Indications for removal
The dentist decides whether or not to remove a tooth, adequately assessing the situation in the mouth.
Direct indications are:
- advanced caries that cannot be treated;
- lack of a crown, with roots not suitable for implantation;
- crown fracture exposing the pulp;
- the dental unit is a source of infection, as a result of which complications develop (tonsillitis, periostitis, sinusitis, osteomyelitis of the jaw, abscess and phlegmon of the cheek);
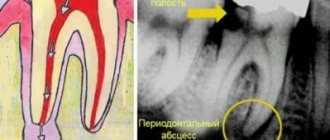
- unsuccessful treatment of periodontitis;
- unerupted or incompletely erupted teeth are the cause of frequent inflammation, damage to nearby tissues and teeth;
- severe mobility with an extreme degree of periodontal damage that cannot be treated;
- purulent periodontitis, which is not relieved by conservative methods;
- crowding of teeth.
Atraumatic removal of third molars
Damage to the inferior alveolar and lingual nerves are fairly common complications during extraction of mandibular third molars. However, improved diagnostic approaches and surgical treatments are helping to significantly reduce the incidence of such adverse outcomes. Below is a description of diagnostic and therapeutic techniques aimed at preventing surgical complications during extraction of lower third molars.
Tools and Methodology
When removing an impacted wisdom tooth in the lower jaw, it is extremely important to prevent damage to surrounding anatomical structures such as the inferior alveolar and lingual nerves, as well as periodontal tissues of the second molar. Therefore, the surgical instruments used are of utmost importance. In the presented case, an innovative mechanical periotome Luxator LX (Directa Dental) was used, which directly carried out the extraction procedure. The instrument allows you to cut the Sharpey fibers passing between the root cementum and the alveolar bone, and thereby free the tooth from the periodontal ligament.
Clinical case
A 22-year-old somatically healthy patient sought dental care for pain in the area of the 17th tooth, which spread to the entire lower jaw. The orthopantomogram visualized compression of the mandibular nerve, which was in contact with the roots of the 17th tooth (photo 1).
Photo 1. Orthopantomogram before treatment.
An intraoral examination revealed swelling and redness of the mucous membrane distal to the 18th tooth. There were no sensory disturbances in the lower jaw. The repeat image revealed that the position of the nerve was too close to the distal-lingual root of the tooth, which was also confirmed on CT sections (photos 2 - 3).
Photo 2. CT slices helped evaluate the course of the inferior alveolar nerve.
Photo 3. Localization of the nerve relative to the root based on CT data.
After performing anesthesia with a 2% vasoconstrictor, a single flap was formed, along which an intrasulcular incision was made around the 18th tooth. The releasing distal incision was made at an angle of 45º to the second molar, and at first this incision had a full tissue depth, and at the end it only partially penetrated the tissue. This incision avoids the risk of cutting the lingual nerve and serves as a connector for the flap. After exposing the jaw bone and installing a tongue guard, the Sharpey fibers were cut using a Luxator LX mechanical periotome around the entire circumference of the tooth, freeing it from the periodontal ligament (photos 4 - 5).
Photo 4. Extraction procedure using Luxator LX 360°.
Photo 5. Extraction procedure using Luxator LX 360°.
The tooth was extracted using an elevator without luxation of surrounding tissues or damage to the mandibular nerve. Through a controlled reciprocating motion, Luxator LX penetrates the periodontal ligament space (0.15 mm to 0.38 mm) and separates the fiber bundles from the tooth surface in the least traumatic way. This approach also minimizes the risk of damage to the nerve structures of the jaw. Photo 6 shows an x-ray that demonstrates how the working part of the instrument penetrates into the space of the tooth socket. Photo 7 shows the absence of root remains. The extraction procedure was carried out without segmentation of parts of the molar, so the latter was extracted in its entirety (photo 8).
Figure 6: Visualization of the Luxator LX inside the socket on a radiograph.
Photo 7. X-ray control: absence of root fragments in the hole.
Photo 8. Extracted tooth.
