31/10/2021
Many people associate going to the dentist with something unpleasant, painful and terrible. Therefore, people often postpone treatment until the moment when the tooth hurts so much that the pain becomes impossible to bear. Indeed, in Soviet times, anesthesia was a “weak link”, and many manipulations were carried out without pain relief at all. But over the past 15 years, dentistry has come a long way. And now treating various diseases of the oral cavity is not painful at all. Modern anesthesia eliminates not only physical pain, but also reduces the patient’s psycho-emotional stress, which significantly increases the effectiveness and quality of treatment. All dental procedures are absolutely painless, be it caries treatment or implant installation.
Indications
Most dental procedures are performed under local anesthesia.
Its use is mandatory in the following cases:
- Treatment of pulpitis (first visit)
- Periodontal operations (closed and open curettage, gingivoplasty, elimination of gum recession, guided tissue regeneration)
- Prosthetics of vital (living) teeth with fixed structures (crowns, inlays, onlays, bridges)
- Tooth extraction, implantation, bone tissue augmentation, tooth-preserving operations (apex resection, root amputation, hemisection), making incisions for periostitis, pericoronitis, opening abscesses and phlegmons, removing cysts and tumors
In some situations, anesthesia is mainly used, but patients with reduced sensitivity can do without it:
- Treatment of caries, wedge-shaped defects, non-carious lesions, periodontitis
Procedures that most often do not require anesthesia, but particularly sensitive patients may require:
- Professional oral hygiene
- Restoration of pulpless teeth (both fillings and crowns or inlays)
- Removable prosthetics (if the gag reflex is increased, there may be a need for mucosal anesthesia)
Anesthesia is not recommended:
- Oral examination
- Preventive measures (fluoride varnish applications, fissure sealing)
- Teeth whitening
- Orthodontic treatment
Children often tolerate tooth preparation for caries much easier than an injection into the gum. Therefore, you should not necessarily give an injection on your first visit before starting treatment. It makes more sense to try drilling without anesthesia and switch to it only if the child complains of pain. Compassionate parents, do not worry that your child may experience hellish pain and refuse further treatment. Dentin sensitivity in children is less than in adults. The likelihood of getting psychological trauma from an injection is higher.
Diagnostic local anesthesia is used to identify the diseased tooth. When several adjacent teeth are severely damaged, it is difficult for both the patient and the doctor to determine the source of pulpal pain. In order not to depulpate them all, you can give one anesthesia and wait. If the pain has passed, it should be treated first; if not, anesthetize the next tooth and check the reaction.
Types of local anesthesia in dentistry
Superficial (application) anesthesia
It is carried out by spraying, irrigating or lubricating the mucous membrane with a topical anesthetic (most often lidocaine). The main advantage is that it is painless (no injection is required). However, it is only effective for soft tissue anesthesia. It does not reduce tooth sensitivity at all. Therefore, the use of only superficial anesthesia in the treatment of small carious cavities or ultrasonic teeth cleaning is unjustified.
Often used to reduce pain before an injection.
Application anesthesia helps patients with an increased gag reflex (when taking impressions, for example).
To remove mobile baby teeth in children, superficial anesthesia is sometimes sufficient, but if the roots have not yet completely resolved, then such anesthesia is not enough - infiltration anesthesia is necessary.
Lubricating with ointment is preferable to spraying with a spray because it is easier to control the area of application. When splashed, the anesthetic can get onto the soft palate, creating discomfort and additional anxiety for the patient in terms of difficulty breathing (choking).
Infiltration anesthesia
It is carried out by injecting an anesthetic drug into the place whose sensitivity needs to be reduced. The anesthetic solution from the injection point spreads to nearby tissues (including dental nerves), temporarily eliminating pain and other sensations. When treating teeth, infiltration anesthesia is applied to the projection of the apexes (where the nerves enter the canals of the tooth). This type of anesthesia is preferred for the upper and lower anterior teeth. For lower chewing teeth, infiltration anesthesia is ineffective (due to the thick and dense bone tissue in this area).
The safest injection method of all. Possible minor complications include hematomas (bruises) and stomatitis at the injection site.
When anesthetizing single-rooted teeth (incisors and canines), one injection on the cheek side is sufficient. Multi-rooted teeth (molars and some premolars) require injections on both sides: buccal (labial, vestibular) and palatal (lingual on the lower jaw). On the palatal side, the injection is more painful than on the buccal side (since the mucous membrane of the palate is denser, and the injected solution injures the soft tissues more).
With periostitis, abscess and other acute inflammatory processes in soft tissues, the effectiveness of infiltration anesthesia decreases, and the pain of the injection increases. In such situations, conduction anesthesia is indicated.
Conduction anesthesia
It consists of blocking the sensitivity of the entire nerve trunk by introducing an anesthetic to the place where it exits the jaw to the surface. In this case, several teeth can be treated at once.
There are the following subtypes of conduction anesthesia in dentistry: mandibular and torusal (the lower teeth on one side are anesthetized), mental (lower premolars, canines and partially incisors), palatal (upper teeth on the palatal side), incisive (upper incisors and canines on the palatal side) , tuberal (upper molars on the buccal side), infraorbital (upper premolars and canines on the labial side).
