Indications for implant removal
- Rejection of the structure mainly develops within six months after implantation.
- Peri-implantitis or perimucositis - the first is accompanied by a loss of jaw bone against the background of inflammation of the soft tissues, the second occurs without loss of tissue volume.
- Excessive load on the implant - occurs due to violation of the installation protocol.
- Incorrect position or defective implant is extremely rare.
- End of service life - for models with limited serviceability.
In our clinic, implant installation is carried out strictly in accordance with surgical protocols, using the most reliable systems in the world, Nobel Biocare (USA), with a lifetime warranty from the manufacturer and almost zero risk of rejection. If an unpleasant situation does arise, we guarantee free dismantling of the structure.
Prevention of negative consequences
The specialist must:
- prepare the oral cavity for surgery;
- diagnose diseases included in the list of contraindications;
- perform plastic surgery of the jawbone, if required;
- follow the surgical protocol for the procedure;
- ensure complete sterility;
- issue recommendations for the rehabilitation period.
The patient must:
- inform the doctor about existing serious illnesses;
- undergo the necessary examination;
- carry out assignments;
- ensure quality oral hygiene.
How are dental implants removed?
After the doctor, based on X-ray data, decides to remove the dental implant, a planned operation is scheduled. Removal of dental implants occurs in this way:
- Anesthesia is performed.
- The temporary or permanent crown is removed.
- The gum is incised to provide access to the artificial root.
- The implant is removed.
- Sutures are placed (if re-implantation is planned, bone material is added before suturing).
Clinical cases
Let us give examples from life regarding the unsuccessful completion of osseointegration, which resulted in the removal of the implant.
- After chemotherapy, a man had a titanium structure installed on the area of his jaw that had a malignant formation. The patient did not inform the doctor about the presence of a serious pathology, and the doctor did not notice bone changes in the operated area. Naturally, engraftment did not take place due to a decrease in the regenerative function of the bone. After the removal of the rod, six months passed before reimplantation became possible. During this time, the implantologist and oncologist actively took measures to solve the problem.
- The patient was treated by an orthodontist. She was fitted with braces and offered to have one tooth implanted. Since there was not enough space for it, bone augmentation was performed. After integration of the artificial root, it was rejected due to compression by neighboring teeth, as a result of which it was removed.
Dental implant removal cost
The cost of removing a titanium rod is equivalent to removing a complex tooth. However, a number of factors are taken into account that can increase the final amount. This is bone grafting, plastic surgery of soft gum tissue. Additional procedures are paid separately.
If the implantation was carried out in a clinic and the removal is performed in the same clinic, the procedure is free under warranty . If the patient came from another clinic, he needs to pay for the service. The price will depend on the clinical picture.
What the patient should know
Every person who is going to undergo a dental implant procedure must have the following information:
- implantation is a commercial service and is not included in the list of “Compulsory health insurance”;
- a denture that is broken for no reason by the patient can be replaced free of charge with a new one only in the clinic where it was placed;
- the cost of treating complications is much higher than the cost of implantation , so it is necessary to strictly adhere to the specialist’s prescriptions.
An important point is the selection of the clinic. Well-established dental centers provide a long-term guarantee on their work and are responsible for its quality.
Why does the implant not take root?
Physiological rejection
Occurs as a result of the patient’s body’s rejection of implants for the following reasons:
- allergic reaction to components of the dental system material;
- weakened immune system;
- chronic diseases in the acute stage;
- trauma to the jaw bone at the site of rod insertion;
- installation of an implant without taking into account the individual characteristics of the patient’s dental apparatus.
Doctor's mistakes
In clinics that value their reputation, such situations rarely happen:
- unsatisfactory diagnosis and sanitation of the oral cavity at the preparatory stage for implantation;
- neglect of the osteoplasty procedure for bone tissue atrophy;
- incorrect selection of the implant model, location in the jaw, unreliable fixation;
- violation of sterility;
- premature load on the structure, unacceptable in a particular situation;
- use of rods of questionable quality.
Patient errors
We make sure to give recommendations to the patient after implantation. If he was irresponsible in their implementation, the implant may be rejected due to:
- getting infections into the mouth through unwashed hands;
- non-compliance with the rules of daily oral hygiene;
- failure to follow postoperative recommendations for taking antibiotics and other drugs;
- smoking, drinking alcohol immediately after implantation of a titanium rod;
- increased physical activity;
- thermal procedures (bath, sauna, hot bath, overheating under the sun);
- hypothermia;
- neglect of doctor visits for examinations and preventive office procedures.
