From this article you will learn:
- what causes gingivitis,
- what are the forms of this disease,
- gingivitis in adults - symptoms and treatment at the dentist.
The article was written by a dentist with more than 19 years of experience.
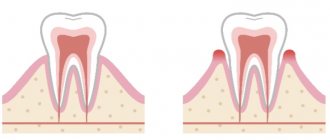
Gingivitis is an inflammation of the marginal part of the gum adjacent to the teeth, including the interdental papillae (Fig. 1-2). With this disease, patients most often complain of bleeding gums, pain when brushing teeth, as well as swelling, redness or cyanosis of the gums. Gingivitis with a predominance of such symptoms is usually called “catarrhal” by dentists.
However, in a small percentage of cases, inflammation can also manifest as gingival overgrowth, or even ulceration and necrosis. The most important feature that distinguishes gingivitis from other inflammatory gum diseases is that the inflammation does not spread deeper than the gum mucosa. Accordingly, with gingivitis there is no destruction of the bone tissue around the teeth, no mobility of the teeth, i.e. symptoms of a disease such as periodontitis.
Gingivitis: photo, diagram
If you have mobility of some teeth, as well as periodontal pockets, from which pus can be released during periods of exacerbation, such symptoms no longer indicate gingivitis, but the presence of periodontitis (a more severe form of gum inflammation). You can read more about this disease at the link above. Let us only note that in most cases the development of periodontitis is a consequence of untimely and/or ineffective treatment of gingivitis.
Main forms of gingivitis:
- catarrhal gingivitis (Fig. 1-8),
- ulcerative-necrotizing gingivitis (Fig. 12-15),
- hypertrophic gingivitis (Fig. 16-18).
In this article we will analyze in detail each form of gingivitis, indicating effective drugs and regimens for their use. We will also list patients’ mistakes in the process of self-medication, which often lead to the development of severe chronic gum inflammation. If you are more interested in how to properly treat gingivitis not in adults, but in children, then read more about this in the article: → Gingivitis - symptoms and treatment in children
Catarrhal gingivitis: symptoms
Among all patients with gingivitis, this form accounts for more than 97% of cases. Those. This is the most common form of this disease. The term “catarrhal” means that the inflammation affects only the mucous membrane of the gums, i.e. flows superficially. Thus, with gingivitis, there is no destruction of the bone tissue around the teeth, as well as destruction of the periodontal attachment. In Fig. 3-5 you can see what catarrhal gingivitis looks like in the oral cavity.
The cause is exceptionally insufficient oral hygiene, as a result of which soft microbial plaque accumulates in the area of the necks of teeth, and the formation of tartar occurs. Plaque bacteria produce toxins and pathogens, which trigger inflammation in the gum mucosa. At the same time, various chronic diseases or vitamin C deficiency are not the direct causes of the development of gingivitis, but may be a predisposing factor that increases the impact of microbial plaque.
Catarrhal gingivitis: photo
Symptoms –
- swelling of the gingival margin and interdental papillae,
- redness or bluishness of the gums,
- bleeding gums when brushing teeth,
- pain when brushing teeth,
- itching in the gums,
- Usually, accumulations of microbial plaque are visible at the necks of teeth.
The appearance of bleeding is associated with an increase in the permeability of capillary walls, capillary fragility, as well as a decrease in the thickness of the epithelium of the gum mucosa. All this arises as a result of the influence of toxins and microbial plaque pathogens on the mucous membrane of the gums. Most often, bleeding occurs when the gums are exposed to mechanical factors (for example, when brushing teeth or chewing rough, hard food).
Pain when brushing teeth is also associated with thinning of the epithelium of the gum mucosa. Thinning of the epithelium against the background of gum inflammation is a natural process, and develops due to an increase in the rate of desquamation of epithelial cells (24stoma.ru).
Forms of catarrhal gingivitis –
There are 2 variants of the course of the catarrhal form of gingivitis. Firstly, there is acute catarrhal gingivitis (Fig. 3-4), which is characterized by bright red gum color, acute development, and sometimes significant bleeding and pain when brushing teeth. With this form of the disease (due to pain when brushing teeth), patients sometimes abandon oral hygiene altogether, which leads to an even greater increase in the amount of microbial plaque, and as a result, to an increase in gum inflammation.
