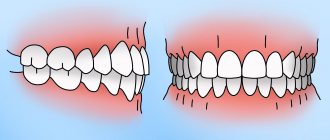
A deep bite is a developmental anomaly of the oral cavity in which the upper incisors almost completely overlap the lower ones. It not only distorts the proportions of the face, but can also cause speech disorders, increased tooth wear and trauma to soft tissues. Pathology can be detected both in early childhood and in adulthood. Treatment depends on the severity, but most often involves braces, plates, or orthodontic surgery.
Manifestations of distal bite in the mouth
Closing of lateral teeth during distal occlusion.
Distal occlusion is manifested in the mouth by the closure of the upper and lower teeth according to the “second class” (violation of the relationship between the projections of the antagonist teeth of the upper and lower jaw).
In the frontal segment (at the level of the front teeth) there are two closure options (the so-called first or second subclasses).
In the first case, a “sagittal gap” is observed, which reflects the discrepancy between the dentition in the sagittal plane (anterior-posterior direction). And the upper incisors are in protrusion (inclined forward). In the second option, the upper front teeth are tilted back (into retrusion). With the formation of a deep bite (when the lower teeth are not visible from under the upper ones).
Sagittal chain with distal occlusion. 2 class 1 subclass.
Distal occlusion. 2nd class 2nd subclass.
How to correct a protruding jaw?
It is possible to correct a protruding upper or lower jaw, but it is worth keeping in mind that this is a long process that will require time and effort. The easiest way to correct a protruding jaw is in childhood: bones that are in the process of growth are easier to manipulate. In adults, correction of the mesial bite can take several years.
All treatment methods can be divided into three categories.
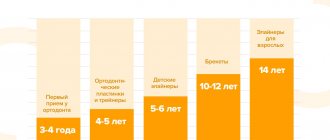
Gentle treatment - mainly used to correct protruding jaws in children under 12-13 years of age. As a rule, it involves inhibiting the growth of one of the jaws and stimulating the development of the other.
- Massaging the bone of the alveolar ridge is a stimulating effect that accelerates the development of the jaw.
- Wearing orthodontic structures - mouthguards, braces and trainers. Removable structures (trainers or LM activators) are effective starting from the period of primary occlusion. They can be used in the preparatory period before installing braces, thereby reducing the time of orthodontic treatment.
- Myofunctional gymnastics aimed at training the facial muscles. Orthodontists recommend starting to do such exercises for children from 2.5 to 3 years old, which will normalize maxillofacial development.
- Using vestibular plates to combat bad habits. Such techniques are used for primary and mixed dentition (aged 3 to 9 years), they are necessary to eliminate myofunctional disorders in the growing body. At the same time, the effectiveness of the exercises significantly increases (daytime training for 1 - 2 hours and wearing the device at night).
Orthodontic treatment
- This is a gradual correction of the position of the jaw using special devices that must be worn every day for a certain time (or constantly). In addition to the well-known brace systems (read more about braces in the article), more complex designs can be used. They change the direction of bone growth, pull the “lagging” jaw forward, expand the dentition, align and move teeth in the right direction. There are intraoral and extraoral systems. They are quite effective, but wearing them is associated with certain restrictions.
Surgical treatment
— surgical correction of a protruded jaw.
- Plastic surgery (trimming) of the frenulum of the tongue is prescribed for children 5-6 years old and can effectively correct the bite during the period of changing teeth.
- Tooth extraction helps reduce the size of an overdeveloped jaw.
- Osteotomy is a radical way to get rid of a protruding jaw. Prescribed to patients over 18 years of age when other methods are ineffective or have failed. During the operation, the jawbone is sawed, placed in the desired position and fixed with titanium structures. Read more about orthoganic surgery here.
Causes of distal bite (distal occlusion)
They are almost always (in the vast majority of cases) skeletal...
- Posterior position of the lower jaw. This is the most common cause of distal occlusion
- Small (short) lower jaw.
