Description
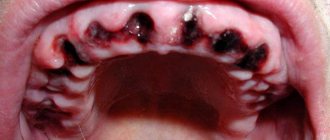
Tooth extraction is accompanied by bleeding, which most often stops after a few minutes with the formation of a blood clot. However, in some cases it does not stop on its own and continues for a long time - primary bleeding. Sometimes bleeding appears some time after the operation (several hours or even days later - secondary bleeding. Prolonged bleeding is most often caused by local causes, less often by general ones.
ICD code for alveolar bleeding
After tooth extraction (ICD 10 code: K08.1), the alveoli are naturally filled with a blood clot formed as a result of bleeding from a rupture of the dental artery, the network of arterioles and capillaries of the periodontium and gums. This bleeding is capillary and parenchymal in nature, usually occurs after tooth extraction and stops after a few minutes (from 5 to 20 minutes). The pressure of the gauze pad used to cover the wound helps to stop bleeding more quickly. Rinsing your mouth after tooth extraction prevents bleeding from stopping.
In some cases, bleeding in the area of the extracted tooth socket does not stop or stops and reappears after a few hours or even days. Typically, most bleeding after tooth extraction is caused by local causes: deep rupture and crushing of the gums, the presence of an inflammatory process, paralysis of the vascular walls after the use of adrenaline. Secondary bleeding associated with infection of the socket and disintegration of the blood clot are also observed.
In more rare cases, such bleeding is caused by general causes associated with blood clotting disorders (hemorrhagic diathesis and diseases with hemorrhagic symptoms). In most cases, bleeding after tooth extraction, due to reasons of both local and general nature, can be stopped using the generally accepted method - tamponade of the hole with iodoform gauze. Tamponade of the hole with iodoform gauze to stop bleeding must be done very carefully. To do this, blood clots are removed from the patient’s mouth and the bleeding hole is dried with a gauze swab in order to determine upon examination where the bleeding is coming from - from the alveoli or from the gums.
When bleeding from torn edges of the gums, after applying a hemostatic clamp to the gingival edge, it is enough to sew the gingival edges, trim or bandage the bleeding vessel. If bleeding occurs from the bone septum, then the bleeding area is compressed by squeezing the bone with bayonet-shaped forceps with non-converging cheeks. After this, the hole is tamponed.
ETIOLOGY AND PATHOGENESIS
The cause of bleeding from the tooth socket is tissue trauma, rupture of blood vessels (dental artery, arterioles and capillaries of the periodontium and gums) during operations in the maxillofacial area, most often tooth extraction or trauma. After a few minutes, blood clotting in the hole occurs and bleeding stops. However, some patients experience disruption of clot formation in the socket, which leads to prolonged bleeding. More often this is due to significant damage to the gums, alveoli, oral mucosa, pathological processes in the maxillofacial area (trauma, bacterial inflammation), less often - the presence of concomitant systemic diseases in the patient (hemorrhagic diathesis, acute leukemia, infectious hepatitis, arterial hypertension, diabetes mellitus). diabetes, etc.), taking drugs that affect hemostasis and reduce blood clotting (NSAIDs, antiplatelet agents, anticoagulants, fibrinolytic drugs, oral contraceptives, etc.).
With prolonged bleeding, the patient's condition worsens, weakness, dizziness, pale skin, acrocyanosis, decreased blood pressure and a reflex increase in heart rate appear.
If the patient was administered a local anesthetic drug with epinephrine, which has a vasoconstrictor effect, when its concentration in the tissues decreases, the vessels dilate and stopped bleeding can resume, i.e. Early secondary bleeding may occur. Late secondary bleeding occurs after several hours or days.
Titles
Post-extraction bleeding.
Classification, features of the course of the disease
Pathology is classified into primary and secondary bleeding. The first group is bleeding that developed immediately after tooth extraction, secondary bleeding - after some time. Approximately 65-94% of all cases occur in the secondary group, which is divided into early and secondary late types.
Externally, bleeding is manifested by the following signs:
- the blood from the hole does not stop, it can pulsate;
- feeling unwell;
- pressure is reduced;
- dizziness appears;
- rapid pulse;
- the skin becomes pale in color.
Classification, features of the course of the disease
Pathology is classified into primary and secondary bleeding. The first group is bleeding that developed immediately after tooth extraction, secondary bleeding - after some time. Approximately 65-94% of all cases occur in the secondary group, which is divided into early and secondary late types.
Externally, bleeding is manifested by the following signs:
- the blood from the hole does not stop, it can pulsate;
- feeling unwell;
- pressure is reduced;
- dizziness appears;
- rapid pulse;
- the skin becomes pale in color.