Secondly, the chronic form of the disease (Fig. 5-6), which is characterized by sluggish symptoms over a long period of time. Chronic catarrhal gingivitis symptoms of bleeding will be quite minor, and pain during brushing may be completely absent. The marginal gum and periodontal papillae will have a bluish color. However, exacerbation of symptoms may periodically occur, which usually occurs against the background of a decrease in immunity during the period of colds.
Chronic catarrhal gingivitis –
Symptoms of gingivitis in adults
To properly treat the pathology, you need to know that the symptoms of gingivitis and treatment are closely interrelated. What helps with the catarrhal form may not be sufficient with the necrotic form. What to do if you are in doubt about what kind of gingivitis you have? Photos from the collections will help in a rough assessment, and then you should go straight to the periodontist’s office.
Common signs of gingivitis:
- Bright red tint of gums (due to dilated capillaries)
- Swelling of the papillae (due to exudation processes)
- Unpleasant odor (halitosis)
- Bleeding (increased vascular permeability)
- Pain when eating (nerve endings are compressed due to swelling)
- Dense plaque and tartar
Important! Chronic gingivitis often occurs together with general pathology. Usually this is an ulcerative lesion of the gastrointestinal tract or HIV infection.
Treatment of gingivitis –
Treatment of catarrhal gingivitis will be quick and effective if 3 conditions are met. Firstly, treatment should primarily be aimed at removing microbial plaque and hard tartar (as the cause of inflammation). Secondly, anti-inflammatory therapy, which may include various rinses and special gels for gums. The third point is the normalization of oral hygiene.
A course of anti-inflammatory therapy can be carried out at home without any problems, but removing a layer of tightly attached microbial plaque and tartar from the surface of the teeth is impossible without visiting a dentist. The fact is that with the help of a regular toothbrush and paste, only “freshly formed” soft microbial plaque is effectively removed. But in the absence of regular hygiene, soft plaque quickly undergoes mineralization by calcium and phosphorus salts (contained in saliva), and turns into tartar.
Partial mineralization of soft microbial plaque occurs on average within 10-16 hours, i.e. it is during this time that soft plaque hardens and becomes tightly attached to the tooth. This is how hard dental deposits gradually form (Fig. 7-8), which can no longer be removed simply by brushing your teeth with a brush and paste. If you start using antiseptic and anti-inflammatory agents for the gums without removing the dental plaque that caused the inflammation of the gums, the effect of the treatment will be short-lived, and the inflammation itself will become chronic.
What does hard dental plaque look like?
Conclusions: please note that dental deposits can be not only clearly visible supragingival (as in Fig. 7-8), but also subgingival, which are located slightly below the gum level. Typically, such deposits can be suspected in the presence of swelling, cyanosis and bleeding of the gums (interdental papillae) - in the visible absence of microbial plaque or dental deposits in the area of the necks of the teeth. Once again, subgingival tartar can be identified and removed only by a dentist.
DETAILED TREATMENT SCHEME –
As we said above, treatment for gingivitis consists of professional teeth cleaning at the dentist, a course of anti-inflammatory therapy, and, no less important, teaching the patient about proper oral hygiene.
The author of the article has more than 10 years of experience as a periodontist, and therefore our recommendations really work (state-issued documents on advanced training in the Periodontology program can be viewed in the editorial section).
1) Removal of dental plaque –
There are several methods for removing dental plaque, but given that with gingivitis the gums are inflamed and usually bleed, it is best to use ultrasonic teeth cleaning (Fig. 9). A special attachment creates ultrasonic vibrations and breaks the attachment of dental plaque to the surface of the tooth enamel. Usually the procedure takes from 30 to 60 minutes (depending on the amount of dental plaque). The procedure is usually painless, but can be performed under anesthesia if desired. Below is a video of this procedure.
At the end of the visit, the dentist will first treat your gums with an antiseptic, and then apply an anti-inflammatory gel to it. A good dentist will then offer to teach you how to properly use a toothbrush and floss, and will also prescribe you a course of home anti-inflammatory therapy. Believe me, within the first 24 hours after removing deposits, you will notice a significant improvement.
