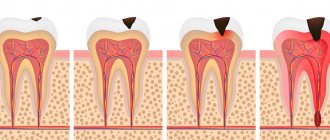
If caries is not cured in time, and there is a deep carious lesion, the only way out is to remove the dental nerve. As caries develops, microorganisms violate the integrity of the enamel, as a result of which the nerve is exposed and reacts to any influence with unbearable pain.
Depulpation (nerve removal) is a modern way to preserve a unit of dentition without implantation.
When nerve removal is indispensable
In modern dental practice, both complete and partial resection are used. Indications for the procedure:
- deep carious tissue damage;
- chronic pulpitis (including asymptomatic);
- bactericidal infection spread by the apex of the tooth root;
- the presence of an extensive pulp area, the threat of developing periodontitis or transition to periodontitis;
- trauma leading to nerve exposure and tooth destruction;
- the need to correct a medical error;
- the need for prosthetics with low crowns.
Unbearable pain can also be an indication for depulpation.
The dentist will never prescribe such a serious intervention as long as it is possible to save the tooth.
Important : problematic “eights” when affected by caries, as a rule, are removed. This is due to the location of the “wisdom” teeth at the end of the dentition, which makes cleaning them from plaque and stone and filling the canals very problematic. Indications for removal are also the wrong direction of eruption, displacement of the dentition, malocclusion, and the development of pulpitis.
Delete or restore?
In many cases, the decision to try to save or remove a problematic tooth is made by the patient himself. The desire of people to preserve a tooth at any cost is understandable and resonates with dentists, armed with the most modern and advanced methods of tooth preservation. However, some patients easily part with dental problems, explaining this action by lack of time for dental treatment or high prices for proper restorative dental treatment. I would like to remind such patients that if one tooth is removed and an implant is not installed in its place, this means inevitably provoking a gradual change in the entire dental system. Having saved money and time on the treatment of one tooth, you will have to face the need for implantation or prosthetics in the future, which require even greater costs. Family dentistry on Paveletskaya offers the patient to make the right choice, wanting to fight as hard as possible to preserve your teeth and at the same time having everything necessary for the successful restoration of problem teeth.
What is the dental nerve called?
In dentistry, the dental nerve, or pulp, is a complex structure - an interweaving of nerves and vessels located inside the root and crown of the tooth and responding to external stimuli.
Depulpation allows you to save the damaged tooth, but has negative consequences:
- Since the pulp acts as a barrier to infections, removing the nerve deprives the tooth of the necessary level of blood supply and mineralization, which shortens its “life.”
- A tooth deprived of a nerve loses sensitivity, the enamel becomes more fragile and faded, and the strength of the tooth decreases.
What is a “dead” tooth?
This is what dentists call a tooth without nerve endings that no longer receives blood. Consequently, the tooth stops receiving nutrients and its work stops, the tooth dies. The disruption of blood supply is explained by damage to the pulp, the area where blood vessels and nerve endings gather into a single bundle. If the vessels and nerves do not function, then the nutrients no longer support the life of the tooth.
Stages of the depulpation process
- X-ray – necessary to assess the condition of the pulp, the number, length and branching of the canals to be filled.
- Anesthesia - local or complete anesthesia completely covers the issue of pain when removing a nerve (it doesn’t hurt!). At the same time, general anesthesia is used relatively rarely - when treating children, with true dental phobia, etc.
- Installation of a rubber dam - a latex film for insulating a tooth. A modern solution to improve the dentist’s working conditions and protect against the possible spread of microorganisms through saliva.
- The actual removal of the nerve is the excision of tissues affected by caries, opening the pulp chamber and extracting the nerve with a special instrument (pulpoextractor). In modern practice, this is a careful cutting of the pulp without affecting sensitive areas.
- Installation of a temporary filling (for a period of 1-2 weeks).
- Control x-ray.
If the x-ray and the condition of the tooth are satisfactory, after the control period a permanent filling is installed.
Methods for restoring the aesthetics of a pulpless unit
Darkening of tooth enamel is an aesthetic problem that not all patients can accept. Dentists offer a number of methods aimed at restoring the external characteristics of a “dead tooth.” What to do in this case? There are 3 main methods for restoring blackened enamel: endobleaching, installation of veneers and crowns. Let's consider each of the listed methods in more detail.
Endobleaching
The method involves introducing whitening agents into the upper layers of the tooth. Typically, dentists use sodium perborate for the procedure. Endo-whitening is possible not only to restore the aesthetics of a “dead” tooth, but also to lighten the enamel tone in healthy teeth.
A healthy element loses its original external characteristics due to a number of factors:
- pulp damage followed by hemorrhage;
- installation of a composite, which began to color the crown of the tooth in a pinkish tint;
- darkening of the crown as a result of silvering of the tooth.
Endobleaching is performed according to the appropriate algorithm:
- Performing professional cleaning to remove hard and soft dental plaque.
- Removing old fillings.
- Injection of a bleaching agent into the cavity of the problematic element.
