Gingivitis: causes and symptoms
In order to know how to treat gingivitis, it is necessary to study at least brief information about this disease and the mechanisms of its occurrence. Gingivitis is a fairly common dental disease, which is an inflammation of the gums, which can be treated with dental ointments and rinses. These rules are similar for the prevention of stomatitis.
The occurrence of gingivitis is often associated with improper oral care, which results in the formation of plaque consisting of bacteria. This sticky substance accumulates along the edges of the gums and in places that are difficult to reach with a regular toothbrush.
In most cases, the causative agents of gingivitis are pathogenic microorganisms that live in the oral cavity of healthy people. The immune system does not allow bacteria to manifest itself, but when it weakens, the virus begins to progress in the body. Among the reasons that can trigger the development of the disease are the following:
- Neglect of dental treatment;
- Poor quality prosthetics and installation of braces;
- Diabetes;
- Viral diseases of the upper respiratory tract;
- Hormonal imbalance, for example, during pregnancy;
- Unbalanced diet, especially lack of vitamins C;
- Nicotine abuse.
Many experts do not consider gingivitis to be an independent disease. In their opinion, the disease develops against the background of other pathologies that contribute to a decrease in the body’s immune defense.
Symptoms of simple gingivitis include swelling and redness of the gums, which may bleed when eating or brushing teeth, and gums often pull away from the teeth. The general clinical picture of the disease looks like this:
- Increased sensitivity of teeth and gums;
- The appearance of dental plaque and tartar;
- Bad breath;
- Swelling;
- Pain and burning when biting;
- Soft tissue necrosis.
There may be no pain, but with acute gingivitis there is already severe pain. In addition, if gingivitis is not treated promptly, complications may develop and numerous ulcers may appear.
Diet and nutrition
For inflamed gums, it is necessary to include a large amount of fresh fruits and vegetables in your diet:
- Citrus fruits . A higher vitamin C content helps reduce inflammation and bleeding.
- Apples and pears . The presence of pectin and a large number of microelements help accelerate the healing process.
- Blackcurrant, raspberry, blackberry . They contain a large number of minerals and vitamins that increase the body's ability to fight inflammation.
- Cabbage, zucchini, carrots . Contains fiber and vitamins from the antioxidant group. They enhance metabolic processes in the body and accelerate tissue regeneration.
Since a common cause of gum inflammation is a lack of vitamins A, C, E and B in the diet, in some chronic cases taking multivitamin complexes (CENTRUM, VITRUM, THERAVIT, Supradin, Sana-Sol) is indicated.
Remember! Gingivitis is a serious chronic oral disease and can even cause dangerous complications. Therefore, it is impossible to treat this disease without the participation of a dentist. Only an experienced doctor will be able to assess the condition of the gums and recommend optimal treatment methods!
Types of diseases
There are several types of gingivitis, so for effective treatment it is necessary to determine the form of the disease. The following options are possible here:
- Catarrhal. One of the most common forms, which is diagnosed in most patients. The disease manifests itself as bleeding gums and discomfort when pressing on soft tissues.
- Hypertrophic. Usually diagnosed during adolescence. The source of inflammation is located in the area of the front teeth. A characteristic feature of this form of the disease is the proliferation of interdental papillae, and soft tissue hyperplasia is possible.
- Ulcerative-necrotic. This is an advanced stage, which is manifested by acute pain, ulcers in the mouth, and excessive salivation. Patients experience lack of appetite, high fever, and enlarged lymph nodes.
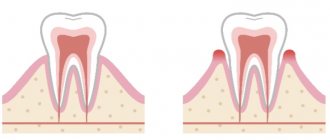
- Atrophic. The most severe form, in which atrophy of soft tissues is observed, the roots of the teeth are exposed. Characteristic signs of this disease are a gray tint of the mucous membrane and bad breath. The patient experiences general weakness and severe pain.
According to the form of its occurrence, gingivitis is divided into chronic and acute. In the first case, the disease does not have pronounced symptoms, there is practically no pain, the gums bleed only when brushing the teeth. In the second, the disease manifests itself more acutely and gives the patient a lot of discomfort.
Why is it important to see a doctor?
When the first signs of gingivitis appear, you should immediately contact a qualified dentist or periodontist. This is necessary in order to confirm the diagnosis. In terms of external signs, gingivitis resembles periodontal disease or periodontitis, however, there are significant differences between these ailments.
Treatment of gingivitis is carried out according to a single scheme, regardless of the cause of the disease. Treatment usually takes place in two stages: oral hygiene (performed by a dentist) and local rinsing with antiseptic solutions.