Patient errors that could potentially lead to implant failure
- palpation of the implant and its insertion site with dirty hands, resulting in infection entering the wound;
- neglect of the rules of regular dental hygiene after installation of an artificial root - the oral cavity is neglected, pathogenic bacteria develop in it;
- the patient violated the antibiotic regimen or neglected to take these drugs altogether;
- smoking and drinking alcohol immediately after implantation surgery;
- increased physical loads;
- overheating under the sun, in a bathhouse, sauna, warm bath;
- the person spent a lot of time in the cold;
- neglect of regular visits to the doctor for preventive teeth cleaning to remove soft and hard plaque.
Rejection symptoms
- Bleeding, redness of the gums;
- swelling;
- pain;
- increased body temperature;
- mobility of the artificial root;
- detachment of soft gum tissue by more than 1 mm;
- headache;
- difficulty chewing food;
- bad breath;
- weakness;
- the appearance of fistula tracts in the subgingival part;
- violation of the symmetry of the oval of the face.
Bleeding, swelling of the gums, pain and fever are normal in the first week after implantation. If they persist and other unpleasant signs are added, you should urgently consult the doctor who performed the operation.
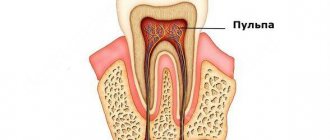
Peri-implantitis
Peri-implantitis is one of the most common reasons that an implant does not take root. When this complication develops, the soft tissue around the implanted implant becomes inflamed. Gradually, the inflammatory process is transferred to the bone and begins to destroy it. The titanium rod begins to loosen, and the periodontal pocket deepens. Then the purulent process develops. In most cases, peri-implantitis develops immediately after surgery, sometimes inflammation occurs several weeks or months later.
Symptoms of peri-implantitis are:
- Redness of the gums around the implant, severe swelling.
- Pain that intensifies when you press on the gums.
- Bleeding at the surgical site.
- The appearance of fistulas on the gums, from which purulent contents are released.
- Loosening of the implant.
You should consult a doctor at the first symptoms of peri-implantitis. At an early stage of development, inflammation can be treated and the implant can be preserved. Delaying a visit to the implantologist in most cases leads to the fact that the implant will have to be removed.
Dentistry for those who love to smile
+7
Make an appointment
How to avoid complications
It is possible to prevent the removal of a dental implant. Negative consequences are minimized when:
- a responsible approach to the issue of choosing a clinic - it is important to find out about certification for the right to conduct such operations, the qualifications of doctors, and familiarize yourself with the terms of the contract;
- maintaining sterility and hygiene during the rehabilitation period after implantation;
- quitting smoking and alcohol in the first 7-10 days;
- minimizing physical activity;
- excluding solid foods and hot foods from the diet;
- refusal of thermal procedures;
- Regular visits to the clinic in accordance with the drawn up treatment plan.
Implantation is a serious surgical procedure, and during the recovery phase it is important to follow recommendations regarding nutrition, hygiene, and medication.
The body's reserves are not endless
Each organism has different reserves and the cause of the negative process may be
:
- Exacerbation of chronic diseases plus weakened immunity. The regeneration algorithm does not start properly.
- Allergic reaction.
- Trauma to tissue in the area where there is an implant instead of an extracted tooth.
Perhaps the implant was installed a long time ago, of an old generation, and its service life has come to an end. Either the operation was performed in another specialized office by an inexperienced doctor, or the problem was inflammatory processes in the socket of the extracted tooth before the implant. Come, and the doctors of the German Implantology Center will help Moscow patients and everyone who turns to us for help to overcome unpleasant consequences.
Features of the operation
Removing an implant is carried out in almost the same way as removing your own tooth. Local anesthesia is used for the operation. First, the crown is removed, then the dentist loosens the titanium root so that it can be removed from the bone. After this, the oral cavity is disinfected. After extraction, the process of complete healing of the soft tissues takes up to two months. After this time, re-installation of the implant is permissible.
