Conduction anesthesia is considered the most effective method of pain relief in dental practice. The essence is to block nerve impulses that are directly responsible for pain syndromes in the brain.
After the administration of the anesthetic, the pain threshold is reduced to zero. This allows the necessary operation to be carried out smoothly. The advantages of this method are good tolerability and high efficiency. In addition, after the intervention, the pain syndrome continues to remain at a minimal level.
Use in dental practice
An anesthetic drug is injected into an area located a short distance from the site where surgery will be performed.
Conduction anesthesia can be performed in one of two ways:
- Central. The doctor determines the main trunks of the nerve endings for subsequent administration of the medicine into one of them.
- Peripheral. The anesthetic is injected into one of the branches of the main nerve of the stem system.
High-quality pain relief involves delivery of the solution to its destination. We are talking about a canal - a bone opening through which the nerve ending passes.
Complications with local anesthesia.
During the process of local anesthesia, a pharmacological multicomponent drug enters the human body (into the injection area and into the general bloodstream).
Some of these components are vasoconstrictors (vasoconstrictors - catecholamines: epinephrine, vasopressin, norepinephrine, mesatone), in addition to local effects, they have undesirable general effects: they increase blood pressure, blood sugar levels, and increase heart rate. Such effects are especially unfavorable for patients with coronary artery disease, arterial hypertension, diabetes mellitus, pheochromocytoma, glaucoma, etc.
Other components of local anesthetics - stabilizers and preservatives - may be a risk factor in patients with an allergic predisposition (especially with severe forms of hypersensitivity, for example, Quincke's edema).
Advantages
The preference for using this method in dentistry is due to the following advantages:
- the ability to block sensitivity over a large area of the jaw for the alternate removal of several units of the dentition, opening purulent abscesses;
- the need to use a small amount of the drug compared to alternative methods of pain relief.
It is worth highlighting a number of advantages associated with minimizing the likelihood of complications:
- reduced risk of developing neuropathic syndromes;
- there is no possibility of the solution penetrating into the vessels;
- improving the quality of blocking the sensitivity of nerve endings;
- high efficiency for operations of any complexity.
Indications
Conduction anesthesia is performed before the following therapeutic measures:
- simultaneous extraction of several units of the dentition located in one area of the oral cavity;
- removal of tooth roots with inflammatory processes;
- removal of pathological teeth (for example, those that have grown into the gums);
- implantology (used for painless implantation);
- surgical intervention on the lower molars (molars);
- treatment of inflammation in the maxillofacial region;
- elimination of inflammation on mucous membranes and soft tissues;
- treatment of complex carious cavities;
- with intolerance to general anesthesia.
Maxillary anesthesia
- Palatal method. Allows you to completely block sensitivity in the palate area, making any manipulation absolutely painless. The action of the anesthetic spreads simultaneously to the alveolar process.
- Tuberal. This technique is used for operations or extraction of molars.
- Infraorbital. Suitable for treating canines, premolars, and incisors.
- Incisive. Anesthesia is injected into the mucosal area located between the incisors and canines.
Mandibular anesthesia
- Mental way. It is carried out for the treatment of premolars, incisors, and canines.
- Mandibular. It involves blocking all units of the dentition on the side where the drug is administered.
- Torusal. Involves the introduction of a solution into the roller of the movable jaw, called the torus. Allows you to block pain symptoms in the area of premolars, as well as molars.
There is another Bershe Dubov method. It is used for maxillofacial surgical interventions. Anesthesia applies to all elements on one side. The needle can be inserted intraorally or extraorally.
Restrictions
Before choosing a pain relief method, it is important to exclude contraindications. These include:
- some operations performed on patients under 12 years of age;
- disturbance of the psycho-emotional state in a pronounced form;
- skin diseases in the area of intervention;
- allergic reactions to antiseptics;
- patients with congenital deaf-muteness;
- inability to establish contact with the patient.
What are the dangers of local anesthesia?
Dental treatment and prosthetics under general anesthesia often becomes the source of many questions. Is it dangerous to use anesthesia in this way? Will this affect your health? Are fillings on several teeth worth artificially induced sleep? After all, each of us has heard that any general anesthesia is not without consequences for the human body. Moreover, local anesthesia seems to have been successfully used for dental treatment for a long time. Of course, we are horrified by the forced “heroism” of the Soviet people, who treated their teeth without any pain relief at all - with the exception of removal, when a drug was used that did not always act properly. People of that era, not only general anesthesia, even local anesthesia could be considered a luxury. This, by the way, explains the “genetic” fear of the dentist even among the children of those who lived in those days.
