms of periodontitis
Laser gingivectomy in the area of one tooth
Catarrhal and hypertrophic gingivitis symptoms and treatment in adults
Open and closed curettage of periodontal pockets
The roots of the teeth are exposed - what to do and how to treat them
Splinting teeth for periodontitis with fiberglass and tape
Stages
During the course of the disease, there are three main stages, which differ in the nature and severity of symptoms. These are the next stages.
- First. Periodontal pockets are still shallow - up to 3 mm. Periodically, after brushing, bleeding gums are noted. It is not accompanied by pain or loosening of teeth.
- Second. The depth of the pockets increases to 5 mm, due to which the neck of the tooth is partially exposed. Hypersensitivity also occurs when eating hot or cold foods.
- Third. This stage, with a non-aggressive course of the disease, develops approximately 4-5 years after the onset of inflammation. In severe cases, the dental pockets deepen up to 6 mm. Food debris accumulates in them, which leads to suppuration. This causes the teeth to become very loose.
What to do to avoid complications
To avoid complications, it is necessary to recognize the disease in the early stages and take measures for adequate treatment. All this will allow you to achieve stable and long-term remission and preserve the functions of your teeth and gums. In order for the dental system to be healthy, it is necessary not only to observe the rules of personal hygiene, carrying out regular care procedures, but also to periodically visit a specialist who will perform professional cleaning in order to remove minor dental deposits.
General symptoms of the disease
In the initial stages, the patient suffers from severe bleeding gums. They become loose and swollen. The patient feels itching, throbbing, severe burning, pain when he chews food. An unpleasant odor begins to emanate from the mouth. Dental pockets at this stage are shallow, they are located mainly in the interdental spaces. At the initial stages, the teeth are motionless and not displaced anywhere. The patient's general condition is normal.
The clinical picture of the developing disease is somewhat different. In addition to the above symptoms, the patient may experience:
- displacement of teeth and their loosening;
- high sensitivity of teeth to external irritants (temperature fluctuations);
- problems chewing food;
- disturbance of general well-being (typical of severe forms of pathology), accompanied by weakness, malaise, and increased body temperature;
- an increase in the size of regional lymph nodes, which in addition become painful;
- during a dental examination, the doctor observes signs of diffuse gingivitis;
- Plaque and deposits accumulate abundantly on the teeth;
- tooth loss, fistula, abscesses (signs are characteristic of advanced stages of the disease).
In the case of a chronic form of the disease, the gums have a pale pink tint. There are no dental deposits, manifestations of pus or blood. There is a possibility of exposure of the roots of the teeth. X-ray does not show signs of bone resorption.