- Installation of a temporary filling.
The procedure is performed every week until the tooth becomes similar in shade to the rest of the row. The minimum number of visits to the dentist is 4–5 times. The permanent composite material is installed 10 days after the last gel injection procedure.
The results of endobleaching last for an average of 2–3 years. After this time, the procedure is repeated again in cycles. Patients are not recommended to undergo more than 3 courses of whitening due to the risk of crown breakage.
This method has a number of disadvantages:
- Impossibility of predicting the result of restoration.
- The impossibility of completely restoring the enamel due to its dullness.
- There are a number of contraindications to the procedure: allergic reactions to the injected bleaching agents; pregnancy; cracks in the enamel; pathologies of the endocrine system.
Veneers
The structures are thin linings made from several types of materials - ceramics and composites. Ceramic plates are often made from zirconium dioxide or porcelain. Porcelain veneers are identical to the enamel color of healthy units. This is achieved due to the transparency of the composites used.
Composite veneers are more affordable, but their service life does not exceed 5 years. This is due to the fragility of the products and their rapid loss of their original appearance.
Installation of veneers is also carried out in stages:
- Selection of the optimal shade of the plates.
- Grinding of the top layer of enamel for better attachment of the product to the tooth. During the procedure, about 0.5–1.5 mm of enamel is ground off.
- Manufacturing of crowns on special machines using 3D technologies. Products are produced in dental laboratories using impressions previously taken from the patient’s dentition.
- Fixation of finished structures using a special adhesive.
There are contraindications for installing veneers:
- bite pathologies;
- enamel abrasion;
- high risks of dental injury;
- bruxism;
- element wobble.
The most significant disadvantage of veneers is the need to wear them throughout your life. This is due to the fact that the teeth on which the onlays are installed are subjected to preliminary grinding and can no longer be restored.
Crowns
Dentists consider this method of restoring the appearance of a “dead” tooth to be preferable. This is due to several reasons:
- Increasing the strength of a problem unit by 30–60%.
- Possibility of preserving the root during the procedure.
- Possibility of ensuring uniform load on all areas of the jaw.
- Protection of tooth tissues from external negative influences.
- The disadvantage of the procedure is the need to grind the top layer of the tooth.
All methods of restoring a “dead” tooth have a negative impact on its health. In order not to resort to the restoration procedure, it is necessary to follow a number of preventive rules. These include: timely visits to the dentist; competent choice of dental care products; daily hygiene measures; flossing after meals; high-quality cleaning of the surface of the tongue; timely change of toothbrush (once every 3 months).
Depulpation before prosthetic crowns
Depulpation is unconditional if there is serious tooth decay. It is preferable to remove the dental nerve during prosthetics in the following cases:
- The size of the teeth determines the low position of the crown (too small or short teeth);
- The inclination of the prosthetic tooth is from 15°;
- Increased sensitivity of teeth;
- According to aesthetic requirements.
The need to remove the dental nerve during prosthetics is dictated by deep removal of the top layer of dental tissue: if the doctor is not sufficiently qualified, heating or touching the nerve can cause an attack of unbearable pain. However, cases of nerve-sparing crown installation also occur in modern dental practice.
If over time the nerve under the crown becomes bothersome, it is possible to remove the pulp through the top of the crown and fill the hole after removal.
The danger of such a procedure is associated with the risk of complications in the future due to surgery on the exposed dental nerve.
An alternative restoration method is the use of ceramic inlays.
Inlays are most often made of ceramic. When no more than 70% of the tissue in a tooth is destroyed, an inlay is an excellent method of restoration, which can also serve for many, many years. In the example below, we see that the teeth on the left were restored with light-rejecting fillings, and the teeth on the right were restored with inlays. This photo was taken three years after restoration. The inlays were made by the chief physician of the Family Dental Clinic, S.V. Tsukor. The fillings were not made in our center.
You can see that the fillings have areas of darkening, peeling and other defects, but they retain their functionality and do not fall out. The tabs on the right are in perfect condition even after years of use.
About dental anesthesia
Standard dental practice is an injection of anesthetic; Taking tablet analgesics before going to the dentist is not recommended, as it leads to a decrease in the effectiveness of anesthesia (usually the effect of an anesthetic injection is 45 minutes). For patients suffering from a fear of injections, it is possible to use paste anesthesia, which has a similar effect.
The choice of anesthesia is up to the dentist; Taking into account the individual pain sensitivity threshold of each patient, the standard dose is sometimes doubled or even tripled. With proper selection of an anesthetic, discomfort during the procedure for the patient is excluded.
Why can a tooth hurt after pulp removal?
This often happens: the nerve has already been removed, but the pain remains. Such manifestations are acceptable in the first 3-4 days as a natural reaction of the body (for example, to clenching the jaws or to temperature stimuli).
Other causes of toothache after pulp removal:
- Careless cleaning of the canals, preservation and intensification of the inflammatory process due to incomplete removal of tissue damaged by caries.