However, now, as it seems to us, there are practically no problems - any pharmacy chain in Moscow will offer local anesthetic drugs to choose from. It will be enough just to give an injection and the doctor will effectively treat your teeth without any pain. Isn't this enough? Why use general anesthesia for dental treatment? Many people believe that local anesthesia is much less harmless than general anesthesia. However, is the notorious “freezing” so harmless and does it really have no effect on our body?
However, local anesthesia only looks harmless. In fact, novocaine is combined with the hormone adrenaline to narrow the capillaries, which provides a long-lasting anesthesia effect. Adrenaline, in turn, causes an increase in heart rate, which is quite undesirable for those who suffer from cardiac problems. Both novocaine and other drugs that are its analogues can cause allergies. Also, local anesthesia can increase blood pressure or cause vasospasm. Of course, if the patient’s heart is fine, as well as his blood pressure, local anesthesia does not threaten such a person. However, where can one find an absolutely healthy person in the current ecology?
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment
If the patient has problems with the heart and blood pressure, then local anesthesia is simply contraindicated. And any conscientious dentist, before using local anesthesia, will definitely ask the patient about his state of health. And, most likely, having heard complaints about hypertension or heart problems, he will recommend general anesthesia instead of “freezing,” which will cause much less harm to the body.
Conduction anesthesia
Conduction anesthesia: definition, technique, indications, complications
Conduction anesthesia of the upper limb
What is conduction anesthesia
Conduction anesthesia is one of the types of anesthesia in which nerve transmission is blocked in the area of the body where the operation is planned, which results in complete immobilization and pain relief.
Synonyms for conduction anesthesia: nerve block, peripheral anesthesia, nerve anesthesia, brainstem anesthesia, nerve block, conduction anesthesia.
Conduction anesthesia is one of the types of regional anesthesia.
How does the patient feel during conduction anesthesia?
At the site of conduction anesthesia, the patient may experience various sensations. At the moment of puncture with a needle, there is either slight discomfort or some pain, the severity of which is no more than the pain felt when taking blood from a vein for a test. When a local anesthetic is administered, feelings of heaviness, bloating, and heat may occur in the anesthetized area. If no technical difficulties arise during conduction anesthesia, then the duration of unpleasant sensations is calculated in only a few seconds.
During the operation, conduction anesthesia guarantees a complete absence of pain with a clear consciousness of the patient. If the patient feels anxious and wants to sleep, then conduction anesthesia can be combined with sedation.
How does conduction anesthesia work?
Anesthesia during conduction anesthesia is achieved due to the blockade of a nerve or group of nerves through which the pain impulse is transmitted from the source of pain (the site of surgery) to the brain, which processes this signal and gives it to us directly in the form of a sensation of pain. Depending on which nerve is blocked, anesthesia for a particular area of the body will occur.
How is conduction anesthesia performed?
Technically, conduction anesthesia is one or more injections of a local anesthetic solution into the area where the nerve required for the block is located. For regional anesthesia to work, the drug must be injected in close proximity to the nerve—a few fractions of a millimeter from it. If the local anesthetic is injected a little further than the nerve, then anesthesia will not develop, and the patient will feel pain during the operation, which will require a change in anesthesia tactics, in particular, the use of a different type of anesthesia. In the event that a local anesthetic is injected directly into the nerve itself, an anesthesia complication such as neuropathy may develop (see below).
What operations can be performed under conduction anesthesia?
Unfortunately, due to the anatomical characteristics of the human body, not every part of the body can be anesthetized using conduction anesthesia. Therefore, an approximate list of the main operations that can be anesthetized using conduction anesthesia will be as follows: operations on the upper and lower extremities, operations to remove an inguinal or femoral hernia, some operations on the genital organs, operations on the thyroid gland, operations on the carotid arteries, dental operations.
What are the complications of conduction anesthesia?
The most serious complications of conduction anesthesia include the development of neuropathy, as well as the occurrence of an adverse reaction to the local anesthetic.