Causes
Local causes of alveolar bleeding: damage (rupture, crushing) of soft tissue and bone vessels during traumatic surgery; fracture of the alveolar wall or interradicular septum; the presence of an intraosseous vascular tumor; during an acute inflammatory process (inflammatory hyperemia), in the second phase of the action of vasostrictors (vasoparesis), during purulent melting of a blood clot and thrombi in the vessels during alveolitis. Common causes of prolonged post-extraction bleeding are due to a violation of the blood clotting process or a violation of the vascular system. These include hemorrhagic diathesis: hemophilia, thrombocytopenic purpura (Werlhof's disease), hemorrhagic vasculitis, hemorrhagic angiomatosis (Rendu-Opeler disease), angiohemophilia (Villebran disease), C-vitaminosis, diseases accompanied by hemorrhagic symptoms: acute leukemia, infectious hepatitis, septic endocarditis, typhus and typhoid fever, scarlet fever and; in patients receiving anticoagulants, in patients suffering from hypertension.
Local factors
- Ruptures or injury to soft tissues. These are the most common causes of alveolar hemorrhages.
- Destruction of a blood clot formed in the socket. This can be caused by the actions of the patient himself, for example, active rinsing of the mouth, and alveolitis that develops as a result of infection of the socket.
- Damage (fracture) of the alveoli or bone septum located between the teeth.
- Opened vascular tumor in the area of the extracted tooth.
- Inflammatory process in periodontal tissues of various etiologies.
This is interesting: The importance of the drug Kollapan for modern dentistry
High blood pressure
A patient with hypertensive pathology often experiences bleeding from the socket, so if he has such a disease, he should inform the doctor about it before the operation. This will allow you to find an individual approach to a problem patient and prevent possible complications.
Poor blood clotting
If the patient has previously been diagnosed with coagulation disorders, then he is obliged to inform the doctor about the existing problems in order to prevent negative consequences.
Inflammation of the socket
After surgery, the doctor must treat the hole with an antiseptic. But even treatment is not always a guarantee that the bleeding will stop after wisdom teeth are removed. If the socket is a source of infection, the gums usually bleed. In such cases, you should not resort to self-medication, as this can lead to dire consequences. Only a professional specialist can correctly diagnose and prescribe effective treatment.
Purulent accumulations
Before performing any manipulation, the dentist must diagnose the patient’s jaw and make sure there are no pathologies. If there are already purulent accumulations inside the gums, this can provoke heavy bleeding, which is quite difficult to stop.
Damage to the integrity of blood vessels
Due to the irregular growth and location of wisdom teeth in hard-to-reach areas of the oral cavity, the removal of such units is considered a relatively complex dental procedure. Vessels are almost always damaged by surgical instruments. Usually, after several hours, the bleeding stops, but the patient may simply not feel pain due to prolonged exposure to the anesthetic. If large vessels are damaged during surgery, bleeding may occur later and in such cases you should not hesitate to visit the dentist.
Failure to comply with medical recommendations
A rather complex procedure is the removal of a wisdom tooth; bleeding can occur in every patient, even if the operation is performed correctly. The reason for this is improper wound care, which leads to a deterioration in the condition of the hole and the development of an inflammatory process.
General factors
Systemic factors causing alveolar hemorrhage include a group of diseases collectively called hemorrhagic diathesis. Their reasons may be different:
- Deficiency of certain proteins responsible for platelet hemostasis (thrombocytopathy and thrombocytopenia).
- Damage to the walls of blood vessels (Osler syndrome, hemorrhagic vasculitis, hemorrhagic telangiectasia, etc.).
- Bleeding disorders (fibrinolytic purpura, hemophilia, radiation sickness).
- Regular or temporary use by the patient of aspirin-containing drugs , fibrinolytics, anticoagulants.
A tendency to bleeding can also be caused by certain infections (typhoid, scarlet fever), liver pathologies (hepatitis, cirrhosis), diabetes mellitus, and changes in hormonal status.
Increased blood pressure may also be the cause of blood flow from the socket that does not stop. Moreover, this is one of the most common common factors of any hemorrhage, including alveolar hemorrhage.
Statistics and reasons
According to statistics, bleeding after removal of a dental element occurs in 0.25% of patients. The cause of complications in 70% is the condition of the mucous membranes surrounding the hole and other local factors:
- Injuries to soft tissues, alveoli or interradicular septum.
- Termination of the effect of adrenaline as part of anesthesia.
- Inflammation in the damaged area.
- Alveolitis, which provoked purulent melting of a blood clot inside the unit.
- Damage to vessels located close to distant elements.
- Hemangioma.
- Damage to a blood clot in the socket.
The most common factor in the development of pathology is damage to periodontal tissues.
30% of bleeding is caused by systemic disorders in the body:
- Hemorrhagic diathesis.
- Hypertension.
- Diseases of the walls of blood vessels.
- Infectious diseases.
- Menopausal factor and other hormonal imbalances.
- Blood diseases.
How long does bleeding last
Patients are interested in the answer to the question of how long bleeding lasts after tooth extraction.
Normal: from 10 to 30 minutes. It is during this period of time that the first blood clot should normally form, and the blood, accordingly, will clot and gradually stop. This should happen even if a complex procedure was performed, for example, a wisdom tooth was removed.
Pathology: prolonged bleeding after tooth extraction, which can last from several hours to several days. It is also impossible to call situations normal when the blood stopped in the dentist’s office, but at home it began to flow again, and not to ooze, but to be released in large volumes.