The alveolus was cleaned, irrigated with cold saline, and sutured with 4/0 silk thread. The sutures were removed 7 days after the iatrogenic intervention. The patient reported that the wound was healing without significant pain symptoms, which could be relieved with simple painkillers. The patient was advised to use an innovative gel toothpaste with a mixture of humectant and antibacterial agents (eg, cetylpyridinium chloride, triclosan and essential oils), which helps reduce the risk of plaque formation and reduce signs of bleeding. The level of abrasiveness of this paste was also slightly lower than that of conventional paste. The dental hygienist will further assist the patient in maintaining an optimal level of hygiene, as this is essential to ensure adequate healing. The procedure for professional oral hygiene was recommended to be carried out using glycine powder, which does not irritate the gums (Air Flow, EMS). Since the rough surface of teeth is more susceptible to the formation of bacterial plaque, polishing is an essential step in hygienic cleaning of the oral cavity. Silica-based polishing pastes with a low RDA value, such as ProphyPaste CCS Yellow RDA 40 (Directa Dental), can be used for this purpose.
conclusions
Extraction of the third molars of the mandible is directly associated with the risk of damage to the nervous structures of a temporary and permanent nature. Such complications can even provoke legal problems, so before starting treatment, the doctor must conduct a comprehensive diagnosis of the clinical situation, taking into account all aggravating factors (including the degree of wisdom tooth retention). The surgical approach used allows us to minimize tissue trauma and reduce the risk of damage to nearby nerves. Luxator LX is an effective tool that facilitates efficient molar extraction, significantly reducing the invasiveness of the surgical procedure and subsequent postoperative discomfort.
Authors: Loris Prosper Nicolas Zunica
Contraindications
- acute diseases of the cardiovascular system;
- high blood pressure numbers;
- infectious processes in the body;
- menstruation period in women, since blood clotting time is increased, which threatens bleeding after extraction;
- acute, severe diseases of the central nervous system;
- pregnancy, lactation period;
- purulent-septic processes in the oral cavity, which provokes sepsis; mental disorders.
The possibility of extracting a diseased tooth appears after treatment of these pathologies and stabilization of the patient’s condition. In case of an emergency, the doctor performs removal in a patient with concomitant diseases. Severe pain syndrome is the cause of exacerbation of chronic pathology.
In what cases is removal of the upper tooth inevitable?
Medical indications for extraction of the upper tooth can be divided into planned and emergency. The planned ones include:
- periodontal inflammation or the formation of a cyst at the roots of a tooth with impenetrable roots;
- tumors of the upper jaw;
- the presence of unerupted, out of place or extra teeth that cause discomfort (damaging soft tissues, causing speech defects, preventing normal chewing of food, increasing the risk of developing inflammatory processes);
- destruction of the crown that cannot be restored;
- periodontal inflammation, one of the signs of which is pathological tooth mobility;
- fractures of tooth roots;
- the presence of teeth that interfere with orthopedic or orthodontic treatment.
Emergency indications are:
- purulent inflammation of the bone tissue of the upper jaw, occurring in an acute form;
- destruction of the crown of a tooth that has no functional value.
In addition, severe toothaches that cannot be eliminated by conservative methods (for example, in case of complex crown fractures) can be the basis for unscheduled extraction.
Removal techniques
The dental surgeon determines the extraction tactics individually for each patient. Takes into account the location of the tooth, the type of pathological process, and the degree of spread. Before extraction, the doctor sends the patient for an x-ray. The goal is to obtain accurate information about the roots and structural features of adjacent teeth and the jaw apparatus in which the pathological unit is located.
Simple operation
In the case of a conventional location, removal occurs in a simple way, which takes no more than 10 minutes, taking into account the effect of anesthesia. The dental surgeon performs the operation according to the following scheme:
- a preliminary survey of the patient about allergies to anesthesia drugs, chronic pathologies and the medications he uses;
- administration of a drug for superficial sedation in order to normalize the mental state and ensure a comfortable extraction process (at the request of the patient or according to indications);
- injection of a local anesthetic into nearby tooth tissues (gums, cheek), usually using ultracaine, which is considered hypoallergenic;
- after 4-5 minutes, the surgeon begins the removal process by loosening the tooth in the surrounding tissues;
- after ensuring mobility, the specialist separates the tooth from the gum and with a sharp movement turns it out of the alveolar socket;
- the wound is treated with an antiseptic solution;
- a tampon with a medicinal substance is applied to the wound, after which the bleeding stops for several minutes;
- if after tooth extraction the wound surface is too large, the doctor will apply several stitches, which will prevent the possibility of postoperative infection and bleeding in the future;
- the patient receives recommendations and goes home after stabilizing his physical and emotional condition.