Conduction anesthesia is not always successfully performed by the dentist. You have to do it again from time to time. Due to the technical complexity of the implementation: the doctor does not see the nerve trunk, the needle is brought to the average location of its location in the anatomical atlas, and a particular patient may have individual (quite different from the standard) anatomical features. The introduction of an anesthetic at a considerable distance from a large nerve does not allow achieving a complete block of sensitivity.
Even worse is a direct needle hit on a nerve during conduction anesthesia. In addition to sharp pain (as patients describe it - “electric shock”), subsequent loss of sensitivity is possible. Most often, mandibular or torus anesthesia is performed, so paresthesia of the tongue and lower lip (one half) is most common. Tingling, loss of taste, and discomfort may last for several weeks or months. Usually, sensitivity returns on its own without any manipulation, but in rare cases, paresthesia remains for life.
Therefore, conduction anesthesia is not recommended when safer infiltration can be used.
Intraligamentary anesthesia
It is carried out by injecting the drug into the periodontal ligament (located between the alveolus and gum on one side and the tooth on the other). To completely remove the tooth, several injections are required around the perimeter. Only one tooth is numbed. Effective for all teeth, but extremely painful. It is recommended to use it after preliminary infiltration anesthesia.
If the anesthetic is administered excessively, necrosis of the periodontal ligament (with subsequent tooth loss) is possible. If anesthesia is used to remove a tooth, this problem is irrelevant.
Intrapulpal anesthesia
It is carried out by injecting an anesthetic directly into the pulp of the tooth in case of pulpitis. This injection is very painful, so it is given only after preliminary infiltration, conduction or intraligamentary anesthesia. The tooth is still pre-drilled (otherwise you won’t be able to get to the pulp). The effectiveness is close to 100%, the analgesic effect does not last long, but usually this period of time is enough to remove the pulp.
Apart from pain, there are no complications.
Intraosseous anesthesia
It is achieved by introducing an anesthetic into the bone tissue surrounding the tooth after its perforation. Preliminary infiltration or conduction anesthesia is required. Due to the technical complexity of implementation, it is rarely used. Only if other types of local anesthesia have failed. About 90% effective, can block multiple teeth.
Modern methods and instruments of local anesthesia in outpatient dentistry
The problem of pain and anesthesia in dentistry remains very relevant to this day [1].
Most dental interventions without adequate pain relief are accompanied by pain of varying severity, up to intense pain. In the future, this may provoke fear of visiting the dentist, which, in turn, may lead to the patient’s delay in seeking dental care.
Modern technologies of local anesthesia include the use of carpule technology, an alternative to which currently does not exist [2].
An important component is local anesthetic solutions and instruments, which include both traditional dental syringes for carpules and computerized systems.
The effectiveness and safety of pain relief depend not only on the anesthesia technique, but also on the correct choice of local anesthetic, based on the characteristics of its pharmacokinetics and pharmacodynamics, the presence of a vasoconstrictor, and the concentration of these components. A wide range of modern drugs based on articaine creates the opportunity for an informed choice of anesthesia, allowing for adequate pain control during dental interventions with minimal risk of possible complications. The main advantage of articaine-containing anesthetics is that they diffuse better into the tissue at the injection site, act faster and last longer, have a larger zone of anesthesia and low toxicity [3].
The widespread use of these drugs in dental practice has made it possible to expand the indications for the simplest and safest methods, which include infiltration and its variety, periodontal, anesthesia [4].
The beginning of the 21st century in dentistry marked the emergence of new technologies, among which were computer syringes [b].
At the Department of General Dentistry and Anesthesiology of the FPDO, clinical trials of syringes “Wand”, “Anaject”, “QuickSleeper”, “STA-system” were carried out, which showed a number of advantages of automated injectors over traditional ones. Among them were such as automation of the aspiration test, slow supply of anesthetic under constant pressure controlled by a computer, precise dosing of the amount of anesthetic administered, disposable systems for each patient, etc.
On the basis of the dental department of Federal State Budgetary Institution No. 2 of the Ministry of Economic Development of the Russian Federation (department head L.M. Vyalushkina), we conducted a clinical trial of the STA system (USA), which was specially designed for periodontal methods of anesthesia. An important distinguishing factor of this system is the presence of a voice training mode that communicates the sequence of actions; double needle rotation function, preventing needle deviation during injection; constant visual monitoring of pressure and anesthetic supply.
As mentioned earlier, an important component of local anesthesia is the aspiration test, which, unfortunately, many doctors neglect or cannot perform due to a poor-quality carpule syringe. Thanks to automated aspiration, the STA system fully justifies its safety, since the medium is always taken from the injection site, informing the doctor about it.
We performed 30 anesthesia in patients with a high level of personal anxiety according to Spielberg, who separately indicated during the survey their fear of injections using the BTA system, and in 30 patients with a high level of personal anxiety according to Spielberg without fear of injection with a conventional carpule syringe.
To assess the functional state of patients and their level of anxiety before dental surgery, a special questionnaire was developed, the first page of which corresponded to the standard questionnaire included in medical records at the initial visit with the addition of items about blood pressure, its indications and decrease (increase) if necessary, as well as notification of informed consent to participate in the study.
The second sheet contained the Spielberg test to determine personal anxiety before and after treatment. The third sheet was asked to be filled out by the doctor, where blood pressure and heart rate were recorded before and after anesthesia, diagnosis, amount of anesthetic, its type, duration of anesthesia and the speed of its onset, as well as the zone of anesthesia and assessment of the effectiveness of pain relief using an analogue-visual scale developed at the Department of General Dentistry practice and anesthesiology FPDO MGMSU.