Diagnostics
Primary diagnostic methods:
- measurement of pressure level, pulse rate;
- external examination, examination of the oral cavity, tooth extraction sites.
During the examination, the patient will be asked questions about his health and the time of occurrence of complications. It is necessary to determine the cause of the problem, for example, whether the patient has eaten or drunk, or whether there is a fever. In some cases, differential diagnosis will be carried out to determine the presence of the following diseases - diabetes, hypertension, diathesis, hepatitis, leukemia during an exacerbation.
Differential diagnosis
The main goal of diagnosis is to differentiate local factors from systemic factors or the consequences of taking anticoagulant drugs. Questions to the patient help clarify the picture:
- what diseases does he suffer from?
- whether he is taking aspirin-containing drugs, oral contraceptives, NSAIDs and other drugs that cause a decrease in blood clotting;
- Have you had any difficulty stopping bleeding before?
To establish the exact cause of hemorrhage, it is necessary to exclude or confirm diseases that can cause coagulopathy:
- hemorrhagic diathesis;
- hemophilia;
- leukemia;
- liver cirrhosis or hepatitis;
- diabetes.
When differentially diagnosing alveolar bleeding, a blood test is usually required, and there is a need to involve a hematologist.
How to solve the problem at home
What to do if a similar situation arises with you or your immediate family? First of all, you need to assess the scale of the problem and the intensity of the bleeding. If it is really strong and does not go away for a long time, then you cannot hesitate; you cannot do without professional help and you need to visit a dental surgeon. Also, consulting a doctor is simply necessary in situations where the phenomenon was caused by systemic diseases of the body (diabetes mellitus, impaired hemostasis). If blood only oozes, then first aid must be provided. Let's look at local ways to stop bleeding.
Tampon application
Applying a tampon will help stop bleeding
You will need a regular sterile bandage. Make a fairly tight tampon from the bandage, then apply it tightly to the wound surface and bite. Despite the fact that such a homemade tampon should fit very tightly, it should not cause pain. How long does it take for the bleeding to stop in this case? You need to keep the bandage on for about 20-30 minutes; due to compression (squeezing) of the edges of the wound, improvements should occur during this period of time.
If the procedure is not beneficial, you can roll the gauze swab out of the bandage again and pre-moisten it with hydrogen peroxide (3%). Next, you need to repeat the procedure.
Application of cold
You can narrow blood vessels and stop bleeding with ice, as well as any product taken from the freezer. The main conditions here are to apply cold only externally, after wrapping it in a towel or any other soft cloth. Apply to the cheek from the side of the extracted tooth, leave for five minutes with breaks of 5-10 minutes. The total number of applications is 3-4 times.
This is interesting: The wisdom tooth is growing and the gums hurt - what to do and what to rinse with
Cold causes capillaries to constrict
Using a hemostatic sponge
Hemostatic sponge absorbs secretions
This is a material that professional doctors use in their practice (however, it is sold in pharmacies). It can be used according to the principle of tamponing the hole (i.e., exactly the same as in the first method). But applying the material has nuances: when soaked in blood, it immediately reduces its size, so you definitely need to take a fairly large piece of sponge. It is also necessary that the sponge sinks slightly into the hole after application. To place it, it is better to use thin tweezers. It is even better that all manipulations are performed not by you, but by one of the people nearby, otherwise you can easily injure the wound even more.
Normalization of blood pressure
It is advisable to do this even for those who do not have problems with blood pressure and do not suffer from hypertension, because... In stressful situations, such as tooth extraction, pressure can naturally increase. If the readings are high, then take the appropriate medication.
If the methods do not help, and the bleeding within 1-2 hours does not stop, then you need to consult a doctor.
Tranexamic acid
In patients with hereditary angioedema, before starting treatment, consultation with an ophthalmologist is necessary (determining visual acuity, color vision, condition of the fundus). During treatment, regular ophthalmological examination is necessary (including assessment of visual acuity and color perception, examination of the fundus with a slit lamp, measurement of intraocular pressure, assessment of visual fields). If visual impairment occurs during treatment with tranexamic acid, the drug must be discontinued.
In patients with hereditary angioedema who have been receiving tranexamic acid for a long time, regular laboratory monitoring of liver function is necessary.
Tranexamic acid preparations should be used with caution in hematuria caused by diseases of the renal parenchyma, since intravascular fibrin deposition is often observed in these conditions, which can aggravate renal damage. In addition, in cases of massive bleeding of any etiology from the upper urinary tract, antifibrinolytic therapy increases the risk of blood clots in the renal pelvis and/or ureter and, accordingly, secondary mechanical obstruction of the urinary tract and the development of anuria.
