Neuritis
is an inflammation of the peripheral nerve trunk.
The peripheral nervous system refers to the nerve structures outside the brain and spinal cord (which are in turn called the central nervous system). Excitation (signal) is transmitted along the nerves, allowing the central nervous system to receive information about the state of all organs and systems of our body and control muscle contractions. The tissues of various organs are penetrated by nerve endings, which are connected to the brain, and in most cases to the spinal cord using bundles of nerve fibers enclosed in a sheath of connective tissue. Such bundles are called nerves, and large nerves are called nerve trunks.
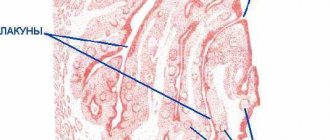
With neuritis, nervous tissue is involved in the inflammatory process. This leads to the fact that the signal in some part of the nerve passes worse or does not pass at all. Accordingly, the sensitivity of any area may be lost and the mobility of the muscles innervated by the affected nerve may decrease.
Types of neuritis
A distinction is made between local neuritis and polyneuritis.
Local neuritis
is an inflammation of any one nerve (facial, auditory, oculomotor, glossopharyngeal, radial, sciatic, peroneal, femoral, etc.).
Polyneuritis
is multiple inflammation of the nerves. If the effect of the factor that caused the inflammation is local, only one nerve is affected. Polyneuritis develops under the influence of a systemic factor, which, as a rule, leads to degeneration of the nerve sheath and nerve fibers.
Surgery
Certain surgical procedures can help relieve neuralgia pain when the condition does not respond to treatment.
Examples of surgical procedures that may help treat neuralgia include:
Microvascular decompression : Helps remove an enlarged blood vessel affecting a nerve. The procedure involves placing a soft pad between the blood vessel and the affected nerve.
Stereotactic surgery : This is a non-invasive procedure that directs highly concentrated beams into the root of the damaged nerve. The radiation disrupts the transmission of pain signals to the brain.
Percutaneous balloon compression : This involves inserting a small balloon into the affected nerve. The balloon is inflated, causing controlled, deliberate nerve damage. This procedure prevents the affected nerve from sending pain signals to the brain. However, the effects of the procedure usually wear off after 1-2 years.
Causes of neuritis
Local neuritis is caused by:
- local infection;
- local hypothermia;
- injury. Often neuritis develops after a nerve injury;
- compression of the nerve. Thus, neuritis of the axillary nerve can develop due to prolonged use of a crutch, neuritis of the peroneal nerve - due to working in an uncomfortable position, etc.;
- arthritis (in this case the nerve of the joint may become inflamed);
- tumor (if the tumor compresses the nerve).
Multiple neuritis (polyneuritis) can be caused by such reasons as:
- infectious diseases, including measles, herpes, influenza, malaria, diphtheria and some others;
- intoxication. Poisoning with arsenic, lead, mercury, carbon monoxide, phosphorus, bismuth and other highly toxic substances can lead to the development of various types of neuritis. The most common cause of multiple neuritis is alcohol poisoning;
- systemic diseases (diabetes mellitus, rheumatism, gout);
- avitaminosis;
- vascular disorders;
- as well as some other reasons.
Causes of the inflammatory process
Pathology appears after bacterial and viral infections or under the influence of external factors and internal processes in the body. The most common reasons are:
- consequences of ARVI, sore throat, bronchitis, influenza;
- previous injuries;
- pathological changes in blood vessels;
- poisoning: alcohol, toxic substances;
- diseases of the endocrine glands: thyrotoxic goiter, diabetes mellitus.
The disease also occurs due to compression of the nerve trunk. The reason may be the constant adoption of an uncomfortable posture. Thus, pianists and cellists often suffer from neuritis of the median nerve of the hand. Treatment will help avoid complete loss of sensitivity in the fingers or hand, and atrophy of muscle tissue.
Symptoms of neuritis
The main symptoms of neuritis are:
Pain along the nerve
The most common symptom of neuritis is pain along the affected nerve. The pain, as a rule, is dull in nature and intensifies in the cold, with physical activity or uncomfortable body position.
Sensory impairment
Sensory loss in the area of the affected nerve is common. It can manifest itself in the form of numbness, tingling, or “pins and needles.”
Decreased muscle activity
There is a partial decrease in muscle strength (paresis), a decrease or loss of tendon reflexes, and in some cases, muscle paralysis (complete cessation of muscle activity).