After removal using a simple method, the patient feels well. If the wound bothers you after the anesthesia wears off, it can be easily eliminated by following your doctor's recommendations.
The hard way
When the doctor sees abnormalities on the x-ray, removal will be carried out in a complex way. The experience and skill of the doctor matters.
Stages in complex removal:
- taking anamnesis;
- choice of anesthesia;
- mandatory administration of sedatives to relieve tension in the patient;
- injection of local anesthesia into 5-6 areas surrounding the tooth to be removed;
- the doctor makes an incision in the gum to access the tooth and roots;
- drilling into several parts using a drill for easy removal and prevention of injury;
- the tooth is separated from the gum in parts and removed;
- a mandatory revision of the resulting hole is performed;
- the wound is treated with an antiseptic and sutured;
- To prevent infection and bleeding, the doctor places a drug or PRP membrane in the wound. They dissolve along with the sutures.
Extraction during the normal course of the process takes 20-30 minutes. If the operation is complicated, the procedure may take up to 2 hours. After a complex removal, the wound is wider, the tissue is more traumatized, the pain is more pronounced and lasts longer.
It is important that removal is carried out carefully, taking into account future implantation. Therefore, it is better to entrust the operation to an experienced maxillofacial surgeon who will not damage the alveolar ridge. In this case, you will not have to build up bone tissue before installing the implant and eliminate possible complications. Average surgeons usually do not stand on ceremony during operations. The result is broken bone structures of the jaw, wandering remnants of roots, unremoved cysts growing into the maxillary sinus, perforations, fistulas, osteomyelitis and much more. Not to mention the shocking post-operative pain that overtakes the patient after such punitive surgery. Only the maxillofacial surgeon has enough theoretical and practical skills to perform tooth extraction without complications.
Molar tooth extraction in children
Unfortunately, young children often develop diseases in both their primary and permanent molars. Worse, it is not always possible to heal them. Dentists remove permanent teeth for children only when there is no way to save them.
Primary molars are both treated and removed. If a permanent tooth begins to grow under a baby molar, then the baby tooth is always removed, since it interferes with the normal formation of the permanent tooth.
At the same time, dentists never agree to premature removal of baby molars. Such teeth are sure to heal. If you remove a baby tooth ahead of schedule, then the baby will develop a crooked bite.
There are situations when a child’s molar tooth must be removed. Such situations include:
- molar root cyst;
- presence of granuloma;
- inflammation of the tooth root;
- inflammation of the nerve of the lower jaw;
- severe destruction of the integrity of the tooth.
Price
The cost depends on the technology used:
| Name of service | Price |
| Easy removal | 13,500 rub. |
| Difficult removal | 23,000 rub. |
The case includes:
- anesthesia;
- operation;
- removal and application of sutures.
Additional services:
| Name of service | Price |
| Sedation (per hour) | 12,000 rub. |
| Consultation with existing x-ray examination | 2,000 rub. |
| Consultation and X-ray diagnostics (CT scan in our Center on disk) | 5,200 rub. |
| Sight shot | 500 rub. |
Features of tooth extraction in the upper jaw
Unlike lower “eights,” upper wisdom teeth are considered less problematic. They tend to grow straighter, have less retention, and rarely have roots that are bent, twisted, or excessively long. The bone of the upper jaw is not so massive and dense, there are fewer blood vessels in the soft tissues, and the likelihood of hitting the trigeminal nerve is lower. Therefore, the upper wisdom teeth rarely have to be removed, and if it comes to surgery, it is easier than removing the lower wisdom tooth.
Recommendations after surgery
- Do not eat or drink water for 6-7 hours after surgery;
- reduce physical activity, avoid visiting saunas and swimming pools for 4-5 weeks to prevent the development of bleeding;
- take analgesics to relieve pain in the early period;
- regularly take antibiotics prescribed for a course of 7 days;
- rinse your mouth with an antiseptic solution after eating;
- follow a gentle diet, avoid solid and irritating foods;
- stop smoking - nicotine provokes bleeding.