Although clinical studies have not revealed a significant increase in the incidence of thrombosis, the risk of thrombotic complications cannot be completely excluded. Cases of the development of venous and arterial thrombosis and thromboembolism in patients receiving tranexamic acid have been described. In addition, cases of occlusion of the central retinal artery and central retinal vein have been reported. Several patients developed intracranial thrombosis during treatment with tranexamic acid. Accordingly, in patients with a high risk of developing thrombosis (history of thromboembolic complications, cases of thromboembolism in relatives, verified diagnosis of thrombophilia), tranexamic acid should be used only if absolutely necessary and under strict medical supervision. Before using tranexamic acid, an examination should be performed to identify risk factors for thromboembolic complications.
The presence of blood in cavities, such as the pleural cavity, joint cavities and urinary tract (including the renal pelvis and bladder) can lead to the formation of an “insoluble clot” in them due to extravascular coagulation, which may be resistant to physiological fibrinolysis.
Patients with irregular menstrual bleeding should not be prescribed tranexamic acid until the cause of dysmenorrhea is determined. If the amount of menstrual bleeding is inadequately reduced during treatment with tranexamic acid, alternative treatment should be considered.
There is insufficient data on the effectiveness and safety of the use of tranexamic acid in the treatment of menorrhagia in patients under 15 years of age, so the drug should be used with caution.
Tranexamic acid should be used with caution in women concomitantly taking combined oral contraceptives due to the increased risk of thrombosis (See section "Interaction with other drugs").
In patients with DIC who require treatment with tranexamic acid, therapy should be carried out under the close supervision of a physician experienced in treating this disease.
Due to the lack of adequate clinical studies, the simultaneous use of tranexamic acid with anticoagulants should be under the close supervision of a specialist experienced in the treatment of blood clotting disorders.
If vision impairment occurs while taking tranexamic acid, you should stop taking the drug and consult a doctor.
When is it time to go to the doctor?
All home remedies for stopping bleeding after tooth extraction did not work, and you also notice other alarming symptoms: swelling of the mucous membrane, persistent pain (pain radiates to the head and other parts of the face), a lot of blood and you even have to spit it out, general weakness , increase in body temperature - do not hesitate to consult a doctor!
On a note! Did the situation take you by surprise at night? Find a 24-hour private clinic where services will be provided for a fee. Or go to the emergency room of a government institution, but do not forget to take your insurance card and passport with you. Sometimes government agencies may also require SNILS, which is not mandatory, but often becomes the subject of disputes with staff, especially when it comes to free treatment.
If you are going to get to the hospital in person, then do not drive, because... general weakness can lead to poor concentration. If you are not ready to get to the clinic on your own, you can call an ambulance and describe all the symptoms you have. Upon arrival, doctors will most likely try to tampon the hole with hydrogen peroxide, but if there is no result, they will take you to the appropriate department.
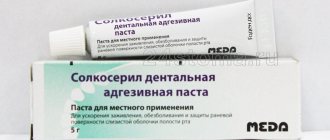
Treatment
Using surgical instruments, a blood clot is removed from the socket, it and the adjacent area of the alveolar process are dried, the wound is examined and the cause of the bleeding, its nature and location are determined. Bleeding from a damaged mucous membrane is stopped by suturing the wound, on the wound, ligating blood vessels or suturing tissue; bleeding from small vessels can be stopped by electrocoagulating them. If a bone vessel is damaged, it is compressed with forceps or another surgical instrument. After stopping the bleeding, the postoperative wound should be sutured. To stop bleeding from the depths of the socket, tamponade is performed using various means. The simplest and most accessible method of hemostasis is tamponade with iodoform gauze, which is removed from the socket no earlier than 5-6 days after the start of granulation of the socket walls. For tamponade of the hole, you can use hemostatic gauze “Oxycelodin”, as well as gauze impregnated with a solution of thrombin, hemophobin, epsilon-aminocaproic acid, ampher, and the drug caprofer. A good hemostatic effect is achieved by introducing absorbable biological hemostatic drugs into the socket: hemostatic sponge, fibrin film, cotton wool, foam, fibrin glue, biological antiseptic tampon (BAT), gelatin or collagen sponge.
Local therapy
Local treatment involves establishing the exact location of hemorrhage, antiseptic treatment of the wound, packing the hole, and suturing.
If the interradicular septum is bleeding , it is compressed with forceps, a tight tamponade is made with a gauze swab impregnated with iodoform-alcohol, and several sutures are placed on the hole with polyamide or catgut thread.
A gauze ball is placed on top, which the patient bites on. If after half an hour or an hour the bleeding stops, the patient is sent home. The tampon is removed from the wound after 4-5 days.
If the source of hemorrhage is damage to a large vessel , it is bandaged with catgut or polyamide thread, sutures are applied if necessary, a gauze swab is placed and pressed with teeth.
If stopping hemorrhage is unsuccessful, the patient is hospitalized and undergoes general hemostatic therapy, the type of which is determined by the specific clinical situation.
General methods
If local methods do not help stop the bleeding, this indicates a violation of hemostasis and requires laboratory tests for blood clotting and general hemostatic measures based on their results.
This can be an infusion, injections of coagulants and hemostatics, transfusion of red blood cells. With the development of pronounced inflammatory processes in the gums, antibiotics are prescribed.