Video of dental plaque removal with ultrasound –
2) Anti-inflammatory therapy –
If you have gingivitis, treatment at home will mean that you must conduct a course of antiseptic rinses + applications of a special medicinal gel to the gums. With ordinary catarrhal gingivitis, there is no need to carry out such a course at the dentist, because You can also rinse your mouth with an antiseptic and apply the gel to your gums yourself. The main thing for this is to choose the right products for your gums.
Treatment regimen – the standard course of treatment for gingivitis is usually 7-10 days. Gum treatment is carried out 2 times a day - morning and evening. In the morning after breakfast, first brush your teeth, and after oral hygiene, rinse your mouth with an antiseptic chlorhexidine solution. To do this, you need to take 10 ml of solution into your mouth (about 1 sip) and, without spitting anything, rinse your mouth for exactly 1 minute. Keep in mind that you should not rinse your mouth with water after rinsing. Below we will tell you what concentration of chlorhexidine is best to use.
The second stage of morning treatment is the application of a medicinal gel to the gums. During my time as a periodontist, I tried many different products, but Cholisal gel works best. Before applying this gel to the gum, it is first better to make a dry gauze swab from a bandage. The fact is that the mucous membrane of the gums is always wet, and therefore, in order for the gel to stick better, you need to dry the gums with a dry gauze pad before applying it. Next, in front of the mirror (with your teeth bared so that your gums are clearly visible), apply the gel to the marginal part of the gums around the teeth using a clean finger.
It is advisable to apply the gel to the gums around the necks of the teeth - not only in front of the dentition, but also from the side of the palate/tongue. You can rub the first portion of the gel into the marginal part of the gums (with light massaging movements), and apply the second portion without rubbing. This will increase efficiency, but such double treatment is best done only from the front surface of the teeth. On the side of the palate/tongue, you need to do one thing - either apply the gel to the gums and leave it, or just rub it in (the second would be more preferable).
Important: keep in mind that saliva is always released during the application of the gel, but it does not need to be accumulated or spat out. Swallow it as usual. After treating the gums with gel, it is advisable not to drink for 30-60 minutes, and also not to eat or rinse your mouth for 2-3 hours. The second treatment is carried out in the evening (the scheme is similar - after brushing your teeth, rinse your mouth with an antiseptic, and then apply the gel to the gums). And so on for 7-10 days.
Which means are better to choose?
If previously a 0.05% concentration of chlorhexidine was universally recommended for the treatment of gums, now it is recommended mainly only for children and adolescents. In adults, for the treatment of gingivitis, it is better to use chlorhexidine 0.12%, but if you have very severe bleeding and sore gums, in this case chlorhexidine 0.2% will be optimal.
Please note that a 0.05% concentration of chlorhexidine will be especially ineffective: if you smoke, if you eat a lot of carbohydrates, if you have concomitant chronic tonsillitis, if you have gastrointestinal diseases, if you have a history of candidiasis (thrush), if you have long-term chronic inflammation of the gums. In all these cases, it is also better to use 0.2% chlorhexidine for 7 days.
As for choosing specific brands of mouthwashes and gum gels, you can read more about this in the articles linked below. In this case, we should not forget about special anti-inflammatory toothpastes, which contain components that can reduce gum bleeding and inflammation.
→ The best mouth rinses for gingivitis → Choosing the optimal gel for gums → Rating of anti-inflammatory toothpastes
Gingivitis: photos before and after treatment
Important: note how the bluish gums turned pink after treatment of gingivitis in Fig. 10-11. The return of healthy gum color is primarily associated with the removal of dental plaque. Without this, even the most powerful anti-inflammatory drugs will not be able to completely normalize the condition of the gums - after all, the gums will continue to be affected by toxins and pathogens from microbial plaque and dental plaque.
3) Normalization of oral hygiene –
Please note that simply curing gingivitis is not enough. It will very soon arise again if you do not start brushing your teeth correctly and regularly. In the absence of regular oral hygiene, plaque and tartar will form again very quickly and cause new inflammation. Good hygiene includes not only the use of a toothbrush and toothpaste, but also special dental floss. In order not to clutter this article, we do not provide detailed hygiene recommendations here, but you can take them into account in our articles:
→ How to brush your teeth properly, → Technique for using dental floss.