In particular, gingivitis affects only the gums, without affecting the bone tissue. With periodontal disease, the picture is the opposite: the teeth begin to loosen, while practically no inflammation is observed in the gums. However, only an experienced doctor can determine this difference. After confirmation of the diagnosis, a treatment regimen is prescribed.
Important! The doctor must be truly experienced. In case of periodontal disease, potentially dangerous teeth are removed. With proper treatment of gingivitis, teeth are usually preserved.
Diagnostics
Diagnosis of gingivitis is carried out in several ways, which are used in combination. At the initial stage, the doctor collects anamnesis:
- The diet and bad habits are revealed;
- The reasons for tooth extraction/loss are clarified;
- Genetic predisposition is determined.
After this, an examination of the oral cavity is carried out, the depth of the dental canals is studied with a special probe. Additional methods of diagnostic testing include x-rays and testing the sensitivity of the pulp.
The following methods can be used to diagnose gingivitis:
- Fedorov-Volodkina index;
- RMA index;
- Schiller-Pisarev test.
Treatment of gingivitis at home
Treatment of gingivitis at home is possible, but only if certain rules are followed. This is a serious disease that you cannot fight on your own. Even those drugs that have helped your friends may, at best, be ineffective, and at worst, cause complications. Therefore, treatment must be prescribed by a doctor. Even folk remedies should be used only with the permission of the dentist. Let's look at the most effective methods for treating gingivitis in adults at home.
Gels, ointments and compresses
Therapeutic ointments have antimicrobial and anti-inflammatory effects. They quickly relieve pain, eliminate bleeding, and reduce swelling. To treat gingivitis at home, dentists usually prescribe ointments and gels:
- Metrogil Denta. An antimicrobial agent containing an antiseptic and antibiotics. Thanks to its gel-like texture, the drug is convenient for self-use and has no contraindications. Not recommended for use in children under 6 years of age or during the first trimester of pregnancy.
- Asepta. A fast-acting drug that relieves pain and eliminates bleeding gums. It is not an independent means of treatment, therefore it is used only in combination with other medical procedures. There are no identified contraindications, but individual intolerance to individual components is possible.
- Solcoseryl. Homogeneous gel intended for external use. It has a wound-healing effect, stimulates the regeneration of soft tissues and mucous membranes.
- Holisal. Pronounced antimicrobial effect with analgesic effect. It has no age restrictions for use and is included in complex therapy in the treatment of gingivitis and other diseases of the oral cavity.
- Apident. Made from beekeeping products, it fights bleeding gums, soothes the mucous membranes, and destroys pathogenic microflora.
Rinse
Mouth rinsing is more related to the prevention of gingivitis, but in order to eliminate this disease as quickly as possible, doctors often include such therapy in the treatment complex. The most effective rinses include:
- Chlorhexidine;
- Furacilin;
- Furamistin;
- Miramistin;
- Rotokan;
- Chlorophyllipt.
Rinsing is done after each meal or throughout the day, at regular intervals. Depending on the concentration of the active substance, solutions can be used in pure form or need to be diluted with water. Information about this is indicated in the instructions for use.
Irrigators with rinsing for gingivitis
Irrigators are ideal for gingivitis, when the gums are inflamed, bleed and react painfully to any touch. The device directs a stream of water under pressure, which allows you to efficiently clean even hard-to-reach areas of the oral cavity. The jet pressure can be adjusted, which reduces pain to a minimum, and instead of water, medicinal solutions can be used. The following liquids are suitable to combat gingivitis:
- PerioGard;
- Donfeel;
- Peridex.
The listed drugs contain medicinal components that stop inflammatory processes in the gums and destroy pathogenic bacteria. The advantage of the irrigator is its gentle effect on infected surfaces: unlike toothbrushes, such devices do not injure the gums.
Vitamins
An additional effect that helps the body resist the disease. For gingivitis, vitamins of groups C, P and PP are usually prescribed. They are contained in ascorbic acid, Quercetin and Ascorutin.
Medicines
Medicines are usually prescribed in complicated or advanced cases of oral lesions. These are antibiotics or antimicrobial agents that should be taken only on the recommendation of a dentist.
Help to cope with gingivitis:
- Maraslavin;
- Novoimanin;
- Salvin.
Decoctions (folk remedies)
When figuring out how to treat gingivitis at home, you cannot skip traditional medicine. These are decoctions based on medicinal herbs and plants that help against inflammation and increase healing.
Medicinal decoctions against gingivitis:
- Sage;
- Calendula;
- Chamomile;
- Oak bark.