The choice of hemostatic agents is very wide. The most commonly used are the following:
- Aminomethylbenzoic acid and its analogues - Ambien and Pamba.
The mechanism of action of these drugs is based on a decrease in activity and a decrease in the production of fibrinolysin in the blood, a component responsible for anticoagulant functions. Release form: tablets, solutions for intravenous and intramuscular administration, sponges intended for packing bleeding wounds. - Aminocaproic acid . A drug with the same mechanism of action as aminomethylbenzoic acid. It is taken orally and intravenously.
- Calcium gluconate and chloride . The therapeutic effect is provided by calcium ions, which reduce vascular permeability, have a hemostatic effect, and normalize blood clotting. Available in the form of solutions for intravenous and intramuscular administration and tablets.
- Etamsylate (analogue – dicinone). Coagulant and hemostatic. Stimulates the adhesion of red blood cells, reduces the permeability of vascular walls, and increases blood clotting function. Available in tablet form and solutions for intravenous and intramuscular administration.
- Vikasol. Contains synthesized vitamin K, which ensures blood clotting. It is produced in the form of solutions for intravenous administration and tablets.
- Ascorutin. Contains rutozoid (vitamin P) and ascorbic acid, effective as a means of combating vascular fragility, normalizing hemostasis.
Vitamin C injections, agents that stimulate regeneration, and non-steroidal anti-inflammatory drugs are also prescribed.
The most common cause of bleeding is increased blood pressure. Taking antihypertensive drugs in this case is a simple and effective way to stop bleeding.
Publications in the media
Pulmonary hemorrhage (PH) - the release of sputum stained with blood (hemophthisis) or pure blood (hemoptoe) when coughing.
Classification • I degree - excretion of up to 300 ml of blood per day (usually hemoptysis) • II degree - excretion of up to 700 ml of blood per day •• without a decrease in blood pressure and Hb concentration •• with a decrease in blood pressure and Hb concentration • III degree - excretion per day more than 700 ml of blood •• massive bleeding, accompanied by a decrease in blood pressure and Hb concentration •• fulminant bleeding, ending in death (death occurs from asphyxia - “drowning in one’s own blood”).
Etiology and pathogenesis
• LC can occur with diseases of the respiratory system, cardiovascular system and lesions of the mediastinal organs. With pulmonary tuberculosis, LC occurs in 10–12% of patients. LC is a common symptom in lung cancer, bronchial carcinoid, aspergilloma, abscess and gangrene of the lung, bronchiectasis, pulmonary infarction, Goodpasture's and Wegener's syndromes.
• Bleeding from the pulmonary circulation •• diapedetic (infiltrative pulmonary tuberculosis without disintegration) •• with hypertension in the pulmonary circulation (mitral stenosis, congenital heart defects, massive mediastinal tumors) •• rupture of the branches of the pulmonary artery or vein in chronic diseases: fibrous cavernous tuberculosis, chronic abscesses; in acute diseases: acute abscess or gangrene of the lung; with a rapidly progressing malignant process in the lung, pleura, mediastinum.
• Bleeding from the systemic circulation accounts for 80–90% of all bleeds. In chronic inflammatory diseases, restructuring of the bronchial arteries of the submucosal and mucous layers of the bronchi occurs, the development of arteriovenous anastomoses and pulmonary hypertension.
• LC associated with blood coagulation disorders are rare.
Clinical picture • Isolation of sputum with blood or pure scarlet foaming blood when coughing • Depending on the degree and duration of bleeding, signs of anemia, cardiovascular and respiratory failure increase • Aspiration of blood into the respiratory tract: moist rales in the lower parts of the lungs (usually in bleeding side), rapid development of aspiration pneumonia.
Complications • Asphyxia • Aspiration pneumonia • Dissemination or exacerbation of the inflammatory process.
Laboratory tests • Decrease in the concentration of Hb, erythrocytes, Ht • When aspiration pneumonia is associated - leukocytosis • With prolonged bleeding against the background of destructive processes in the lungs - disorders of the blood coagulation system.
Special studies • Chest X-ray in three projections •• Areas of hypoventilation or atelectasis •• The appearance of a fluid level in a cavity formation or an increase in the volume of the cavity • Bronchoscopy •• Detection of the source of LC (disintegrating tumor, bleeding carcinoid, bronchonodular fistula, etc.) • • Indirect signs - bleeding from the mouth of the bronchus, blood clots in the lumen of the bronchi, local endobronchitis • When bleeding has stopped, diagnostic segmental bronchoalveolar lavage with sediment microscopy is used - the information content of the method reaches 80–90% • Angiography of the bronchial arteries: the information content reaches 90% • After stopping bleeding, CT and bronchography can be used.
Differential diagnosis • Gastric bleeding (weakened patients, children can swallow blood, which is then ejected as gastric contents) • Pseudohemoptysis - spitting saliva, sputum stained with blood only in the morning, a pinkish spot on the pillow after sleep - observed in diseases of the oral cavity, pharynx, poorly fitting dentures.