Following the doctor's recommendations reduces wound healing time and prevents the development of complications.
Is it painful to remove an upper wisdom tooth?
Based on patient reviews, we can conclude that what scares them most about the operation of removing the upper “eights” is pain. But you shouldn’t be afraid of it: modern anesthetics completely block unpleasant sensations. Even if one of the drugs did not provide high-quality pain relief, the doctor will always be able to choose another one. There is no need to endure pain during wisdom teeth removal!
Most often, patients complain of pain not during, but after surgery. This is quite predictable: the anesthesia wears off and the body “remembers” the wound in the mouth. To relieve pain during the rehabilitation period, the doctor prescribes painkillers to the patient. With a simple removal of a wisdom tooth from above, 1-2 appointments may be enough, but after a complex operation, you will have to take pills for several days.
How long does it take for a wound to heal?
Normally, the wound surface heals in 4-5 weeks. In older patients, healing is delayed due to decreased tissue repair and reduced blood circulation.
The rate of healing depends on the extent of the procedure and the roots. In the case of complex removal of a molar with 3-4 roots, the process of tissue regeneration is delayed up to 20-25 days.
Restoration of gum tissue goes through the following stages:
- in the first days, the wound is closed by a blood clot (thrombus), formed as a result of stopping the bleeding;
- 3-4 days after removal, the thrombus resolves, and new tissue appears on the surface of the wound in the form of a thin film;
- bone tissue forms on the sides of the socket already at 3 weeks;
- after 3-6 months, the hole heals and has no differences with the jaw bone.
The speed of wound healing after removal depends on the characteristics of the body and the age of the patient. If necessary, the doctor corrects the tissue regeneration process with medications and physiotherapeutic methods.
Why you shouldn’t refuse tooth extraction
Our reluctance to part with healthy teeth is legitimate and understandable. But an orthodontist drawing up a treatment plan cannot be guided solely by the patient’s wishes. The doctor focuses on the goal set for him and uses optimal methods that correspond to the real state of affairs to achieve it.
The need for removal is always carefully considered, because treatment with removal takes a lot of time, and for the dentist it also results in a larger amount of work and much greater responsibility. It is also necessary to understand that to make a decision on removal, the doctor does not need only a TRG image (teleradiogram). A treatment plan will be drawn up after obtaining a clear understanding of the patient's jaw anatomy to ensure that their facial contours are maintained after realignment.
Types of operations
Tooth extraction from above is carried out using various tools and techniques, depending on the position of the unit and the condition:
- Incisors and canines. For the front teeth, straight forceps are used, the doctor makes dislocation, rotational movements. Luxation and rotation movements are used for posterior teeth and canines.
- Premolars and molars are removed using S-shaped forceps. For premolars, luxation movements are first made, the first being in the direction of the cheek. For molars, in some cases special forceps with spikes are indicated. Luxation movements - towards the sky or outwards.
- To remove the “eights”, bayonet forceps or straight elevators are used; to remove the roots, you can use S-shaped tools or forceps with converging cheeks.
About the removal of premolars (end)
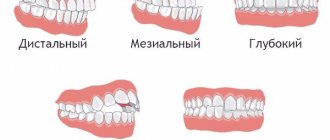
When else do we like to remove premolars? Remember? Yes for distal occlusion . When the upper teeth protrude (stick out) forward unattractively.
And instead of bothering to find the cause of protruding teeth at the skeletal (jaw size problem) or cranial (jaw position problem) levels (and the reason most often lies there) - we simply remove the upper teeth (usually premolars), close the gaps, trying to dock upper teeth with lower teeth in the anteroposterior direction (sagittal plane). In essence, we are trying to solve “non-dental” problems at the expense of teeth (reducing their number). And we often get the problems described above. And sometimes we don’t even think that the treatment is inadequate and does not correspond to the cause. Moreover, we are aggravating this reason.
By the way, when treating distal occlusion by removing premolars, there is another mechanism for causing troubles and complications. It is no secret that most often the cause of distal occlusion is a more posterior than normal position of the lower jaw. With all the consequences... And accompanying... Deep bite. Beveled profile. Reduced height of the lower third of the face. The TMJ (temporomandibular joint) is in compression, because the head of the condyle is displaced distally (backward). What contributes to the development of degenerative changes in the TMJ.