Diagnostics
The fact of rejection is established based on the patient’s complaints and dental examination data. To confirm the diagnosis and determine the cause, additional studies are prescribed: CT scan, orthopantomography. From the images you can assess the condition of the bone tissue and the position of the artificial root. Bone resorption and areas of osteoporosis indicate that the prosthesis has not taken root.
To determine the condition of the mucous membranes, special tests are used. Special compounds are applied to soft tissues. When the gums are inflamed, the tissue turns brown; in this case, the Schiller Pisarev test is positive. There are tests to evaluate how well a patient cares for their oral cavity.
To determine the type of pathogen that caused the inflammation, biomaterial is collected from the periodontal pocket. The culture method is used to determine which microflora caused the disease. This allows you to identify the source of infection and prescribe effective therapy.
Signs
Rejection can occur immediately after installation, several months, a year or several years after prosthetics. How do you know if there is a problem with an artificial root and when to see a doctor? If you decide to have a tooth implanted, ask your doctor to tell you about the warning signs that you need to pay attention to.
Early rejection
Soreness, swelling of soft tissues, and slight bleeding are normal after installation of a titanium structure. These symptoms are expressed 2-3 days after the procedure, then gradually disappear. Sharp pain that is difficult to relieve with analgesics is the first sign of a problem. It is accompanied by pronounced swelling of the gums, and bleeding develops. This course of the postoperative period indicates inflammation caused by infection or the body’s individual reaction to a foreign body. In this case, contact your dentist immediately.
Late rejection
Trouble often occurs in the first months after prosthetics. Implants that have been in place for more than a year rarely cause problems. The first sign of trouble is pain in the area of the artificial tooth. It can be mild, appear when pressure is applied, or be permanent. The soft tissues in the area of the prosthesis swell and bleeding occurs. If you visit the dentist at the first signs of pathology, you can stop the initial signs of inflammation and prevent complications. If you hesitate to visit the clinic, the inflammation progresses and spreads to the bone tissue of the jaw. The artificial root begins to wobble and falls out over time. Late rejection is typical for patients who do not follow doctor’s recommendations and who are inattentive to their health.
Can implantation be repeated?
After the first failure, many patients refuse this method of prosthetics, but there are those who want to repeat the procedure. Is it possible? Is there a chance for successful osseointegration?
To make a decision about the possibility of reimplantation, it is necessary to establish the reason why the first attempt failed. If rejection occurred due to a doctor’s error or incorrect choice of a titanium structure, you can try again after 6-7 months. To do this, you need to achieve complete restoration of the bone and sanitize foci of infection in the oral cavity. The chances of success with a repeat procedure are high.
If the dentist determines that the structure has not taken root due to a previously undiagnosed chronic disease or the body’s reaction to a foreign body, you need to choose another method of restoring the integrity of the dentition. Repeated attempts will not lead to results.
If the cause of the problem is poor oral care or smoking, the patient must change his lifestyle for successful dentures. Giving up a bad habit, regular, thorough cleaning of the oral cavity from food debris and plaque make it possible to repeat the procedure and obtain good osseointegration. If you do not want to change your habits, you will have to refuse implantation.
Listen to the doctor's recommendations. If he does not recommend reimplantation, there is no need to waste money and time; choose a prosthetic method that is more suitable for your case.
Reviews
I have been visiting this dentistry very often lately. I had implants and crowns installed by dental surgeon Dmitry Nikolaevich Amiridi. I especially liked his professionalism! The doctor is punctual, quickly provides services, provides detailed consultations and gives practical advice. All essentially, without excess water. He is attentive and treats his patients well. Overall, the clinic is clean and tidy, making it comfortable to be in. The service at the reception is also excellent!
Tatiana
Service: Implantation
I thank Dmitry Nikolaevich Amiridi and his team of professionals! Everything in your clinic is at the highest level!
Stanislav
Service: Implantation
Good afternoon. I have been a client of the Axioma Dental dental clinic for more than three years. I would like to note the professionalism of the doctors, the comfortable atmosphere (the clinic has been newly renovated), and the convenient recording and reminder system. All necessary information about treatment and further prevention is always provided. Thank you
Novel
Service: Implantation
Doctors of this specialty
Amiridi Dmitry Nikolaevich
Dental surgeon, implantologist, chief physician
Make an appointment
Karyatov Vitaly Vladimirovich
Dental surgeon, implantologist
Make an appointment
Prices for services
Implantation Straumann Roxolid SLActive RUB 52,000.