Treatment • Urgent hospitalization, for LC II–III degrees - to the intensive care unit • For LC II–III degrees, the prescription of broad-spectrum antibiotics is indicated • LC must be stopped using conservative methods: the mortality rate of surgical operations performed at the height of LC is 20%, and after stopping LC - 2% • Method of controlled arterial hypotension: decrease in systemic blood pressure by 15–20 mm Hg. has a distinct hemostatic effect. The most commonly used is continuous drip or fractional intravenous administration of ganglion blockers (azamethonium bromide) under blood pressure control. Even if a rapid effect is obtained, controlled arterial hypotension is maintained for 2 days. The effectiveness of the method is 90–95% • Bronchoscopy • When a source of LC is detected, applications of vasoconstrictors (epinephrine), electro-, laser or argon plasma coagulation are carried out • If indirect signs of bleeding are detected - bronchial lavage with ice-cold physiological solution (no more than 400 ml) • If the above methods are ineffective, tamponade of the bleeding bronchus is used with a Fogarty-type balloon or a foam sponge obturator (the diameter of the obturator should be 3 times the diameter of the bronchus). The tampon is removed after 7–10 days, if there is a surgical pathology - on the operating table • Embolization of the bronchial arteries is a highly effective method, although, like the other above methods, it provides a temporary stop of LC • At the same time, disorders of the blood coagulation system are corrected (10% calcium solution chloride, etamsylate, fresh frozen plasma) • In case of life-threatening LC, emergency rigid bronchoscopy under anesthesia with tamponade of the main bronchus is indicated; if bronchoscopy is impossible, tracheal intubation with a double-lumen tube and transfer to single-lung mechanical ventilation.
Surgery. The scope of the operation and timing depend on the identified pathology and the general condition of the patient. The extent of the operation can vary from pneumonectomy to cavernotomy or abscessotomy with cavity tamponade.
The prognosis for stage II–III LC is always serious, because at any moment the bleeding may intensify and lead to asphyxia.
Prevention: timely diagnosis and adequate treatment of the underlying disease.
Abbreviations • PB - pulmonary hemorrhage.
ICD-10 • P26 Pulmonary hemorrhage that occurred in the perinatal period • R04.8 Bleeding from other parts of the respiratory tract.
Consequences of prolonged bleeding
If the bleeding does not stop for a long time after tooth extraction, many people become nervous and even believe that this can be fatal. Is it really? No one has ever died from blood loss after extraction, but patients have encountered other complications. Let's list them:
- poor health and weakness. Prolonged blood loss can cause dizziness, blood pressure drops, and pale skin.
- dry socket effect. A protective clot does not form on the wound, and it is susceptible to bacteria; food debris can get into it, which will rot,
- infectious and inflammatory process. Alveolitis, gumboil, osteomyelitis and phlegmon may develop. At the same time, the body temperature will rise, severe pain will be tormented, and pus may be released from the wound.
Interesting! In 2009, a woman died in the UK after having several teeth removed the day before. Reason: excessive blood loss. As it turned out, the woman hid from doctors the presence of a whole “bouquet” of diseases: cirrhosis of the liver, a blood clotting disorder.
“If you are planning any surgical operation, be sure to inform your doctor about all your existing diseases and individual characteristics. Then the specialist will draw up a treatment plan taking into account your health problems and select the necessary medications. This will help to avoid postoperative complications even if the removal was difficult and the patient has serious illnesses,” says A.V. Kryukov, dental surgeon with 12 years of experience.
Complications after wisdom tooth removal
Manipulations for the extraction of wisdom teeth should not be underestimated, since even if such procedures are carried out correctly, the patient may experience complications.
This is interesting: Tooth hurts after nerve removal: when to urgently see a doctor?
Edema
One of the most common consequences that occurs after tooth extraction is swelling. The reason for this may be partial damage to the tissues around the tooth. Usually the swelling goes away within 1-2 days. To speed up the elimination of swelling, this can be done by applying cold compresses to the cheek.
Fever
After a tooth is removed, the body’s natural reaction is to increase body temperature. This condition can last for 2-3 days. To improve your health, you need to take antipyretic drugs, but if the condition does not improve, you should immediately visit a doctor.
Soreness
Pain after extraction of the “eight” occurs due to damage to the periodontal tissues and nerves. If the pain cannot be tolerated, then for relief you need to take analgesics. When painkillers do not help, you should go to the dentist.
Suppuration of the socket
If the wound becomes infected, suppuration may occur. The reasons for the formation of pus may be non-compliance with medical recommendations and improper care of the oral cavity, as well as dental fragments remaining in the tissues after surgery. Self-medication in such cases is inappropriate; only a qualified doctor can prescribe adequate treatment and eliminate the cause of suppuration.
Dry socket
The blood clot must remain in the wound. It protects nerve endings and bone from microbial penetration. Therefore, on the first day after the manipulation, you should not rinse your mouth, and also do not eat hot food.