Using this method, 20 teeth were treated for caries, 31 teeth were treated for pulpitis, and 7 teeth that could not be treated were removed.
The effectiveness of STA - intraligamentary anesthesia on an analogue-visual scale was 95% when using 4% articaine-containing anesthetic with epinephrine 1:200000 for the treatment of caries, 96% in the treatment of pulpitis and periodontitis and 98% when removing teeth on both jaws.
The heart rate on average did not exceed 80 beats per minute before treatment in the first group (62%) before anesthesia; after treatment there was a slight decrease to 73-76 beats per minute (47%). In the second group, no statistically significant changes in heart rate were observed before and after the injection.
It should be noted that when performing local anesthesia using the STA-system, there is no collateral numbness of the cheek, lip and tongue, which is often perceived negatively by patients with a high level of anxiety.
The STA system provides constant audio and visual feedback by guiding the needle tip into the periodontal ligament. As it is achieved, the dentist hears a voice pronouncing the abbreviation “PDL”, meaning the correct placement of the needle.
In this way, injury to the periodontal ligament associated with increased pressure is eliminated, since the dentist is constantly in visual-auditory communication with the syringe. Thus, summarizing the experience of working with the STA system, we can note the high efficiency while ensuring the complete safety of this device, which, in turn, allows us to recommend it for use in dental practice.
Literature. 1. Rabinovich S.A., Lukyanov M.V., Moskovets O.N., Zoryan E.V. Modern methods of pain relief based on articaine-containing drugs. Guidelines. - M., VUNMC, 2002. 2. Rabinovich S.A. Modern technologies of pain relief in outpatient dental practice: dis. ...doctor. honey. Sci. - M., 2000. 3. Malamed SF Handbook of local anesthesia. 4th ed. St. Louis: Mosby, 1997. 4. Bizyaev A.F., Ivanov S.Yu., Lepilin A.V., Rabinovich S.A. Anesthesia in a dental clinic. - GOU VUNMC Ministry of Health of the Russian Federation, 2002. 5. Egorov P.M. Local anesthesia in dentistry. - M., 1985. 6. Allen R. Heifer, DDS, MScD. Profound anesthesia made easy with the STA System. Endo Tribune | November, 2008.
Instruments for local anesthesia
The injection requires a syringe, a needle and a local anesthetic solution.
For several decades now, in dentistry, instead of disposable syringes, a reusable carpule syringe has been used. A disposable anesthetic cartridge and a disposable needle are inserted into it. They are used once, and the metal syringe itself is sterilized after each patient. Reuse of an incompletely used carpule is prohibited, since during the injection a reverse flow of blood or other liquid through the needle into the carpule is possible (there is a risk of infection of the next patient).
A special syringe gun is available for intraligamentary anesthesia. The same needles and carpules are inserted into it as into a carpule syringe. It allows you to more accurately dose the volume of anesthetic for a given type of anesthesia (but it is also possible to perform intraligamentary anesthesia with a regular carpule syringe).
The thickness of the needles used in carpule syringes is 0.3-0.5 mm. This is much thinner than disposable syringes (therefore the injection is much less painful). Length – 8-30 mm. For mandibular and torusal anesthesia, longer and thicker needles are used than for infiltration. To carry out intrapulpal and intraligamentary anesthesia, the needle can be bent (it does not break).
Carpula is a sealed glass cartridge with a rubber plunger. In dentistry, in most cases, the anesthetic solution, in addition to the anesthetic drug itself, contains a vasoconstrictor - a vasoconstrictor component that prevents the rapid elimination of the anesthetic through the general bloodstream. This is adrenaline (epinephrine). Its concentration is negligible - 1:100000 or 1:200000. When manually drawing such a mixture into a disposable syringe, add 1 drop of adrenaline to the anesthetic solution. However, the size of a drop is such a relative value that the concentration of this very active component can differ tens of times in different syringes. This creates many complications, even life-threatening situations for the patient.
The introduction of carpules with precise industrial dosages of components has greatly reduced the number of such complications. However, it should be noted that different manufacturers have different attitudes towards maintaining strict dosages of their own carpules. For the product of the Russian pharmaceutical industry, Brilocaine (manufacturer: Bryntsalovskiy Ferein), the anesthetic effect of two capsules from one package can be radically different: from complete absence of pain relief to super strong (“my legs froze,” according to the patient). Although the packaging states exactly the same ingredients as imported Ultracain, Ubistezin or Septanest.
Anesthetics with low vasoconstrictor dilution 1:200000
Indicated for most outpatient interventions in pediatric dentistry. 4% articaine 1:200000 provides anesthesia for soft tissues for 180 minutes and dental pulp for 45 minutes, which satisfies the protocol for most outpatient interventions.
Currently, anesthetics based on 4% articaine with epinephrine 1:400000 have appeared in European countries. They provide anesthesia for dental pulp tissue for 20 minutes and soft tissue for 1 hour. This anesthetic provides the duration of anesthesia required by the doctor and a short period of “numb” tissue, which is so important for pediatric patients. Currently, these anesthetics are not certified in the Russian Federation, but work is underway to introduce them into domestic dentistry.