Implantation Straumann Roxolid 44,000 rub. Consultation with a specialist 500 rub. Extended consultation of several specialists with the development of a comprehensive treatment plan RUB 1,500. Closed sinus lift 18,000 rub. Open Sinus – lifting 47,000 rub. Guided bone regeneration (restoration of the height and width of the alveolar ridge) (for a segment of up to 4 teeth) RUB 40,000. Bone grafting using an autologous bone block RUB 56,000. Implantation Nobel (Replace CC/Parallel CC) RUR 44,000. Implantation Osstem (Korea) 29,000 rub. Implantation whiteSky (Bredent) 85,000 rub. Expert doctor:
Amiridi Dmitry Nikolaevich
Dental surgeon, implantologist, chief physician
Aspects of Dental Implant Removal
When dental implants are fractured, further removal from the jaw bone structure is required.
An implant fracture provokes destabilization of the abutment and loosening of the supporting screw, which, in turn, can lead to the development of inflammation and infection of the peri-implant area with various types of bacteria. The latter provokes bone loss in the coronal part of the intraosseous support. If an implant is fractured in the area of a cemented crown, there may be a simultaneous increase in the mobility of the abutment and the fixed restoration (photo 1). Implant fracture can also occur as a result of repeated fittings of inadequately fitted restorations and the tightening and unscrewing of the abutment screw (Figure 2).
Photo 1. Fracture of the implant platform. Due to inflammation, bone loss occurs. Granulations are noted in the apical part.
Photo 2. Example of an implant fracture. The structure requires removal, and the implantation area requires augmentation for the subsequent implantation procedure.
Even after cleaning the peri-implant area in such cases, as well as after taking systemic antibiotics, the patient continues to experience bone loss, swelling and discomfort in the peri-implant area. Removing implants with a fracture of the coronal part of the connection area is quite a difficult task when using only instruments with the possibility of developing reverse torque. Sometimes such an approach can also provoke further development of the fracture, which only complicates the possibility of removing the defective structure. Typically, such structures are removed using a hollow trephine. In this case, the diameter of the trephine must be greater than the diameter of the implant so that the cutting tool can pass parallel to the surface of the titanium support without touching it. If segmentation splits the implant at its widest part, which unfortunately results in a significant spread of titanium debris, a narrower trephine can be used to preserve additional bone. Once the body of the implant is no longer in contact with the surrounding bone, a small root elevator is penetrated circumferentially to destroy the apical portion of the structure in the underlying bone.
The procedure for removing an implant is quite delicate when it comes to removing the apical part of the structure, when the implant is close to adjacent teeth, the sinus cavity or the mandibular nerve canal. Planning for such a procedure is carried out with the mandatory use of cone-beam computed tomography (CBCT), which allows assessing the condition of bone tissue in all projections. Photo 3 shows one implant that was removed using reverse torque and a second that was removed using a trephine. Since when performing osteotomy with a trephine, the resulting bone tissue defect is larger than the size of the initially installed implant, such areas are quite difficult to re-implant, especially if we are talking about immediate implantation. In some cases, wider diameter implants are used to compensate for this outcome. In this case, it is necessary to remember to ensure a distance of 1.5-2 mm between two adjacent implants and teeth, and 3 mm between two adjacent implants. Photo 3 shows an implant fracture that formed adjacent to the fracture of the 13th tooth. After removing the defective structure and tooth, two new implants (Astra Tech, Dentsply Sirona) were installed in their place, using both the existing and additional volumes of bone tissue to stabilize them (photo 5).
Photo 3: Two implants removed using two different techniques. The narrow implant was removed with a reverse torque instrument, and the wide implant was removed using a trephine.
Photo 4. View of the implant that was removed using a trephine. After removal, an implant with a wider diameter was installed in place of the defective structure. Along with implantation, an augmentation procedure was performed.
Photo 5. View of the implant that was removed using a trephine. After removal, an implant with a wider diameter was installed in place of the defective structure. Along with implantation, an augmentation procedure was performed.
If it is impossible to carry out one-stage implantation, the area where the titanium support was removed should be restored using bone augmentation, wait until the required level of bone organization for 4-6 months, and only then proceed with re-implantation. In isolated cases, another, wider implant can be installed in the area of implant removal without violating either the aesthetic or functional criteria of rehabilitation (photos 6 - 10).