An adverse reaction to a local anesthetic is manifested either by the development of an allergic reaction or a systemic reaction of the body. A systemic reaction of the body occurs when a local anesthetic solution is accidentally unintentionally introduced into a blood vessel; it can manifest itself as cardiac arrhythmia, dizziness, weakness, and loss of consciousness. An allergic reaction to a local anesthetic is extremely rare, occurring in approximately 1 in 50,000 anesthetics.
Neuropathy is damage or dysfunction of a nerve, manifested by various symptoms: a crawling sensation, numbness, pain or muscle weakness in the anatomical area where anesthesia was performed. However, you should not be upset or afraid of conduction anesthesia. The incidence of neuropathy is not that high - less than 1% of cases. In addition, in most cases, complete restoration of the damaged nerve’s functionality occurs within a few months (less often within a year). And, most importantly, the development of new technologies for conduction anesthesia has made it possible to minimize the likelihood of developing this type of complication.
What makes conduction anesthesia as safe as possible?
Conduction anesthesia is made as safe and effective as possible by using ultrasound.
Ultrasound helps to perform conduction anesthesia under visual control, and not blindly, as it was before (and sometimes still occurs in the vastness of our homeland). The use of an ultrasound machine helps to see the nerve and needle, and, therefore, allows you to inject local anesthetic into the required area.
The use of ultrasound in conduction anesthesia can minimize the risk of developing neuropathy, accidental intravascular injection of a local anesthetic and, most importantly, significantly increase the success of performing a nerve block, thus obtaining one hundred percent high-quality anesthesia.
Complications of local anesthesia and endodontic treatment
Posted by Tara Renton
Translation: Gavryushina Anna
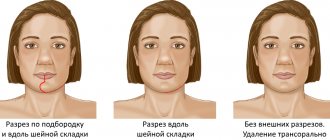
Possible mechanism of nerve damage during local anesthesia
Nerve injury due to local anesthesia is a complex problem. Nerve damage may be physical (needle, compression due to epineural or perineural hemorrhage) or chemical (bleeding or local anesthetic components). Thus, the resulting nerve injury may be a combination of peri-, epi-, and intraneural trauma causing subsequent hemorrhage, inflammation, and scarring leading to demyelination (loss of the nerve sheath). Administration of local anesthesia can cause nerve damage in a variety of ways. The location of the nerve injury may also be important, as well as the mechanism. Factors to consider are that only 1.3–8.6% of patients experience an "electric shock" type sensation when receiving mandibular anesthesia, and 57% of patients who suffer from long-term neuropathy did not experience discomfort during the injection , so this is not a specific sign.
Injuries during mandibular anesthesia
Neuropathy
Any damage to sensory nerve tissue can cause a combination of anesthesia (numbness), paresthesia (altered sensation that is not painful), dysesthesia (altered sensation that is unpleasant/painful), and neuropathic pain. Neuropathy in the orofacial region should be taken seriously and the cause should be determined as there are some serious conditions that need to be addressed if the cause is not obvious. It is often possible to determine its origin from the anamnesis. Lack of sensation must be noted on the face so that the increase or decrease in the insensitive area can be assessed. Any patient with an expanding area of paresthesia for which there is no known cause should be referred to a specialist. Among other things, paresthesia can result from trauma, nerve damage, surgery, infections and prolonged reactions to local anesthesia, viruses, malignancies, or serious illnesses. If a dental cause is suspected, patients require re-evaluation, careful documentation, and follow-up.
Unilateral paresthesia and facial paralysis can occur when conduction anesthesia is administered in the wrong direction when the local anesthetic solution is deposited in the parotid gland. This usually occurs when the depth of penetration of a long needle is approximately half its length. This most likely occurs when the mandibular ramus expands laterally, making it difficult for the operator to “feel the bone.” Unilateral facial paralysis is reversible. It goes away within a few hours. The patient should be reassured and his eyes protected until the blink reflex is restored, as the corneal reflex is often impaired.
Neurological damage from untreated periapical infections
In endodontic practice, we often encounter patients with apical periodontitis of endodontic origin, leading to impaired sensitivity of the inferior alveolar or mental nerve. It invariably resolves with a decrease in inflammation and local swelling. A number of authors have reviewed and documented clinical cases of a neurological disorder with paresthesia and hypoesthesia of the mental nerve arising as a consequence of apical periodontitis of the second premolar and second molar of the mandible.
Motor nerve palsy due to endodontic treatment
There are reports of shortages