It is also worth noting that there is no difference in the depth of anesthesia and effectiveness between anesthetics with vasoconstrictors 1:100000, 1:200000 and 1:400000. There is a difference only in the duration of local anesthesia of the dental pulp: 25, 45 and 75 minutes, respectively. Many dentists mistakenly divide anesthetics into “strong” (1:100,000) and “weak” (1:200,000). This statement is misleading.
For short-term interventions in children with concomitant pathologies, the use of anesthetics without a vasoconstrictor is indicated. However, their use does not guarantee complete safety and does not reduce the risk of complications. It is worth noting some of their pharmacological features. Vasoconstrictors are added to the local anesthetic solution not only to increase the duration of pain relief, but also to reduce their toxicity. The fact is that all anesthetics have a vasodilating effect and undergo fairly rapid absorption into the bloodstream. The addition of a vasoconstrictor slows the absorption of the anesthetic and prolongs its action. When using an anesthetic without vasoconstrictors, this effect does not occur. The anesthetic is forced into the blood, which can lead to a toxic reaction. This complication is possible if the permissible dosage is exceeded, which is different for anesthetics with and without a vasoconstrictor. In summary, it should be noted that anesthetics without a vasoconstrictor do not affect the functioning of the cardiovascular system, are less allergenic since they do not contain preservatives, but due to accelerated absorption they are toxic and safe to use only if the dosage is observed.
Local anesthetics
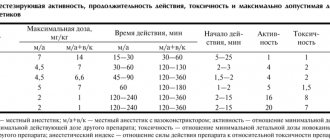
In Russia, 4 types of anesthetics are most widely used: novocaine, lidocaine, articaine and mepivacaine.
Novocaine (procaine) was synthesized in 1905 and became widespread throughout the world as the first non-narcotic anesthetic. It is a basic reference point - all subsequent anesthetics are compared in terms of effectiveness and toxicity with novocaine, whose indicators are taken as one. After the introduction of lidocaine, it lost popularity in developed countries. There is a high frequency of allergic reactions to novocaine.
Lidocaine was invented in 1943. Its effectiveness turned out to be 4 times higher than that of novocaine (with only twice the toxicity). Widely distributed throughout the world (1st place in the number of injections among anesthetics in the USA). However, like novocaine, it has a relatively high percentage of allergic reactions (including the development of anaphylactic shock). In addition, it is often used with increased concentrations of the vasoconstrictor 1:50000 and 1:25000, which increases its effectiveness, but increases the number of complications from the cardiovascular system. Indicated for pregnant women - FDA category B (see article Use of local anesthetics for dental treatment during pregnancy; safety for women in labor).
Articaine was synthesized in 1969. It began to be used in Germany, where it was registered under the commercial name "Ultracaine". This name of the drug is now no less popular than articaine, although it represents the product of only one, “Septanest”, “Alfacaine” and several other commercial names - this is the same as “Ultracaine”. The most common local anesthetic in Europe and Russia (it was approved in the USA only in 2000, 10 years later than here). 5 times more effective than novocaine. 1.5 times more toxic. According to the FDA classification, it is classified as category C.
Mepivacaine was developed in 1957. It is equivalent in effectiveness to lidocaine and inferior to articaine. It is noteworthy that, despite category C, it is often used for pregnant patients, due to the permission of non-adrenaline release forms (lidocaine and articaine carpules are sold only with a vasoconstrictor). Although in fact it is not the first choice drug for expectant mothers (see the article Is it possible to do local anesthesia during pregnancy?).
Adrenaline , also known as epinephrine, is not a local anesthetic, but is used in the vast majority of cases for dental injections. By narrowing the blood vessels, it helps preserve the anesthetic depot at the injection site, reduces its toxic effect on the body, and also reduces bleeding (which improves visibility during surgical procedures). Its use in pregnant women and patients with cardiovascular diseases (paroxysmal ventricular tachycardia, atrial fibrillation) is undesirable. Use with caution in patients with arterial hypertension, diabetes mellitus, and hyperthyroidism.
In addition to the anesthetic and vasoconstrictor, the solution may contain preservatives (methylparaben) and adrenaline stabilizers (sodium pyrosulfite). Both methylparaben and sodium pyrosulfite (metabisulfite) have a high frequency of allergic reactions, including the most dangerous - anaphylactic shock. This risk is significantly higher than that of the anesthetics themselves (and in principle there cannot be an allergic reaction to adrenaline). Therefore, methylparaben was completely abandoned in carpules - it is needed only when using large containers for preserving an unused solution after opening the ampoule. Sulfites are necessary to prevent the oxidation of adrenaline - they cannot be abandoned in carpules with a vasoconstrictor. Therefore, anesthesia without adrenaline is recommended for patients with multivalent allergies. The frequency (up to 5%) of sulfites provoking an attack of bronchial asthma is high, so anesthesia with adrenaline is also not recommended for asthmatics.
Injection equipment for local dental anesthesia ru:12659
Injection equipment for local dental anesthesia The safety and effectiveness of local anesthesia in dentistry primarily depends on the equipment used for injection.
Injection equipment must meet the following requirements:
Cause minimal trauma to the patient.
Accurately deliver the anesthetic solution to the destination and create an anesthetic depot.
Precisely dose the anesthetic (up to 0.1 ml).