Many people write that the cause of a distal bite may be an overdeveloped (excessively large) upper jaw. They say that this is why there is a “gap” between the front upper and lower teeth (sagittal gap)... Many years of observations and our experience have shown that this is not so. With any anomaly of occlusion, there can be no talk of any OVERdevelopment. Everything, on the contrary, is UNDERdeveloped.
The lower jaw ends up in a posterior position (the first reason) only because the lower teeth bump into the upper teeth while the upper jaw is shortened and narrowed (generally underdeveloped). Or, when the upper incisors are “wrapped” back, into retrusion (second subclass). In addition, with distal occlusion, the upper jaw is always narrower than the lower jaw. Which, by the way, is another reason for blocking the lower jaw in the posterior position. And this same “blocking” does not allow the lower jaw, which is caught in the trap, to develop normally. Here is the second reason for distal occlusion - underdevelopment of the lower jaw.
There is also a “dental” reason for distal occlusion. Or more precisely, the dental cause of closure is “second class”. This is when mesial (front) displacement of the upper lateral teeth occurs. And then, even with a normal relationship of the jaws in the sagittal plane, the closure of the lateral teeth (molars) will also be in the second class. True, this is not a true distal occlusion...
A “dental” cause of the second class may complement or may camouflage true distal occlusion. Therefore, it will not be possible to figure out what is the reason for the closure in class 2 visually (by eye). Diagnostics required.
Prevention methods
Parents can prevent malocclusion in their child if they take care of their oral health and visit a specialist once every six months.
Habits that should alert a parent:
- sitting, the child constantly props up the same cheek with his hand;
- often touches growing teeth with tongue or hands;
- asymmetrical arrangement of the jaws.
Sleeping on the wrong pillow can be harmful: too high or low. This leads to curvature of the spine and malocclusion.
Only a doctor can make an accurate diagnosis. If you see the listed signs in your baby, visit the Russdent clinic. Our specialists will quickly and painlessly carry out a competent diagnosis and choose a strategy for further work with the patient.
Treatment at Russdent
Our clinic employs the best doctors who have extensive experience and constantly improve their skills through training. In addition, the clinic has modern equipment, which is important for early diagnosis. We use up-to-date treatment methods that provide high effectiveness even in difficult cases. These are the American systems “Damon Q”, “Damon Clear”, “H4”, as well as the lingual systems “Win” (Germany), “Incognito” (USA). For soft correction, transparent Invisalign aligners are used.
For more detailed information, please contact the clinic for a consultation.
Diagnostics
The main goal of any diagnosis is to identify the cause of the problem. And make a diagnosis. Likewise, the diagnosis of distal occlusion is designed to identify the cause of closure in the second class. In order to separate the flies from the cutlets during treatment, so to speak. That is, dental causes of closure are in the second class from non-dental (maxillary, skeletal).
The main diagnostic methods are:
- Analysis of TRG (teleradiogram) of the skull in a lateral projection. It allows you to clearly determine all the skeletal (jaw) nuances of the problem. Both with the position of the jaws and with their sizes.
- Analysis of plaster models of jaws (for this, casts are taken). It allows you to clarify the “dental” nuances: the size of the teeth, the length and width of the dentition, the features of the relationship (including closure) of the upper and lower teeth
Analysis of TRG (teleradiogram) of the skull in a lateral projection.
Analysis of plaster models of jaws.
It is not recommended to fall below this diagnostic “bar”. Below - just by eye. But this, as we understand, is not the best option.
Diagnostics is the first and key step in the treatment of distal occlusion. Do you want to know why it’s impossible to do without diagnostics?
Evolution of tooth size
Our distant ancestors, who lived about 100,000 years ago, had very large teeth - about twice as large as those of modern humans. This was a vital necessity. With the help of teeth it was necessary to gnaw animal bones and tear raw meat. But with the development of the brain and changes in diet, they gradually decreased. Scientists have calculated that every thousand years, 1% of their surface “gone” (although it is possible that over the past centuries this process has accelerated significantly).