It is also worth noting that during the period of treatment of gingivitis you may need a special soft toothbrush, as well as medicated paste. A soft toothbrush for gingivitis (labeled “Soft”, i.e. “soft”) is necessary only if brushing your teeth causes you pain and a desire to give up hygiene altogether. But dentists recommend using such a brush only for the period of treatment of gingivitis - no more than 2 weeks, because Soft bristles are less effective at removing microbial plaque.
Brushes with soft bristles (Lacalut, Parodontax) –
About tooth loss and how to avoid it
Last year, we, at Star Smile, released a cartoon video in which the heroine was thinking about what to do - either start bite treatment when she was young, or wait until all the teeth begin to decay. Here he is, by the way
The video received quite a lot of views and responses, many patients asked us to continue the topic of consequences - to show readers what inattention and carelessness when caring for teeth and gums can lead to. Therefore, we will continue to educate you and hope that our articles will help you contact doctors in a timely manner and avoid most of the problems that we write about.
Vincent's ulcerative-necrotizing gingivitis -
Vincent's ulcerative-necrotizing gingivitis is one of the most severe forms of gingivitis, and its development is accompanied by quite serious symptoms of intoxication of the body. Sometimes the terms “Vincent gingivostomatitis” or simply “ulcerative gingivitis” are also used to refer to it. There are acute and chronic forms of this disease (Fig. 12-15).
Causes of occurrence: critically poor oral hygiene plays a significant role in the development, when there is a significant increase in the mass of microbial plaque on the teeth (especially fusobacteria and spirochetes). Under these conditions, the local immunity of the oral mucosa is no longer able to cope with large amounts of toxins released by pathogenic bacteria. As a result, foci of mucosal necrosis and ulceration occur.
The triggering factor that initiates the development of necrotizing ulcerative gingivitis against the background of poor oral hygiene can be a sharp decrease in immunity or an exacerbation of severe concomitant chronic diseases of the body. But these factors are only predisposing; the main reason is poor hygiene and the accumulation of microbial plaque and/or tartar.
Acute ulcerative-necrotizing gingivitis: photo
Chronic ulcerative-necrotizing gingivitis: photo
Necrotizing ulcerative gingivitis: symptoms and treatment in adults, upon visual examination, you can find that the gums are covered with a whitish or yellowish coating, there are areas of gum ulceration, and some of the gingival papillae are necrotic. In the acute course of the disease, patients complain of high fever, loss of appetite, headaches, putrid breath, bleeding and pain in the gums (Fig. 12-13). In the chronic course of Vincent's gingivitis, the symptoms are less pronounced (Fig. 14-15).
How to cure ulcerative necrotizing gingivitis - treatment is carried out exclusively by a dentist, and urgently. The basis of treatment is the removal of dental plaque, including mandatory scraping of necrotic plaque. Plaque along with dental deposits can be easily removed using a conventional ultrasonic tip (scaler), followed by removal of plaque residues with a curettage spoon. Next, antibiotics, antiseptic rinses, and anti-inflammatory drugs are prescribed.
- Antibiotic therapy - prescribed antibiotics must be effective against fusobacteria and spirochetes, therefore a combination drug of amoxicillin and clavulanic acid, Amoxiclav, is usually prescribed in a tablet.
(for adults - tablets of 500 mg amoxicillin + 125 mg clavulanic acid, which are used 3 times a day - during the first day of the disease, and 2 times a day for the next 6 days). In parallel with Amoxiclav, you need to take the antibiotic Trichopolum (Metronidazole) - 500 mg 3 times a day, for a total of 7 days. In parallel with this, you should use antiseptic rinses with a 0.2-0.25% chlorhexidine solution, as well as a gum gel, for example, Cholisal.
Important: the use of antibiotics and antiseptics for self-medication (without removing deposits and necrotic plaque) will lead to the transition of acute necrotizing gingivitis to a chronic form. As a result, you will get gradual increasing necrosis of the gums, exposure of the roots of the teeth, as well as constant intoxication of the body. Therefore, an urgent visit to the dentist and removal of dental plaque is mandatory! After inflammation subsides, agents are prescribed that accelerate the epithelization of the mucous membrane, for example, Solcoseryl Gel.
Causes of ulcerative gingivitis
Ulcerative gingivitis is an inflammatory disease that affects the gums and leads to destructive changes in the gum tissue. Acute gingivitis can lead to tooth mobility, including tooth loss.