In dentistry today, various syringes are used that make it possible to perform both traditional anesthesia and intraligamentary, intraosseous, needle-free jet anesthesia, etc.
The injector most suitable for the use of modern carpule anesthetics is the carpule syringe.
Reusable carpule syringes are made of metal (stainless steel, titanium, etc.). We have also mastered the production of plastic carpule syringes - disposable and reusable.
The carpule syringe should be:
compatible with needles from different companies;
strong enough to administer anesthetics under pressure;
have an aesthetic appearance, be simple and convenient to use with one hand;
ensure an aspiration test.
A metal carpule syringe consists of a body 1 and a rod 2, which can have different shapes. As a rule, the body is cylindrical in shape with a window and has a side groove 4 (for placing the carpule). On the body there is a removable tip with nipple 3, with a thread for fixing (screwing on) the needle, two holders 6 (for the index and middle finger of the right hand) The holders can be either flat or in the form of rings. Rod 2 is made in the form of a rod with a plunger 8 at one end and a holder (ring) 7 (for the thumb of the right hand) at the second. The plunger can be in the form of a harpoon or “fungus”, or a hook and provides fixation of the carpule piston plug to ensure its reverse motion during an aspiration test.
If an anesthetic is accidentally introduced into a vessel, the toxicity of the anesthetic solution increases 10 times or more (especially if there is adrenaline in the anesthetic solution), and the patient experiences a general toxic reaction. Therefore, to prevent intravascular injection of an anesthetic, an aspiration test (test) is performed: before injecting the anesthetic solution, the syringe plunger must be pulled towards you. If the aspiration test is positive, you need to pull back the needle, then push it forward again.
Selecting a carpule syringe:
The injector should be simple and easy to use with one hand (the holder for the thumb of the right hand should be in the form of a ring).
There should be a window on the injector body to monitor the use of anesthetic and aspiration sample.
There should be a plunger at the end of the syringe plunger for performing an aspiration test.
The removable tip must have a threaded nipple for fixing different needles and the “American system”).
A cartridge syringe from Truewin Industries (Pakistan) meets all these requirements. The syringe is intended for local anesthesia in dentistry. The design of the syringe allows you to press on the rod and pull it back during aspiration with one hand. Truewin Industries Syringe Optimizes Aspiration Sample with Dual Locking Ring
The kit includes 2 replaceable nozzles for carpule needles according to American and European standards. To replace the carpule, it is necessary to pull the pusher back to its original position.
Very simple, reliable design, three ring-shaped finger grips. Made from particularly light alloy. Its coating is resistant to corrosion. The convenience of using this syringe lies in the fact that the anesthetic cartridge is installed into it very simply. Compatible with all standard cartridges (1.8 ml) with rubber piston. The rotating cartridge holder allows you to see the cartridge in any situation, especially when performing an aspiration test or monitoring the volume of injected solution. Simple disassembly of the syringe makes it easy to clean and sterilize the instrument.
Preparing the carpule syringe for use:
Sterilization of the injector in disassembled form (in an autoclave or in a dry-heat sterilizer, or “cold” sterilization). Sterilization by chemical means is carried out by complete immersion in a solution.
Sterilization of carpules. The carpule is wiped with gauze soaked in a 70° alcohol solution. It is necessary to properly process the rubber plugs.
The cartridge is inserted into the injector body
Press the injector piston so that the plunger is securely fixed in the piston plug of the carpule for carrying out an aspiration test
Select a sterile removable tip so that the thread of its nipple matches the thread of the desired needle. Remove the plastic cap from the rear (short) end of the needle and insert it into the nipple hole, at the same time screw the needle cone onto the injector nipple
Remove the plastic cap from the long end of the needle, pressing the syringe plunger, check the patency of the needle (drops of anesthetic appear at the end of the needle). The carpule syringe is ready for use
To carry out effective intraligamentary (infiltration) and intrapulpal anesthesia, special injectors are used, which create high pressure during injection. They also have a dispenser that ensures that a precisely defined amount of anesthetic is introduced into the tissue when pressing on the syringe lever.
Truewin Industries (Pakistan) injector, shaped like a pistol
This is a universal injector for all types of infiltration anesthesia with minimal doses of anesthetic, using a standard cartridge. Injects a small amount (on average 0.2 ml) of anesthetic per “click”, allowing for a slow, atraumatic injection. One injection is sufficient for intraligamentary anesthesia. Made from high grade stainless steel
The injector kit includes:
two removable tips for different types of carpule needles (European and American systems);
a protective cylinder for the carpule (made of plastic), it is put on the carpule before injection to prevent injury to the patient from glass fragments in case of possible rupture of the carpule during injection.
Preparing the injector for anesthesia:
The injector, replacement tips, protective cylinder and cartridge are sterilized.
A protective cylinder is put on the carpule and inserted into the removable tip (the thread of the nipple of the removable tip must correspond to the type of carpule needle - European or American system).
Screw the needle body onto the nipple of the removable tip, which, in turn, is fixed in the injector body.
Remove the plastic cap from the end of the needle, press the lever (trigger) - drops of anesthetic appear at the end of the needle. The injector is ready for use.
The shape of the injector is very convenient for anesthesia. One injection (0.2 ml of anesthetic) is sufficient for intraligamentary anesthesia into dense dental gums, and 0.4 ml of anesthetic (2 injections) qualitatively anesthetizes a single-rooted tooth with paraapical administration of the drug under the periosteum.