Vegetative and trophic disorders
With neuritis, there may be such vegetative and trophic disorders as depigmentation of the skin, the acquisition of a bluish tint, local hair loss, increased sweating and dry skin, swelling.
Trigeminal neuralgia: symptoms and treatment
After the first painful attack, you can grimace as much as you like, feel every millimeter of facial skin and even pat yourself on the cheeks approvingly. Everything is fine! But the fear of the next attack has already settled in my soul forever... This is how most of my patients describe the debut of a painful and difficult-to-treat disease called “trigeminal neuralgia” (trigeminal neuralgia, Fothergill’s disease).
Waiting for the pain
Unlike tension headaches, trigeminal neuralgia is characterized by sudden, short-term, intense, recurring pain in the area of innervation of one or more branches of the trigeminal nerve, usually on one side of the face, but can affect both sides, and can (in an atypical form) manifest as a burning sensation , pressing, aching, bursting, constant or wave-like pain or a feeling of goosebumps running across the face.
Attacks of these pains in the face (lip, eye, nose, upper and lower jaw, teeth, gums, tongue) can occur spontaneously or be provoked by talking, chewing, brushing teeth, touching certain areas of the face (trigger points that trigger an attack; usually located in area of the nasolabial triangle). Their frequency varies from single to tens and hundreds per day! During the period of exacerbation, more often in the cold season, attacks become more frequent.
The pain is so severe that patients cannot concentrate on anything else and are in constant tension, all the time waiting for the next attack (they do not touch the painful side of the face, do not brush their teeth, do not chew on the affected side). There have been cases where patients, unable to bear the pain any longer, committed suicide.
What really hurts
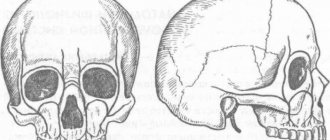
The main cause of true trigeminal neuralgia is compression (squeezing) of the trigeminal nerve root by an arterial and, less commonly, venous vessel directly at the brain stem, from where this nerve actually exits.
The trigeminal nerve, on the one hand, is the main sensory nerve of the face and oral cavity, on the other, it also contains motor fibers that innervate the masticatory muscles. Therefore, in addition to transmitting information to the brain about what our face is doing at any given time, the trigeminal nerve carries impulses to some of its own facial muscles, which is why pain is often accompanied by a tonic, long-term (trismus), or short-term (tic) contraction of these muscles.
There are several hypotheses to explain why nerve compression leads to the development of trigeminal pain, but none of them is yet generally accepted. In all cases, confirmation of a neurovascular conflict is carried out only with the help of MRI, so the doctor will definitely refer you to this study. Unfortunately, in 15% of patients, even an MRI is not able to accurately establish a diagnosis. Then electromyography (EMG) or electroneurography (ENG) can help doctors.
Diagnostic problems
But alas, most often after the first attacks a person is sent not to a neurologist’s office, but to a dental clinic. This is due to the fact that the area of pain is located not only on the face, but also in the oral cavity. Very often, healthy teeth are removed by mistake on the affected side, sometimes this “attraction” lasts for months and years, and only after losing half of the “emergency reserve” of teeth does the patient begin to suspect something...
The standard for diagnosing classical trigeminal neuralgia, according to the diagnostic criteria of the International Headache Society (IHS, ICHD-II), is the presence of at least 4 points out of the 5 below:
- The pain occurs in the form of attacks lasting from several seconds to 2 minutes in areas of the face corresponding to the zones of innervation of the trigeminal nerve.
- The pain is sudden, intense, sharp, similar to an “electric discharge”, caused by irritation of various areas of the face and oral cavity when eating, talking, washing the face, brushing teeth.
- Attacks of pain are stereotypical for each patient.
- There are no neurological symptoms during the interictal period.
- Taking carbamazepine causes pain relief at the onset of the disease.
Conservative therapy
Treatment always begins with conservative therapy, the basis of which is anticonvulsants (in particular carbamazepine). Their use at the onset of true trigeminal neuralgia leads to regression of the pain syndrome in 90% of patients. That’s why it’s so important not to delay seeing a doctor! However, with long-term use, the effectiveness of the drugs sooner or later decreases, toxic damage to the liver, kidneys, and changes in the cellular composition of the blood may develop, so conservative therapy can only be considered temporary.