The changes affected not only the overall size of the teeth, but also their purpose. The largest tooth in modern humans is the first upper molar: in the process of evolution, the main functional role has passed to it from the second upper molar. The fangs, which were no longer so important for holding food, were transformed the most.
Errors in the treatment of distal occlusion
The first, main mistake is that many try to treat distal bite with one device. For example, only with braces (this is the most popular option). But braces, although a cool device, are not for skeletal problems. The level of hardware competence of the braces system does not extend further than “to place the teeth on the jaw.” And distal occlusion, as we have already said, is a purely skeletal problem. Jaws and posture are to blame. And braces are not capable of solving problems with posture or jaw problems. After all, braces cannot change the position or size of the jaw. No matter what the would-be doctors promise...
And therefore, such videos are just an advertising gimmick.
Or rather, a convenient “hook” that catches gullible patients. Convenient because it coincides with the desire to do everything quickly and efficiently... But it doesn’t coincide with reality.
And braces cannot be the main device in the treatment of distal occlusion.
Braces are the wrong choice when treating distal malocclusions. In any case, you definitely shouldn’t start with them. Braces, as mentioned and shown above, can be effectively used only at the final stage of treatment of distal occlusion. All major “feats” must be accomplished before working on the teeth. Before using braces. And they are accomplished at the level of the jaws and skeleton (posture). Otherwise, there will simply be nothing to “clog” (close) these teeth (read with braces). See “Fundamentals of the therapeutic concept of “Ortho-Arteli”.
The second common mistake in correcting distal occlusion is treatment with the removal of upper premolars (4 or 5 teeth).
And this mistake is much more serious. Because it can have the most dire consequences. See "Orthodontic treatment with tooth extraction."
After all, as we said above, the main causes of distal occlusion are skeletal. And most often the lower jaw is to blame. And if so, then a reasonable question arises: if the lower jaw is to blame, what does the upper teeth have to do with it (their removal). Where is the logic?
In general, all errors in the treatment of distal occlusion in an adult are usually associated with insufficient diagnosis. Which entails a misunderstanding of the reasons for the occurrence of distal occlusion in each specific case.
For example, the “dental” cause of distal occlusion is very often confused with the “skeletal” (jaw) cause. We remind you that in the first case you need to move the lateral teeth back. And in the second - to push the lower jaw forward and develop the upper one. And if you get confused, if you don’t figure it out... Start distalizing the upper teeth, or worse, remove them when it is necessary to advance the lower jaw... Or vice versa. It is clear that nothing good will come of it.
The third mistake is when, without understanding what’s what, what exactly is the cause of distal occlusion, but realizing, however, that the problem cannot be corrected with braces, they try to solve the problem surgically. Using orthognathic surgery. Through osteotomy of the lower and upper jaws.
This is where I would like to dwell in more detail. And explain something. Why do orthodontists send to a surgeon to “treat” a distal bite? They have already said: they understand that braces will not cope. But they don’t understand how to treat it without braces. They don’t understand because in dentistry in general, and orthodontics in particular, there are a lot of prejudices regarding the possibilities of moving the lower jaw forward and developing the upper jaw. And these, as we saw above, are the main (“key”) points in the treatment of distal occlusion.
Most orthodontists simply do not believe in this (that it is possible in principle). Because someone (even a “great one”) said two hundred years ago that this cannot be done. Time has passed. Everyone has already forgotten why it is “impossible”. But no one even bothered to check why, in fact, it was impossible...
And therefore, those doctors who blindly believe in these moss-covered “dogmas” simply do not see an alternative. And for them there are only two extreme poles in the treatment of distal occlusion: braces and surgery. That's all.
During a direct examination by a specialist, you will be able to find out your exact diagnosis, as well as receive a referral for diagnosis or a treatment plan.