Needles for carpule syringes
Advances in science have led to needles becoming strong, flexible and sharp. These are disposable needles, which reduces the risk of infection entering the body and cross-contamination of the patient(s).
The carpule needle consists of a metal needle itself and a plastic connecting coupling (cone). The long end of the needle (for introducing anesthetic into the tissue) ends with a cut, the short end serves to pierce the carpule plug. The sharpness of the final cut of the needle allows you to minimize the pain of the injection.
The best companies put a mark (dot) on the outside of the cone with red paint on the cut side of the needle tip, which allows better orientation during anesthesia (when directing the cut of the needle to the bone).
Needles are divided by length into “long” (from 28.9 to 41.5 mm) and “short” (from 10 to 25.5 mm). Most companies produce standard needles with lengths of 12, 16, 25, 35, 38 mm
On the inside of the plastic cone there is a thread for screwing the needle onto the carpule syringe. The size (shape) of the cone depends on the type of needle: “European system” or “American system”.
Length, diameter of carpule needles in European and American systems:
Carpule needles are placed in a plastic case. During sterilization, a paper seal or control cut is applied, which seals the package. Needles are packed in a box of 100 pieces. The label indicates the name and address of the company, the type of needle, its length, the outer diameter (number) of the needle, the date of manufacture, and the shelf life. For example: 0.30x21 mm (diameter and length of the needle), 01.2015 (shelf life), Sopira (name of the manufacturer).
The use of carpule needles provides high-quality local anesthesia with minimal pain. It is better to buy needles in batches (packages). It is recommended to use needles only from well-known companies that guarantee high quality products.
A new brand in the field of dental anesthesia - SOPIRA needles (Heraeus Kulzer) - is a combination of many years of experience with the latest developments.
Precision, functionality and reliability are the high standard for SOPIRA carpule needles. The needles are characterized by first-class steel and an innovative needle cut. This solution meets all the requirements of a wide range of forms of dental anesthesia.
A special silicone coating makes it easier for the needle to penetrate the tissue.
Plastic connector with thread and needle bevel orientation indicator allows you to select the optimal direction of needle entry into tissue during injection
The triangular bevel of the needle tip helps reduce pain during injection.
The needles are compatible with all types of dental syringes on the dental market
The use of carpule needles from little-known and dubious companies can lead to complications (possible needle obstruction; fracture near the needle cone during anesthesia). In addition, the needle may not be sharp enough, which will lead to severe pain during the injection and injury to the periosteum.
The commercialization of the activities of dentists is increasingly increasing the requirements for anesthesia. In recent years, effective anesthesia has become a kind of calling card for a private practitioner. The complex that makes up the modern technology of local anesthesia, providing the dentist with effective and safe actions, is:
reliable modern anesthetics and vasoconstrictors
effective methods of local anesthesia
knowledge and practical skills on the full range of issues related to local anesthesia
reliable and convenient instruments (syringes and needles)
#Anesthesia
Ukr-Medmarket 5712 • 01/20/2015
+ Add article
Physiodispenser micro-nx impla-nx led
44,000 UAH $ 1554.77 • € 1368.58
Oles • KolomyiaMore details
Local anesthesia in pediatric dentistry
Local anesthesia is not recommended for young children under 2-4 years of age. Even if it is possible to fraudulently persuade a child to take an injection, after it, as a rule, he will no longer open his mouth for further treatment. Up to 6-7 years of age, the optimal method is infiltration anesthesia (including for the treatment of lower teeth). At this age, the lower jaw is not yet so dense and there is no need for conduction anesthesia. Of the drugs for children, the optimal choice would be articaine with a low adrenaline content of 1:200000 - since long-term manipulations are still contraindicated for children (they quickly get tired of the treatment), there is no need for long-term pain relief for many hours.
Features of pain relief for permanent teeth
Treatment of permanent teeth in children certainly requires pain relief. The choice of pain relief method depends primarily on the child’s age and degree of development. Difficulties in pain relief usually arise in the treatment of mandibular molars, which is due to varying degrees of development of the cortical layer of the bones of the facial skeleton. In most cases, when treating uncomplicated caries of permanent teeth of the lower jaw in children under 12 years of age, infiltration anesthesia is sufficient. In children over 12 years of age, infiltration anesthesia is effective only in the area of incisors and premolars.
To treat the canines of the lower jaw in children over 12 years of age, mandibular anesthesia or mental anesthesia should be performed, the volume of injected anesthetic is 0.6-1 ml. For the treatment of first molars with short-duration interventions (15-20 minutes), infiltration buccal anesthesia is effective, with the volume of injected anesthetic being 0.6-1 ml. Infiltration anesthesia of the second molars of the lower jaw is not so effective; in most cases, complete anesthesia of the pulp tissue is possible only with the use of conductive mandibular anesthesia.
There are some peculiarities in conducting conduction methods of anesthesia of the lower jaw. First of all, their implementation must be justified from the point of view of nosology and the method of treatment chosen by the doctor. If possible, conduction methods of anesthesia should be avoided and preference should be given to safer infiltration techniques.
There are studies confirming that the diameter of the needle does not affect the reduction in the degree of pain of the anesthesia.