Photo 6. View after removal of a 3.6 mm implant using a 4.0 mm trephine.
Photo 7. After removal, an implant with a wider diameter of 4.2 mm was installed. Along with implantation, an augmentation procedure was performed.
Photo 8. Augmentation in the implantation area using a bone graft and collagen matrix.
Photo 9. Augmentation in the implantation area using a bone graft and collagen matrix.
Photo 10. View after suturing.
After explantation of a 3.6 mm diameter implant that tapered to 2.5 mm apically, a 4.2 mm diameter tapered implant with an apical diameter of 2.5 mm (Astra Tech, Dentsply Sirona) was placed. In this case, it was possible to achieve adequate immediate stability of the intraosseous structure. An additional augmentation was installed on the vestibular side of the implant, since the bone in this area was resorbed as a result of the development of a fracture of the primary structure.
Incorrectly positioned implants
If the implant is not positioned adequately, remodeling of the surrounding hard and soft tissues sometimes results in exposure of the abutment and threads, thereby compromising the esthetic outcome of the treatment (Figures 11 and 12).
Figure 11: The implants were placed too vestibular, resulting in bone loss and soft tissue recession.
Figure 12: The implants were placed too vestibular, resulting in bone loss and soft tissue recession.
In such cases, it is sometimes best to first remove the defective implant, then perform augmentation, and only then reinstall the supports in the required three-dimensional position. With this approach, the amount of bone tissue removed during explantation should be minimal. For such purposes, it is best to use tools with reverse torque. Kuhn et al, who removed orthodontic implants in their study, found that the rate of complications when explantation with reverse-torque instruments was minimal, and certainly lower than when using a trephine for the same purpose. For implant removal, the level of reverse torque can reach values of 200 Ncm to resist the formed contact between the titanium surface and the jaw bone (photos 13 and 14).
Photo 13. Removal of implants using instruments with reverse torque.
Photo 14. View of removed implants.
It is important to note that the strength of osseointegration may be higher than the capabilities of the reverse-torque instrument used, in such cases secondary fracture of the implant or fracture of the instrument itself often develops. In such cases, a trephine is used to complete the explantation. This tool is often included in kits for removing wide, long or hollow implant structures. They are primarily designed to separate cortical bone at the ridge apex in the peri-implant area to reduce the force required to reverse torque during subsequent implant removal. Trephine designs used as additional instruments in reverse explantation are very thin and are not suitable for removing bone along the entire length of the intraosseous support. Attempts to luxate the implant while it is inside the trephine most often lead to a fracture of the trephine itself. For volumetric removal of surrounding bone tissue, wide trephines or special piezo instruments are used. With adequate use of reverse torque, it is possible to preserve the volume of surrounding peri-implant bone tissue as much as possible.
Contraindications for implant removal
It is important to note that not all implants with a compromised esthetic profile require explantation, especially if they support multi-unit restorations. An example of such a case is presented below. The implants were placed approximately 20 years ago, and it was only now that the patient's upper jaw began to show signs of recession (Figure 15). On the right side, there was a deficiency of keratinized/attached mucosa and bone tissue in the vestibular direction. However, the bone loss reported was not pathological, but rather the result of physiological remodeling (Figure 16).
Photo 15. As a result of physiological remodeling, bone loss and the development of recessions were noted.
Photo 16. Visualization of the level of bone loss after flap separation.
Bone tissue augmentation was carried out simultaneously with the installation of implants. Obviously, the existing loss of soft tissue level was associated with the formation of an appropriate biological width and the presence of a thin mucosal biotype in the patient. Recent studies by Linkevicius et al have shown that the presence of sufficient initial soft tissue volume is an important criterion for predicting the success of future implantation. In this clinical case, removal of the implant would have entailed the need to remove a fairly large prosthetic structure, so instead of explantation, a procedure for correcting the mucogingival profile was performed. After treating the implant surface with glycine and sterile saline, a collagen-bone matrix (OSSIX VOLUMAX; Datum Dental Ltd.) was fixed to the buccal side of all three problematic implants (Figure 17). After harvesting the subepithelial connective tissue graft from the hard palate, areas of bone augmentation were covered, as well as exposed areas of implants and abutments (Figure 18). At the end of the intervention, a coronal displacement of the flap was performed, which was fixed in a new position. 1 month after the intervention, a not complete, but significant restoration of the level of soft tissue coverage around the problematic intraosseous supports can be noted (photo 19).