- Using during the procedure a pulp extractor that is not suitable for the size of the canal or improper handling of the instrument.
- Broken dental instrument, retention of its remains in the upper part of the root (such a medical error leads to the need to remove the tooth).
- The occurrence of a secondary inflammatory process in the treated canals (residual pulpitis) occurs against the background of an incompletely removed nerve.
- Allergic reaction of the patient to the filling material.
Procedure technology
The depulpation procedure can be carried out in three ways:
- vital extirpation – removal of the pulp occurs completely and is carried out under local anesthesia. The procedure involves removing the nerve in just one session, but requires careful examination;
- Devital amputation is the use of a special drug to mummify part of the nerve. It involves applying a special paste that leads to pulp necrosis. This technique is used extremely rarely, since it can cause a number of complications associated with necrotic processes in the nerves. Can only be found in low-budget dental offices;
- diathermy - necrosis of the nerve occurs by applying a current discharge, after which the dead nerve is removed. An electrode is inserted into the pulp area, passing a current through itself, which not only kills the nerve, but also cauterizes the wound.
After the depulpation procedure, you may experience pain for several days that occurs when you squeeze your jaw or eat hot or cold food (drinks). This pain does not require treatment and goes away on its own.
Change in enamel color after nerve removal
If the dental clinic follows international depulpation protocols, such phenomena are excluded. However, in budgetary institutions there are frequent cases of using outdated practices.
The color of the enamel after nerve removal can be affected by:
- Improper preparation of the tooth for installation of a filling;
- Poor quality instrumental processing of channels;
- Low quality filling materials.
Thus, when using resorcinol-formalin paste (the use of the material is practiced in the treatment of baby teeth), the enamel acquires a pinkish tint; When using endomethasone, the tooth may turn yellow after a few years.
Lifespan of a tooth without a nerve
How long does a tooth live without a nerve? The duration of operation is influenced by several factors:
- Quality of oral care after the intervention. Typically, the dentist gives the patient a number of recommendations that he will need to adhere to for 1-2 weeks. All these recommendations are aimed at minimizing the negative consequences after pulp removal. Typically they include: avoiding solid and rough foods; temporary exclusion of coloring foods and drinks from the diet; thorough oral hygiene using brush paste and dental floss; limiting excessive physical activity.
- Food quality. Solid foods consumed immediately after the element is sealed may cause the seal to fall out. In addition, they often cause chips and cracks in the enamel of the problem unit. As mentioned earlier, the “dead” segment is more vulnerable to negative external factors.
- The effect of the treatment.
- Regularity of patient visits to dental clinics.
The patient can independently make the tooth last longer; to do this, you need to follow some rules:
- include in your diet more foods containing phosphorus, calcium and other microelements necessary for teeth;
- take vitamin complexes during the off-season;
- Avoid using whitening toothpastes;
- Avoid using hard bristle brushes.
If the sealed element is destroyed as a result of the inept actions of the doctor or the patient himself, then it will no longer be possible to restore it. The only way out of the situation in this case is to remove the “dead” tooth.
Possible complications
A medical error associated with poor-quality disinfection of the canal when removing a nerve can trigger the process of suppuration with subsequent transition to a periodontal abscess (in the absence of adequate treatment). This complication leads to the need for tooth extraction.
Other possible complications:
- Pain for several days after nerve removal. The duration of discomfort is individual for each patient; if pain persists for a long time, it is necessary to consult a doctor to re-open the canals and carry out disinfection.
- Increased bleeding of the canal occurs when the pulp extractor is removed after the pulp has been torn off. To avoid this phenomenon, many specialists carry out the procedure in stages with copious rinsing of the tissues with an antiseptic. Bleeding control is carried out directly at the appointment.
- The appearance of granuloma, fistula, cyst, gumboil.
Specific problems can arise if the material is applied incorrectly: if the filling extends beyond the boundaries of the root apex, the jaw nerve may be pinched.
If you experience pain in the lips and chin, you should urgently consult a dentist: a possible complication is facial paralysis.
Characteristics of a pulpless tooth
The first problem that people encounter after depulpation is the fragility of the element. After the intervention, it is not recommended to chew hard and rough food on the problematic side, as this may cause breakage of the segment. After depulpation, many doctors advise patients to resort to restoring the problem unit using crowns or prosthetics. After restoration, it will be possible to preserve the integrity of the “dead” element for many years. With successful treatment and restoration, the tooth can last more than 10 years. Otherwise, the “dead” element will collapse within 1–2 years.
The service life of a pulpless unit largely depends on the quality of the dental canal filling by the dentist. Mistakes made by the doctor during the procedure can lead to various complications: dental cyst, fistula or gumboil. In this case, the unit cannot be saved. In order to minimize the risk of unpleasant consequences, the doctor must follow a clear algorithm for performing work to remove nerve endings. The patient, in turn, must regularly carry out hygiene measures (2 times a day) and visit the dentist at least once every 6 months.