And TMJ (or rather its dysfunction ) is in itself a wide field for various kinds of non-dental clinical manifestations. What is it... For dysfunctions of the temporomandibular joints (TMD), the clinic is often more psycho-neurological than dental. And there is a reason for this: compression (squeezing) of the joint elements, muscle spasm, which always accompanies distal occlusion and TMD, lead to improper redistribution of blood pressure in the skull, tension of the dura mater, and irritation of nerve endings. This is what causes headaches , tinnitus , panic attacks ... And many other “interesting” things. But this will be a separate conversation. It's a very serious topic.
And all because the entire lower jaw, I repeat, is positioned posteriorly from the norm. And very often this incorrect posterior position is caused (and accompanied) by the also distally located upper jaw . Or underdevelopment of the upper jaw in that same premaxillary zone, and therefore its (upper jaw) shortening. And instead of bringing the lower jaw forward, decompressing the TMJ, and unloading the joint to relieve the symptoms of dysfunction (and often this is pain!!!), we are trying to solve this problem at the level of the teeth.
And how do we decide? By removing. And by removing premolars, we get all the problems listed above (in the previous part of the article).
In addition, by reducing the length of the already short upper jaw, we simply “perpetuate” the distal position of the lower jaw. And thus we simply “bury” the temporomandibular joint . And we play into the hands of the further development and consolidation, already at the skeletal and dental levels, of that same dysfunction with all its symptoms. Such a vicious and vicious circle...
Regarding the small value of premolars in a functional aspect... There is also something to argue about.
Which teeth make the first contact when closing the mouth? Which teeth perform the chewing movement first? Yes, exactly premolars. And these are very (and very) functionally important teeth. And their location in the jaw is a very (and very) sensitive area for all kinds of skeletal and cranial distortions.
CONCLUSION: There are still indications for treatment with the removal of premolars . Do not deny. But! They are so narrow. So specific. And they are so rare. That we won't even discuss them. These indications can be classified as exceptions. And exceptions, as we know, only confirm the rules. Therefore, treatment with the removal of premolars cannot in any way be a common, routine, widespread and everyday practice. And the patient needs to be very careful in carrying out treatment with the removal of premolars. And doctors should diagnose patients more carefully. And more thoughtfully analyze the consequences of such treatment. And then the number of patients with various kinds of pain syndromes, distorted faces (sometimes literally), and simply patients dissatisfied with the treatment you provided, will noticeably decrease.
READ MORE: “About alternatives to treatment with removal.”
Sign up for diagnostics
Social Like
Comments for the site
Cackl e
Indications and contraindications
Indications for removal are:
- tooth root fractures;
- severe destruction;
- chronic form of periodontitis;
- atypical structure, inclusion or dystonia, leading to pathologies (difficulty opening the mouth, diction disorders, etc.);
- advanced caries;
- strong mobility;
- crowded teeth;
- neoplasm on soft tissues near the root, large cysts.
Contraindications:
- canine removal (treatment recommended);
- pregnancy;
- mental disorders;
- traumatic brain injuries;
- epileptic seizures;
- diabetes;
- diseases of the nervous and respiratory systems.
Before removal, the doctor conducts a thorough examination, determines whether the tooth can be saved and what measures need to be taken to achieve this. In most cases, doctors prefer treatment, as this allows the functionality of the row and aesthetics to be preserved.
Recovery period
How long does recovery take after removal of upper wisdom teeth and what limitations does it impose? In most cases, after 1-2 days the patient returns to normal life, but sometimes recovery takes longer. To prevent the rehabilitation period from being prolonged, it is very important to follow the doctor’s recommendations:
- take prescribed antibiotics, painkillers and anti-inflammatory drugs;
- do not visit the bathhouse, sauna, swimming pool, or take a bath;
- follow a diet, if possible, eat only soft foods;
- refrain from smoking.
If the doctor did not make mistakes during removal, and the patient carefully followed all the doctor’s recommendations, then the recovery period will pass quickly, and the problem of the upper “eights” can be forgotten forever.