If a dry socket forms, this leads to increased pain, inflammation and alveolitis. In such cases, the doctor places a tampon with anti-inflammatory gel on the sore spot. Treatment continues until complete healing.
Clinical picture
Symptoms of the pathology are blood leaking out from under the blood clot and spreading to adjacent tissues and teeth. When the arteries or arterioles of the mucous membrane are damaged, the blood flow pulsates.
The long process is accompanied by manifestations of blood loss: deterioration of health, pallor of the skin, acrocinosis, increased heart rate, dizziness and hypotension. The listed signs are life-threatening. When they appear, a doctor's examination is required.
Differential diagnosis
What a doctor should do if a patient complains of alveolar bleeding:
- Clinical examination.
- Measurement of heart rate and blood pressure.
The dentist will certainly conduct a survey of the patient. List of questions:
- General health.
- Time of bleeding.
- Were there any provoking factors present?
- Does the patient suffer from hypertension?
- Have you ever had problems stopping bleeding from cuts and injuries?
- There is an increase in body temperature.
- Measures taken by the patient to eliminate the pathology.
- Presence of concomitant pathologies.
- What medications does the person take?
Hospitalization is required for persons taking medications that reduce blood clotting.
Differential diagnosis is carried out with systemic diseases that have complications in the form of increased bleeding.
Recommendations for the patient
Some patients are able to cope with the pathology on their own. A set of simple measures will help:
- Blood pressure measurement. If the value increases above normal, you must take appropriate medications.
- Make a turunda from cotton wool or gauze and press it tightly to the hole. Pre-treat the area with 3% hydrogen peroxide. After half an hour, release the pressure on the bandage.
- Rinse your mouth. Do not consume hot food or drinks.
- Apply cold to the “sick” cheek.
It is forbidden to “put” cold directly into the hole. This will lead to inflammation and infection.
If the condition worsens, you should consult a dentist or call an ambulance.
Treatment methods
If there are signs of serious blood loss, hospitalization and intensive infusion are required.
- Local therapy
Methods for stopping bleeding using local therapy are determined by the reasons that provoked the pathology. If blood comes from the hole, the area needs to be cleaned of the clot and antiseptic treatment is required. The problem area is dried with a tampon and tamponade is performed with a turunda with iodoform or a hemostatic sponge.
The hole is filled, starting from the bottom, layer by layer. When deleting an element with multiple roots, each channel is processed separately.
Upon completion of packing, the edges of the wound are connected and sutured. The gums are covered with a gauze pad for an hour. If there is no bleeding, the gauze is removed and the patient is sent home.
If bleeding continues, packing is repeated and ice is applied to the cheek. Turunda is removed from the hole after five days.
Gum rupture is repaired by suturing. When perforation of the bony septum occurs, the edges are compressed with orthodontic forceps and tamponade is performed. Occasionally, ligation is required.
- General methods
The method of stopping the flow of blood from the socket due to systemic reasons is determined by their type and nature.
For blood clotting disorders, coagulants are used. For hemorrhages due to hypertension, antihypertensive drugs are used. The doctor selects drug treatment based on clinical indications.
Preventive measures
Prevention of alveolar hemorrhage consists of fulfilling two main conditions.
- It is necessary to allow time for a blood clot to form in the hole , which will prevent bleeding. There is no need to rush to relieve the pressure on the cotton swab, much less get rid of it. If blood clotting is normal, it should be kept for at least 30 minutes.
- You cannot take actions that could destroy this clot. Such actions include eating hot food or drinks immediately after tooth extraction, vigorously rinsing the mouth, and brushing your teeth the first day after tooth extraction.
General recommendations
To avoid such problems, we strongly recommend that you follow the simplest rules of the rehabilitation period:
- Eating can be done no earlier than 3 hours after tooth extraction.
- Don't eat hot or cold foods.
- Give preference to liquid porridges and broths. Supam. Solid foods should be avoided until the hole is completely healed.
- Avoid taking hot baths and saunas.
- Avoid heavy lifting and exercise for a week.
- After tooth extraction, you should not rinse your mouth; this will significantly increase the healing time of damaged tissue.
- Limit brushing your teeth for the first 24 hours.
- You should not drink alcohol for a week after the operation.
- Never apply warm or hot compresses to your cheek.
Advice for the patient
What to do if you continue to bleed or start bleeding from the socket of an extracted tooth? First of all, prepare a tampon from sterile cotton wool/gauze, place it on the hole, press firmly with your teeth, and maintain this position for half an hour. Over time, the pressure on the tampon can be eased, but there is no need to rush to remove it.
While holding the tampon, you need to measure your blood pressure and, if necessary, take an antihypertensive drug.
You can speed up blood clotting by placing something cold on your cheek, such as a plastic bag filled with water and ice.
While fighting bleeding, you should not eat or drink anything. If it does not stop (this can be easily checked by the condition of the tampon), depending on its intensity, you need to go to the clinic yourself or call an ambulance.
The video provides recommendations from a leading dentist in case of bleeding after tooth extraction.