Even before using these products, it is better to consult with your doctor. Some herbal components are not compatible with medications, which can lead to undesirable consequences.
Healing gels and ointments
Gels and ointments used for gingivitis have an anti-inflammatory, healing and trophic effect. In addition, they relieve pain and eliminate bleeding.
Holisal
Cholisal has both analgesic, anti-inflammatory and antiseptic effects. The gel should be applied to the inflamed areas in a thin, even layer three times a day until any clinical manifestations of the disease disappear.
Solcoseryl
Gel with a pronounced wound-healing effect. The drug increases blood circulation in damaged tissues, improves metabolism and oxygen utilization. To eliminate inflammation, the drug is applied to the gums on both sides twice a day after regular daily brushing of teeth. The course of treatment is at least 10 days.
Asepta gel
Asepta gel, which contains propolis, is the strongest natural remedy against chronic inflammation and for wound healing. The drug also has an antipruritic and analgesic effect. For therapeutic purposes, the gel is applied to the affected areas in the morning and evening. The course of treatment is 14-21 days.
Apident-active
Multicomponent ointment for gums containing bee venom, propolis and herbal extracts. Quickly eliminates the symptoms of gingivitis, relieves pain and inflammation. Apply the drug with massage movements twice a day. Apident-active should be used after eating any food and brushing your teeth. The duration of the course of therapy is 14 days.
Features of gingivitis in children, adults and pregnant women
In general terms, gingivitis occurs in the same way for everyone, only the treatment methods differ. Adults are prescribed drug therapy, including antibiotics. The course lasts 10 days, medications are taken orally or administered intramuscularly.
Children are given antibacterial therapy and immunomodulating drugs are prescribed. In addition, the mucous membranes of the oral cavity are treated with decoctions of medicinal herbs and special gels.
Pregnant women are prescribed vitamins and safe antiseptic drugs. Antibiotics are completely excluded, but removal of tartar and plaque is mandatory.
Hypertrophic gingivitis –
Hypertrophic gingivitis is a variant of chronic gum inflammation.
With it, there is an increase in the volume of the gums, which can occur either due to persistent chronic swelling of the gums (which practically does not respond to anti-inflammatory therapy), or due to its fibrous growth. The hypertrophic form of gingivitis most often occurs only on the front surface of the teeth. Causes of occurrence - most often occurs with endocrine disorders, toxicosis of pregnant women (gingivitis of pregnant women), with hormonal changes in adolescents (juvenile gingivitis), as well as with malocclusion and in the presence of local traumatic factors - overhanging edges of fillings and crowns. In some cases, gum hypertrophy is a consequence of long-term chronic catarrhal gingivitis.
Hypertrophic form of gingivitis: photo
Hypertrophic gingivitis - symptoms and treatment will depend on the form of this disease, i.e. depending on what exactly causes the gum enlargement (edema or fibrous growth). In accordance with this, edematous and fibrous forms of hypertrophic gingivitis are distinguished.
- Edema form (Fig. 16-17) - the gingival papillae in this form are enlarged not due to tissue proliferation, but due to their swelling.
Accordingly, they will not be dense, but loose. It is this form of gingivitis that most often develops in pregnant women and adolescents against the background of hormonal changes. At the beginning of treatment, it is necessary to remove dental plaque and anti-inflammatory therapy. If the effect of these measures is insignificant, then sclerosing therapy is used, when, against the background of pain relief, a sclerosing solution is injected into the swollen gingival papillae. Typically, solutions of 40% glucose, 25% magnesium sulfate, 10% calcium chloride are used. 0.1-0.2 ml of solution is injected into each papilla. Course – 3 or 4 injections into each gingival papilla. The intervals between series of injections are usually 1-2 days. If the effect of such therapy is absent or insufficient, prednisolone is injected into the gingival papillae.
- Fibrous form (Fig. 18, 19) - the gingival papillae in this form are dense, and not loose as in the edematous form. This is due to the fact that the increase in gum volume did not occur due to swelling, but due to the proliferation of fibrous connective tissue. Treatment begins with the elimination of traumatic factors (overhanging edges of fillings, crowns, and also in the case of a traumatic bite - selective grinding of teeth). At the same time, dental plaque is removed.
The main method of treating the fibrous form is surgical excision of gum tissue (Fig. 19-21). After excision, a course of anti-inflammatory therapy is prescribed, for example, therapeutic dressings with heparin ointment, hydrocortisone and other drugs. It should be noted that in the absence of treatment, the long-lasting edematous form of hypertrophic gingivitis can easily turn into fibrous.Surgical excision of the gum –