The appearance of ulcerative gingivitis can be due to various reasons:
- Poor oral hygiene, which leads to the accumulation of soft plaque;
- The presence of carious teeth and other foci of infection;
- Incorrectly installed dentures or braces;
- Regular injury to the gums due to decayed or incorrectly positioned teeth;
- Weakened immunity and the presence of chronic systemic diseases (disorders of the cardiovascular, endocrine, digestive systems, blood diseases);
- Chronic fatigue, lack of sleep, stress;
- HIV – infection, intoxication, radiation exposure;
- Recently suffered infectious diseases (flu, sore throat, stomatitis, herpes, etc.);
- Lack of vitamin C, poor nutrition;
- Excessive consumption of alcohol and nicotine.
Ulcerative gingivitis most often occurs in the presence of several negative factors and primarily indicates weak immunity and the presence of immunodeficiency. HIV disease is very often accompanied by ulcerative manifestations on the gums.
Hypertrophic gingivitis –
Hypertrophic gingivitis is a variant of chronic gum inflammation.
With it, there is an increase in the volume of the gums, which can occur either due to persistent chronic swelling of the gums (which practically does not respond to anti-inflammatory therapy), or due to its fibrous growth. The hypertrophic form of gingivitis most often occurs only on the front surface of the teeth. Causes of occurrence - most often occurs with endocrine disorders, toxicosis of pregnant women (gingivitis of pregnant women), with hormonal changes in adolescents (juvenile gingivitis), as well as with malocclusion and in the presence of local traumatic factors - overhanging edges of fillings and crowns. In some cases, gum hypertrophy is a consequence of long-term chronic catarrhal gingivitis.
Hypertrophic form of gingivitis: photo
Hypertrophic gingivitis - symptoms and treatment will depend on the form of this disease, i.e. depending on what exactly causes the gum enlargement (edema or fibrous growth). In accordance with this, edematous and fibrous forms of hypertrophic gingivitis are distinguished.
- Edema form (Fig. 16-17) - the gingival papillae in this form are enlarged not due to tissue proliferation, but due to their swelling.
Accordingly, they will not be dense, but loose. It is this form of gingivitis that most often develops in pregnant women and adolescents against the background of hormonal changes. At the beginning of treatment, it is necessary to remove dental plaque and anti-inflammatory therapy. If the effect of these measures is insignificant, then sclerosing therapy is used, when, against the background of pain relief, a sclerosing solution is injected into the swollen gingival papillae. Typically, solutions of 40% glucose, 25% magnesium sulfate, 10% calcium chloride are used. 0.1-0.2 ml of solution is injected into each papilla. Course – 3 or 4 injections into each gingival papilla. The intervals between series of injections are usually 1-2 days. If the effect of such therapy is absent or insufficient, prednisolone is injected into the gingival papillae.
- Fibrous form (Fig. 18, 19) - the gingival papillae in this form are dense, and not loose as in the edematous form. This is due to the fact that the increase in gum volume did not occur due to swelling, but due to the proliferation of fibrous connective tissue. Treatment begins with the elimination of traumatic factors (overhanging edges of fillings, crowns, and also in the case of a traumatic bite - selective grinding of teeth). At the same time, dental plaque is removed.
The main method of treating the fibrous form is surgical excision of gum tissue (Fig. 19-21). After excision, a course of anti-inflammatory therapy is prescribed, for example, therapeutic dressings with heparin ointment, hydrocortisone and other drugs. It should be noted that in the absence of treatment, the long-lasting edematous form of hypertrophic gingivitis can easily turn into fibrous.Surgical excision of the gum –
Gingivitis: my gums hurt
The process, which is characterized by gum inflammation, swelling, redness and bleeding, is called gingivitis and is one of the most common periodontal diseases in both children and adults. Only 3% of people can boast of absolutely healthy gums. How to get into such a small percentage of lucky ones? The answer is simple - follow the necessary measures to prevent gum inflammation, regularly visit the doctor and not let even seemingly harmless signs of an incipient disease take their course.
Gingivitis is the last of all diseases in periodontology in which the inflammatory process can still be stopped. Next comes periodontitis, a disease in which inflammation spreads to other periodontal tissues. From this point on, treatment is based only on bringing the disease into remission and attempts to relieve symptoms as much as possible at the time of relapses, as well as in the future when it is necessary to resort to tooth extraction. Therefore, gingivitis in children and adults requires increased attention in order to avoid serious periodontal problems.