And in our clinic we treat distal occlusion between these two poles. Using methods of maxillofacial orthopedics and craniodontics. Here are the ones: changing the position of the lower jaw and changing the size of the upper. And we get good results, without regard to the fact that someone once said something... We must always double-check what was said. We checked. And everything turned out to be somewhat different. Or rather, not at all the way they “frightened” us. You can also push it out. It can be developed. You just need to know how, because there are some “secrets” here. And we, at the Orto-Artel clinic, knowing these “secrets”, take advantage of these opportunities, successfully eliminating distal occlusion of any complexity.
By the way, if we are talking about surgical treatment of distal occlusion, then we need to determine when and in what cases surgery is generally appropriate. But the indication is basically the same - a small lower jaw, the so-called lower micrognathia, and the micrognathia is very pronounced.
We indicated this reason above as one of the skeletal reasons. I will add: the lower jaw should be VERY short. Literally ugly. Only then can this be resolved surgically. In all other cases, you can do without surgery. Proven and tested many times.
By the way... In our clinic, a good half of the patients have formal indications for surgical treatment of distal occlusion. But only a few got to the surgeon. Because formalities are formalities, but compromise solutions were found that satisfied everyone: both the patients and us. This is because we approach treatment not formally, but in essence. And we are guided by logic and common sense.
Well, as a special case of a short lower jaw, which cannot be corrected except by surgery, this is a small chin. If it is small and spoils the face, then even by pushing the lower jaw forward we will not get the aesthetics we want. Simply because orthodontists do not have the means and instruments (devices) to selectively influence the chin. It is impossible to stimulate the chin to grow. Only surgery.
Inferior micrognathia.
This is where the indications (and there is essentially one) for surgical intervention for distal occlusion end.
Going with a knife into the upper jaw - God forbid! Even if the upper jaw is indirectly to blame for the distal occlusion. More precisely, the upper jaw also, as a rule, suffers (dimensionally) with distal occlusion. The upper jaw is directly connected to the base of the skull. And such interventions can then backfire. Literally. And the most important thing is that there is no need to go there surgically. The upper jaw can be developed!!!
Why is the jaw pushed forward and why is it dangerous?
The development of maxillofacial pathology most often begins in infancy or even in the prenatal period. Almost half of the cases are due to hereditary factors, but there are a number of external reasons why the jaw protrudes forward:
- taking medications during pregnancy that lead to the development of fetal pathology;
- injuries sustained by the baby during childbirth;
- rickets suffered at an early age;
- too short frenulum of the tongue;
- bad habits in infancy - prolonged pacifier sucking, sleeping in the wrong position;
- prolonged biting of lips, cheeks, fingers or any objects (for example, sucking the lower lip and thumb leads to lengthening of the upper teeth, and the upper lip - the lower);
- lack of solid food by the time chewing teeth erupt (at 2.5 - 3 years), which leads to impaired chewing function;
- incorrect posture;
- premature loss of baby teeth;
- diseases of the ENT organs and associated difficulties in nasal breathing.
All types of malocclusion have a significant impact on appearance. People with a protruding lower jaw appear gloomy and angry, and their facial features appear rough. Those with a distal bite often slouch and tilt their heads forward, and a small chin is associated with a weak character. But aesthetic problems are not the only difficulty that patients face.
Moving the jaw forward can lead to a number of other disorders:
- joint mobility is impaired and pain occurs;
- the likelihood of diseases of the temporomandibular joint increases;
- diction is impaired;
- difficulties arise with chewing food, gastrointestinal diseases develop;
- due to malocclusion, tooth enamel may wear down unevenly;
- the risk of periodontal disease/periodontitis increases;
- persistent disturbances in sound pronunciation appear, persisting even after 6–7 years (dyslalia);
- Dental prosthetics becomes more complicated.
- Due to improper redistribution of the chewing load, caries more often affects the back teeth.