What not to do
To prevent the development of recurrent bleeding, the patient must adhere to the following rules for 48 hours. It is forbidden:
- Do heavy physical work, bend over and play sports.
- If stitches have been placed, spit and make active facial movements.
- Drink any alcoholic beverages and smoke.
- Injure the socket: drink drinks through a straw, chew on it, touch it with your tongue.
- Take a hot bath, steam in a sauna or visit a sauna.
- Eat tough and solid foods.
- Drink and eat hot (cold) drinks and meals for 3-4 days.
- Drink aspirin and drugs in which it is present.
- Warm (apply heat) the area of the extracted tooth.
- Chew gum.
Following these recommendations will help avoid the development of unpleasant consequences and promotes the proper formation and fixation of a blood clot in the vessel. It may take up to 3 months for the wound to heal completely.
How much should you not eat after extraction and why?
You should not eat immediately after pulling out a tooth; you should wait at least a few hours. While under anesthesia, the patient is not able to control the process of biting food, so he can damage his cheeks, lips, or even get burned without realizing it. You should refrain from eating solid foods and hot drinks. During the first three days, you can only eat soft, not too hot food, so as not to disturb the healing of the wound and not to endanger the clot that has formed in the hole.
If the bleeding does not stop, despite following all the rules for post-operative oral care and nutrition outlined by your dentist, contact your doctor or emergency services immediately.
Sources
- https://kiberis.ru/?p=32357
- https://eltransteh.ru/kod-mkb-pri-lunochkovom-krovotechenii/
- https://my-ort.ru/novosti/lunochkovoe-krovotechenie/
- https://berezkadent.ru/about/polezno-znat/krovotechenie-posle-udaleniya-zuba-mudrosti/
- https://anZub.ru/lechenie-zubov/krovotechenie-posle-udaleniya-zuba/
- https://mnogozubov.ru/krov-ne-ostanavlivaetsya-posle-udaleniya-zuba/
- https://dentist-pro.ru/xirurgiya/udalenie-zubov/kak-ostanovit-krov-posle.html
- https://StomaGet.ru/hirurgiya/kak-ostanovit-krov-posle-udaleniya-zuba
Bleeding from the socket after tooth extraction
Often, after tooth extraction, bleeding occurs from the socket (hemostasis), which occurs due to rupture of ligaments and capillaries (blood vessels). The complication may appear immediately, or maybe after a few days. Hemostasis can be stopped using a gauze pad, which the doctor places on the bleeding area for 15-20 minutes. During this period, a clot forms in the socket, after which the bleeding usually stops. If this does not happen, then stopping is done in other ways: by suturing with catgut, using hemostatic paste (sponge), applying fibrin film, or using special preparations in the socket.
Recommendations after tooth extraction
After the tooth is removed, the patient is allowed to go home if there is no bleeding from the socket. The doctor gives the patient the necessary recommendations, which must be strictly followed. If these rules are followed correctly, bleeding can be avoided.
- At least three hours should pass from the moment of tooth extraction to the first meal.
- It is strongly recommended not to smoke within three to five hours after tooth extraction.
- On the day of surgery, avoid physical activity and lifting heavy objects.
- Also, on the day of removal, you should not eat hot food, steam or take a hot bath.
- When brushing your teeth, be especially careful on the side where the tooth was removed.
- Do not take medications that contain aspirin (this drug thins the blood).
- The next day after surgery, carefully rinse your mouth with a warm, weak solution of potassium permanganate, chlorhexidine or furatsilin. This cannot be done on the day of removal.
- To speed up healing, you can carefully rinse your mouth with decoctions of medicinal herbs (chamomile and sage), and also lightly lubricate it with sea buckthorn oil.
- Do not touch the wound with your fingers (even your tongue), stay as far away from drafts as possible.
It often happens that bleeding from the socket appears several days after the operation. There may be several reasons for this: a complex removal procedure, accidental injury, poor blood clotting, a jump in blood pressure, problems with a herbal clot, as well as failure to follow the rules recommended by the doctor.
How to stop bleeding from a socket after tooth extraction
If bleeding from the socket of an extracted tooth occurs far from the clinic, then you can stop the bleeding at home yourself. To do this, you need to use the following method: make a thick tampon from a sterile medical bandage, moisten it slightly (preferably with lukewarm boiled water), then carefully apply it to the bleeding area and close your teeth. The tampon should not be too large, otherwise it will put too much pressure on the blood vessels. Then take a quiet position, sitting or lying down, and try to relax while continuing to close your teeth.
You can also replace the tampon with a bag of black tea - thanks to the tannins included in the composition, the blood stops faster. But if these methods do not help, then it is possible that a large vessel is damaged. Then you can try this method: mix one spoon of salicylic acid solution with two spoons of peach oil and seven spoons of beeswax. Heat the mixture to a boil, cool, pipette and drop into the well. The mixture will harden and turn into a protective film that will stop the bleeding. It is better to place a cotton swab on top of the resulting film.
If this method does not help, and the bleeding does not stop, contact a specialist immediately! Otherwise, everything can end in blood loss and even life-threatening.