Mandibular anesthesia in children of different ages is carried out according to different intraoral landmarks. This is due to the different position of the mandibular foramen in relation to the occlusal plane of the teeth.
In children under 6 years of age, the mandibular foramen is located below the occlusal surface, so the needle is inserted at the level of the occlusal surface. Accordingly, in children 6-10 years old, the needle is inserted 5 mm above the occlusal surface, and only in children over 10 years old, mandibular anesthesia is carried out by analogy with adults. When performing mandibular anesthesia, an aspiration test should be performed in all cases to reduce the risk of intravascular injection of anesthetic. The anesthetic should be administered slowly.
Mental anesthesia is carried out taking into account the period of development of the dental system. Compared to adults, the mental foramen in children is located significantly anteriorly: in children under 4 years old - in the area of temporary canines, in children 4-6 years old - in the area of the first temporary molar.
Other methods of pain relief. In addition to conduction and infiltration methods of pain relief, which have already become traditional, periodontal and intraosseous techniques are now becoming increasingly widespread in dentistry. However, the question of the safety of their use remains open. In particular, when performing intraligamentary anesthesia, the distribution of the anesthetic passes through the cancellous substance of the jaw bones, reaching the periapical region. The vasoconstrictor has a long-term vasoconstrictor effect (Brannstrom M., Lindskog S., Nordenvall KJ, 1984; Tagger E., Tagger M., Sarnat H. 1994), the safety of which has not been studied for teeth during their formation.
Intraosseous anesthesia is not indicated for use in pediatric dentistry. There is a danger of injury to the tooth buds and the negative impact of the vasoconstrictor on the growth zones of periapical tissues. Also, the vibration and noise of the intraosseous injector can frighten the child or, even worse, provoke sudden movements that can lead to injury from the rotating elements. The author does not recommend intraosseous anesthesia in pediatric practice, although there are studies in the literature about their “highest” effectiveness in children (Sixou JL, Rogier ME, 2006).
If possible, conduction methods of anesthesia should be avoided and preference should be given to safer infiltration techniques.
However, the above methods cannot be completely denied in the treatment of permanent teeth with formed apices. In particular, the effectiveness of intraseptal, intraosseous and intraligamentary anesthesia in the treatment of mandibular molars is high (Medvedev D.V., Petrikas A.Zh., Tazova O.E., 2010; Petrikas A.Zh., Yakupova L.A., Medvedev D.V., 2010).
These techniques can be used as an independent method of pain relief for short interventions lasting 15-20 minutes. They can also be used additionally if the initial anesthesia is insufficient: treatment of acute pulpitis of the mandibular molars (Anisimova E.N., Rabinovich S.A., Butaeva N.T., 2013; Makeeva I.M., Erokhin A.I., Kuzin A.V., 2012), incorrect choice of anesthetic, the effect of which has expired.
The effectiveness of local anesthesia
The success of deep anesthesia depends on the anesthetic, the concentration of the vasoconstrictor, the type of anesthesia, the dose of the drug, the qualifications of the dentist and the individual response of the patient. 4% articaine with an adrenaline concentration of 1:100000 is the most effective. Conduction anesthesia provides better pain relief than infiltration anesthesia, but requires a more highly qualified doctor. (However, even the most experienced specialists have a certain percentage of failures). The patient's agitated panic state and prolonged pain tolerance for several days before the visit reduce the effectiveness of local anesthesia. Alcohol and drugs - even more so.
Dosage
The volume of one carpule is 1.7-1.8 ml. This amount is enough for most manipulations within one or two teeth. When treating a larger number of teeth (especially if they are located far from each other), several carpules and injections into different parts of the oral cavity are required.
A second injection of anesthetic into the same place is carried out if the first one is unsuccessful or after some time, when long-term treatment has not yet been completed and the anesthesia begins to wear off. The introduction of the same drug can help if conduction anesthesia is ineffective the first time. With other types of anesthesia, it is necessary to change the anesthetic itself to a more powerful one. It is impossible to increase the volume of the injected solution indefinitely - in case of an overdose, a toxic reaction occurs. For articaine with adrenaline and lidocaine with adrenaline, the maximum dose is 7 mg/kg body weight. One carpule (1.7-1.8 ml) contains 34-36 mg of 2% lidocaine or 68-72 mg of 4% articaine. Therefore, for a person weighing 70 kg, the maximum number of carpules at one time is: 14 for 2% lidocaine and 7 for 4% articaine.
Features of pain relief for temporary teeth
Of course, the choice of pain relief method depends on the planned intervention.
In the treatment of caries and pulpitis of temporary teeth, preference is given to infiltration methods carried out from the vestibular (buccal/labial) side, and there is no need for lingual or palatal anesthesia. This is explained by the predominance of spongy substance and a large number of nutrient openings in the structure of the jaw bones, facilitating the diffusion of local anesthetic.
In order to reduce the degree of pain of the injection and increase the level of comfort for the child, the following recommendations for local anesthesia should be followed:
- A preliminary distracting preparatory conversation with the child is necessary, during which the doctor uses terms that the child understands. In this case, the words “injection”, “syringe”, “anesthesia”, “removal”, “needle” are not pronounced.
- The child should not see (look at) the injection equipment. All instruments are presented by an assistant out of sight of the child.
- Application anesthesia should be performed so that the child does not feel the puncture stage of the mucous membrane.