Gingivitis: treatment at home
Once again, let us draw your attention to a very important point - treatment of gingivitis in adults at home is only possible in terms of a course of anti-inflammatory therapy. At home, you can successfully use antiseptic rinses and applications to treat catarrhal gingivitis, but to remove plaque, you still need to visit the dentist!
A small example: a person’s gums are bleeding and he decides to use the remedies he heard about in an advertisement. These can be various gels, rinses or anti-inflammatory toothpastes. And indeed, as long as a person uses such means, bleeding decreases or disappears completely for a while. But as soon as the use of the products is stopped, the gums begin to bleed again, plus their swelling and redness return.
The reason for this is quite commonplace - the person tried to treat the symptoms (such as bleeding, pain, swelling) without removing the cause of these symptoms (microbial plaque, as well as hard supra- and subgingival dental plaque). Advertisements for various dental products do not talk about the causes of bleeding or the need to remove dental plaque. Moreover, for obvious reasons... We hope that our article on the topic: Gingivitis symptoms and treatment in adults was useful to you!
Sources:
1. Dental education of the author of the article, 2. Based on personal experience as a periodontist, 3. National Library of Medicine (USA), 4. American Academy of Periodontology (USA), 5. “Non-surgical periodontal treatment” (Roncati M.).
Causes
External or internal factors can stimulate the inflammatory process in tissues, including:
- injuries to mucous membranes and teeth;
- cervical caries;
- anomalies of the dentition and soft tissues of the oral cavity;
- inadequate hygiene;
- sharp edges of the filling, incorrectly fixed braces or dentures.
The causes of catarrhal gingivitis can be supported by additional factors - problems with the thyroid gland, viral infections, blood pathologies and other disorders that increase the risk of developing inflammation several times.
Diagnostic tests
- Schiller-Pisarev test
This test is based on determining the level of glycogen in the gum. Its amount increases significantly during inflammation, while healthy gums do not contain glycogen. Lubricating the inflamed gums with Schiller-Pisarev solution gives a color change reaction from light brown to brown. This research method is used to make diagnoses of both periodontitis and gingivitis.
- Assessment of oral hygiene level
A solution (2 g of potassium iodide, 1 g of crystalline iodine, 40 ml of distilled water) is applied to the outer surface of the six lower front teeth.
The assessment is carried out using a five-point system and each tooth is assessed separately:
- 5 points – complete staining of the entire tooth surface;
- 4 points – staining of ¾ of the tooth surface;
- 3 points – staining of half the tooth surface;
- 2 points - staining of a quarter of the tooth surface;
- 1 point - absence of any staining of the tooth surface.
Then the scores of all examined teeth are summed up and divided by their number (usually the test is carried out on six teeth). This is how the hygiene index is obtained.
As a result, the quality of hygiene is assessed:
- 1.1-1.5 points – good hygiene index;
- 1.6—2.0—satisfactory hygiene index;
- 2.1—2.5—unsatisfactory hygiene index;
- 2.6—3.4—poor hygiene index;
- 3.5-5.0 - very poor hygiene index.
- Vacuum test according to Kulazhenko
Using a Kulazhenko vacuum apparatus, it is possible to determine the time of hematoma formation when a vacuum is applied to the gum area. Typically, the test is carried out in the incisor area by placing a tube of the device on the gum. The formation of a hematoma in 60 seconds indicates the normal condition of the gums, while the appearance of a hematoma in 29-30 seconds signals an inflammatory process.
- Oxygen tension in gum tissue
The sensor of the device is applied to the gum, and the device records the level of tissue hypoxia. Reduced oxygen tension indicates a prolonged inflammatory process.
Why is inflammation of the gums near the teeth dangerous?
Childhood gingivitis develops very quickly, since there are many prerequisites for this - from child abuse of sweets to insufficient oral hygiene. After the start of the process, the volume of actively multiplying pathogenic microflora quickly increases. On the second or third day, you can already notice the first signs of beginning mucosal erosion. If you do not seek help at this time and start the disease, the already matured child will suffer from gum problems all his life and may lose his teeth prematurely.