Photo 17. Covering the affected teeth with a graft and membrane.
Photo 18. Installation of a subepithelial connective tissue flap collected from the palate.
Photo 19. After 1 month.
Given the circular loss of bone tissue around the implants, it was almost impossible to achieve a complete restoration of the aesthetic profile in the area of titanium structures. However, the doctor was able to stop the progression of the recession and achieve regeneration of a certain amount of bone tissue on the vestibular side, as well as increase the area of keratinized mucosa.
Discussion
At the beginning of the introduction of implants into dental practice approximately 30 years ago, achieving osseointegration was considered the end point of treatment. That is, the assessment of the success of treatment depended on the achievement of certain “bone” criteria. The patient in such conditions was considered an ideal candidate for implantation if there was sufficient bone tissue. Given the lack of knowledge about the prospective adaptation of soft and hard tissues to the installed implant, it becomes clear why so many titanium supports were incorrectly positioned. Nowadays, clinical cases with complex patients are solved with customized abutments, cemented restorations and pink ceramics. In addition, doctors now have a better understanding of the process of remodeling of the surrounding bone and gums throughout the entire period of operation of the intraosseous structure. To replace wide tooth sockets immediately after their removal, it has been proposed to use wide-diameter implants. The latter, of course, were not immediately crowned with noticeable success, but it became clear that even if there is a gap between the wall of the socket and the surface of the implant, it is subsequently filled with bone tissue. Currently, such gaps are easily filled with augmentation, and such regenerative methods of intervention can improve the aesthetic outcome of rehabilitation. Today, implantation has become a prosthetic-oriented type of treatment. That is, the doctor is already working, planning the intervention “from top to bottom,” using new technologies and file formats from DICOM to STL at the diagnostic stages. With such diagnostic capabilities, it is easy for the doctor to determine which patient needs augmentation during implantation and which does not. In addition, doctors now have a variety of software at their disposal that allows them to discuss individual treatment features with patients, balancing the level of their expectations with the predicted results. Equally relevant is the use of such software when removing implants and arguing for the patient the need to implement such a procedure. After all, in essence, explantation is not a death sentence, but another chance to achieve successful rehabilitation results.
conclusions
During the implementation of any treatment algorithm, diagnosis and intervention planning are key factors for predicting a successful outcome of rehabilitation. Even if the essence is to remove the implant. When explanting, the doctor must clearly understand the final result of the treatment and what the subsequent goals are. After all, after removal of the implants, the patient must also be provided with adequate socialization conditions for the period of installation of new titanium supports and restorations based on them. The patient should be familiar with all the risks, costs and treatment options so as not to raise their expectations in any way. The availability of new instrumental methods for removing implants helps to minimize the level of invasiveness of this manipulation and reduce the period of time required to achieve complete rehabilitation of a dental patient.
Posted by Barry P. Levin, DMD
What to do if an implant falls out
What to do if something goes wrong after prosthetics? Can the structure be saved or will it have to be removed?
The first thing to do when pain and swelling appears is to consult a dentist. Don't expect the problem to go away. The more time you waste, the more serious the consequences will be. You should not self-medicate; home remedies will not help maintain the prosthesis and relieve inflammation.
If signs of rejection are detected or an inflammatory process is diagnosed, the titanium structure must be removed. The resulting cavity is cleared of pus, granulation tissue, and necrotic masses. Antiseptic treatment is carried out.
A mandatory stage is local and general anti-inflammatory therapy. Taking antibiotics localizes the source of inflammation and destroys the pathogen. With proper treatment and timely treatment, signs of the disease can be stopped within 1-2 weeks. If you delay visiting the clinic, the consequences can be serious. Such patients usually require surgical treatment.
Removal procedure
The operation is divided into several stages and is carried out in one clinic visit:
- Patient preparation and anesthesia.
- Removing the crown - use special forceps to carefully remove the prosthesis, preventing its destruction.
- An incision in the gums gives access to the implanted structure and removes it.
- Treatment of the cavity with antiseptics, stopping bleeding, suturing.
- Analysis of a rejected implant, inflamed cavity.
- A course of antibacterial drugs.
Root extraction is an operation, so the dentist will definitely prescribe a course of rehabilitation, during which it is unacceptable to ignore routine examinations.