- The rule must be observed: “one needle, one injection.” If the needle accidentally comes into contact with the bone tissue of the jaw, its tip is deformed; as a rule, it bends in the direction opposite to the bevel. A repeated injection with the same “dull” needle in another segment will involve applying pressure that is unpleasant for the child.
- The anesthetic should be injected slowly, 1 ml/min. Forced administration of the anesthetic leads to hydrodynamic tissue trauma, which causes pain.
- Two-stage injection of a portion of anesthetic. When performing infiltration anesthesia, the doctor initially injects a small amount of anesthetic? 0.1 submucosally, while a zone of tissue infiltration the size of a millet grain is visually determined. Next, the doctor talks with the child for 2-3 minutes.
- The subsequent administration of the main portion of the anesthetic is painless.
- The temperature of the anesthetic solution should be close to the child’s body temperature. To do this, do not store anesthetic carpules in the refrigerator. Before the injection, the doctor can “warm” the carpule in his hand or in running hot water.
The volume of injected anesthetic for infiltration anesthesia of temporary incisors and canines is on average 0.3 ml; for anesthesia of temporary molars, 0.5-0.6 ml is used. Subperiosteal anesthesia should not be performed as this will cause pain to the child and will not increase effectiveness. The needle should move submucosally towards the apexes of the roots of the teeth. In the upper jaw, when performing infiltration anesthesia, one should not insert a needle into the area of the frenulum of the upper lip, mucous strands in the area of temporary canines. These areas have an extensive network of nerves, providing hypersensitivity in these areas.
When performing an operation to remove temporary teeth of the upper jaw with a diagnosis of periodontitis, various combinations of infiltration methods are used. In the upper jaw, when removing incisors and canines, infiltration vestibular (0.5 ml) and incisal anesthesia (less than 0.2 ml) is used. In this case, classical conduction anesthesia with the advancement of the needle into the incisive canal is not carried out, but a certain amount of anesthetic is injected on the side of the incisive papilla, until signs of ischemia appear. If possible, painful incisal anesthesia should be avoided, which can be replaced with topical anesthesia or by inserting a needle into the vestibular interdental papilla and then moving it to the palatal side with a continuous supply of anesthetic.
The choice of dilution of the vasoconstrictor depends on the expected duration of the intervention and the presence of concomitant pathology in the child. As a rule, the duration of treatment for a child does not exceed 20-30 minutes.
When anesthetizing the first and second temporary molars, infiltration vestibular (0.5-0.6 ml) and palatal (0.2 ml) anesthesia is used. Palatal anesthesia can be replaced by the above-described approach through the interdental papilla. To reduce the degree of pain of local anesthetic injection into the hard palate, preliminary application anesthesia should be used.
When removing temporary teeth of the lower jaw with a diagnosis of periodontitis, a combination of conduction and infiltration methods is used. When removing incisors and canines, infiltration vestibular (0.3 ml) and lingual (less than 0.2 ml) anesthesia is used. Lingual infiltration anesthesia is performed in the area of the transition of the attached gum to the mobile mucosa of the floor of the mouth. The anesthetic is injected into the submucosal layer; the needle is not advanced to prevent intravascular injection. You can anesthetize the lingual mucosa by inserting a needle into the interdental papilla from the vestibular side and then moving it towards the lingual mucosa. When removing temporary first molars of the lower jaw, the above-described technique is used with the only difference that 0.5 ml of anesthetic is injected from the vestibular side of the tooth being removed. In the presence of local inflammation, it is necessary to perform conduction mental anesthesia. When removing the second temporary molars of the lower jaw with a diagnosis of periodontitis, either mandibular anesthesia (1 ml) or a combination of mental anesthesia (0.6 ml) and lingual infiltration (0.2 ml) is performed.
During the period of physiological change in occlusion, the removal of temporary teeth for orthodontic indications has some features. The most common mistake is removing a “moving” tooth under application anesthesia. The depth of application anesthesia is 2-3 mm of the mucous membrane, and the roots of the tooth may not be completely resorbed, and their removal will be painful. Application anesthesia can be used as an independent method only if the tooth is fixed by mucous membrane on one edge. In other cases, infiltration anesthesia should be performed. The anesthetic is administered before signs of gum ischemia appear; its volume is minimal.
Coming time
Intrapulpal and intraligamentary anesthesia begins to take effect within a few seconds. Application, infiltration, intraosseous - after 1-5 minutes. Conduction anesthesia is the most variable - from instant pain relief at the same second (if the needle hits the nerve) to half an hour. Sometimes patients, rising from the dental chair after completion of treatment, claim that “only now the freezing has really taken hold.”
Soft tissues are anesthetized before teeth. If the lip or tongue is already “frozen,” the teeth may still remain sensitive, and their premature preparation will be painful.
Validity
The duration of anesthesia also depends on the anesthetic, the concentration of the vasoconstrictor, the type of anesthesia, the dose of the drug, the qualifications of the dentist and the individual response of the patient. Conduction anesthesia lasts up to 2-3 hours or more. Some patients note that the anesthesia wears off completely only in the evening (if the treatment was carried out in the morning). But this is with a strong anesthetic, a high concentration of adrenaline, a significant dosage, and close contact with the nerve trunk. In other situations, conduction anesthesia may not last even one hour. Infiltration anesthesia lasts 1 hour or less. Other types are even smaller.