In turn, patients prefer vascular drugs, antispasmodics, sedatives, ointments with anesthetics, physiotherapeutic procedures, acupuncture, laser therapy, and are happy to use traditional medicine methods and efferent methods of therapy (plasmapheresis, hemosorption).
In my experience, all this does not bring any particular relief, but it significantly distracts from the anxious anticipation of an attack. And... the time before examination and surgical treatment is delayed, which sometimes leads to tragic consequences. Meanwhile, the operation cannot be delayed.
Neurosurgical treatment
As for surgical treatment, today neurosurgeons have two main methods at their disposal:
Vascular decompression.
The essence of the method, as the name suggests, is to eliminate compression, i.e. compression of the nerve by the adjacent vessel. The method is indicated for all types of vascular compression of cranial nerves. To use it, an established diagnosis of classical trigeminal neuralgia is sufficient. A contraindication is the presence of severe concomitant pathology that makes it impossible to perform a neurosurgical operation.
Stereotactic radiosurgery, or “gamma knife”.
To achieve the effect, the trigeminal nerve root is irradiated with a dose of ~ 90 Gy and the affected cells are “burned out”. Indications for the use of this method are aggravated somatic status (presence of chronic diseases, mainly cardiovascular and endocrine) and the patient’s categorical refusal of surgical intervention. The use of the method is justified by the non-invasiveness of the technique, which significantly reduces the likelihood of complications, however, radiosurgery is less effective and has a higher number of relapses.
In general, the success of treatment for trigeminal neuralgia, just like the treatment of other diseases, depends on a clear diagnosis, strict adherence to surgical technologies and... your timely visit to the doctor!
Valentina Saratovskaya
Photo thinkstockphotos.com
Products by topic: [product](carbamazepine)
Treatment methods for neuritis
Neuritis must be treated. At the first signs of the disease, you should consult a neurologist. If treatment for neuritis is not started on time, the risk of developing paresis and muscle paralysis increases.
Treatment of neuritis is aimed, first of all, at eliminating the cause that caused it. If neuritis is of infectious origin, antibacterial therapy or antiviral drugs are used. If neuritis is of toxic origin, it is important to remove toxins from the body.
Drug treatment
In addition to antibacterial or antiviral drugs, the course of treatment for neuritis usually includes:
- B vitamins
- drugs that improve blood microcirculation
- drugs that increase the conductivity of nerve fibers
Massage
Massage of the muscles innervated by the affected nerve is recommended. Massage can be combined with heat therapy (infrared sauna).
More information about the treatment method
Physiotherapy
For neuritis, physical therapy methods such as electrophoresis, diadynamic therapy, SMT therapy, ultrasound therapy, magnetic therapy, and laser therapy can be used.
More information about the treatment method
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
The treatment program for this disease at the Bone Clinic may include:
Shock wave therapy
More details
PRP therapy
More details
Acupuncture administration of ozone
More details
Teraquantum therapy
More details
Interference therapy
More details
Who will treat you?
Bogdanov Vadim Yurievich
Chief traumatologist-orthopedist..
Read more
Ronami Valery Guseinovich
neurologist, reflexologist, chiropractor, professor, doctor of medical sciences.
More details
Dremin Evgeniy Vitalievich
neurologist, reflexologist, chiropractor.
Read more
Repeated appointments with a neurologist based on examination results in our clinic are free.
Diagnostics
As a rule, the diagnosis is made based on the patient's complaints and examination data. Almost all patients with trigeminal neuralgia undergo magnetic resonance imaging of the brain at some stage to rule out a tumor or multiple sclerosis. In addition to computer and magnetic resonance therapy, radiography of the paranasal sinuses is used to identify chronic inflammatory and other pathological processes; OPTG (orthopantomogram) to assess the width of the bone canals.
The patient requires consultation with several specialists: an ENT doctor, a dentist, a neurologist. A preliminary diagnosis can be made by a neurologist based on the patient’s complaints, studying the history of his disease and an objective examination of the face with an assessment of symmetry at rest and when trying to smile.
Over time, symptoms of inflammation of the trigeminal nerve can give rise to neuropathic complications and lead to the development of secondary pain syndrome. In the chronic form of the disease, the auditory and facial nerves are irritated. Without treatment, trigeminal neuralgia can lead to more serious complications, such as dystrophy of the masticatory muscles; decreased sensitivity of the affected area; synkinesis (cooperative movements in which one nerve controls many muscles); contracture and spontaneous contraction of the facial muscles; chronic lacrimation.