Symptoms Classification of periodontitis Causes Possible complications How is it diagnosed?
Treatment Options Home Treatment Is Periodontitis Contagious? Recovery from severe periodontitis Differences from periodontal disease Prevention Periodontitis is an inflammatory periodontal disease that, without appropriate treatment, leads to destruction of the periodontal junction and tooth loss. It begins with inflammation of the gums, which occurs as chronic gingivitis. Subsequently, the pathological process affects deeper tissues, leading to the destruction of the periodontium, dental alveoli (socket), and the adjacent jawbone.
The tooth and periodontium are a single functionally and morphologically related system. The defeat of its individual elements disrupts the functionality of the dental unit, leads to disruption of the periodontal attachment, the formation of deep periodontal pockets, the formation of abscesses, fistulas on the gums, loosening, and tooth loss.
Generalized periodontitis: symptoms and treatment
Periodontitis is a very common pathology of periodontal tissues (soft tissue structures around the dental unit). If the pathological process is started and left without treatment, then you can lose all the dental units.
Periodontal pockets are the best location for the emergence and development of an infectious process, which does not have the best effect on the healthy state of the body. A beautiful and healthy smile gives you self-confidence and makes you feel natural. When periodontal tissue is damaged, the gums become red and swollen. The disease affects the overall health of the body and the well-being of a person. If something bothers you in the oral cavity, you should immediately consult a specialist. Dentist therapists at the branches of the West Dental family clinic in Yanino-1 and Vsevolozhsk will help with identifying the origins of anxiety and their treatment.
It has been scientifically determined that the occurrence of periodontitis is influenced by: soft plaque and hard deposits; filling material or orthopedic structure fixed in violation of treatment protocols.
HOW DOES GINGIVIT MANIFEST, AND WHY DOES IT OCCUR?
With superficial inflammation of the gums (if only soft gum tissue is involved in the process), we are dealing with gingivitis. Inflammation can occur in the area of 1 - 2 teeth (local gingivitis) or all teeth (generalized gingivitis).
Inflammation of the gums usually begins with damage to the gums, for example, when eating, brushing teeth, an incorrectly applied filling or crown, or a chemical burn. In this case, pathogenic microorganisms penetrate the injured gum and intensify the inflammatory response. The presence of soft plaque, tartar, and poor oral hygiene are mandatory conditions, and very often an independent cause of the onset and maintenance of the disease.
Gingivitis is often observed in people with malocclusions, crowded teeth and their incorrect position. A short frenulum of the upper and lower lips is also a risk factor for periodontal disease.
Smoking plays an important role (spasm of blood vessels occurs, gum nutrition deteriorates), decreased body defenses (immunodeficiency), lack of vitamin C and other risk factors.
In the acute stage of the process, pain, burning, swelling of the gingival margin, and bleeding when brushing teeth are usually noted. If the cause of the disease is not eliminated, then acute gingivitis becomes chronic, which does not go away on its own without treatment. In this case, the gums turn blue and periodically bleed when brushing your teeth and eating. There is an unpleasant odor from the mouth.
Severe forms of gingivitis, such as ulcerative gingivitis, are observed in severe general diseases of the body. For example, with diabetes or a serious immunodeficiency disease. In this case, the temperature rises, painful ulcers covered with a film appear on the dirty gray gums, and general health worsens.
With gingivitis, the teeth remain stable, since the process does not penetrate deep into the periodontium, the so-called periodontal pocket does not form, and the bone tissue of the tooth socket does not dissolve. Can there be consequences if gingivitis is not treated?
If gums are not treated in time, gingivitis will develop into periodontitis. This is a much more serious and dangerous disease than gingivitis. Often it becomes irreversible, since periodontitis affects and destroys the deep tissues of the periodontium - the ligaments of the tooth and the bone tissue of the jaw.
Classification
According to the number of units affected by pathology:
- Catarrhal (localized) – 1-3 units in the affected area;
- Generalized – the entire dentition is affected.
According to the severity of generalized periodontitis (ICD code K05):
- Generalized mild periodontitis (ICD 10 code K05.3). This clinical diagnosis is made when the depth of the pockets in the gingival tissue is less than 3.5 mm, and less than 1/3 of the root is resorbed.
- Average. The subgingival depressions are 3.5-5 mm, and the bone is sclerosed at 50% of the root length.
- Severe degree. This stage is indicated by the depth of periodontal changes greater than 5 mm and resorption of more than 1/2 of the root.
Differential diagnosis according to pathogenesis:
- acute - more than one annual exacerbation;
- chronic generalized periodontitis (according to ICD K05) is an ongoing pathological process;
- exacerbation of chronic periodontitis – pain, discomfort, activation of the inflammatory process.
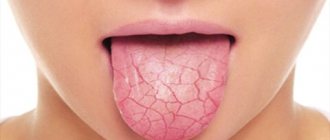
Symptoms
The initial symptoms of the inflammatory process in periodontal tissues are the following:
- swelling of the gum tissue;
- severe bleeding during and after cleaning;
- throbbing severe pain.
As the pathology spreads, symptoms intensify:
- enlarged and painful lymph nodes;
- unpleasant odor from the mouth;
- mobility of dental units;
- increased sensitivity of tooth enamel;
- pain when biting and chewing food;
- deterioration of the general condition of the body;
- purulent discharge from periodontal pockets.
Chronic generalized periodontitis (beyond exacerbation) is characterized by:
- reddish color of gum tissue;
- exposure of tooth roots;
- Bone resorption is visually determined on the Rg image.
WHAT IS A PERIODONTAL EXAMINATION?
The history of the disease (anamnesis) is carefully determined. When did it first start, what was done for treatment, do parents and close relatives have this disease, etc. Careful collection of data makes it possible to determine risk factors and sometimes even predict the course of the disease. This is followed by a careful examination of the oral cavity: the frenulum of the lips and tongue, the dental arches as a whole and, if necessary, each tooth separately, as well as fillings, crowns and orthodontic appliances are assessed.
One of the main examination methods is probing the periodontal pocket of each tooth at six points. The presence of tartar and soft plaque, bleeding, suppuration, tooth mobility, etc. is assessed. This labor-intensive analysis is painlessly performed in 15 - 20 minutes using a special electronic probe of the automated computer clinical diagnostic system Florida Probe (USA). The patient’s personal data is stored in the computer’s memory, which makes it possible to predict the course of the process and select treatment, as well as evaluate the dynamics of the disease and the effectiveness of the treatment.
An orthopantomogram is a necessary element in the diagnosis of periodontal diseases. This image shows the teeth, jaw bones, and the partitions between the teeth. Digital orthopantomographs (such as the ones in our clinic) allow you to obtain excellent images with minimal radiation exposure to the patient and evaluate them on a computer screen using auxiliary computer programs.
Chronic generalized periodontitis
Chronic generalized periodontitis (according to ICD 10-K05) affects the soft tissue and bone structures of all or more dental units. The frequency of occurrence is 5 times higher than carious lesions and its possible complications. Also, a generalized process can most likely lead to complete edentia (lack of teeth). The long-term location of the infectious process in periodontal tissues, without proper treatment, negatively affects the body's immune defense and can contribute to the development of rheumatoid arthritis, heart disease, etc. Generalized periodontitis has a different etiology.
WHAT IS MEAN BY PERIODONTAL TREATMENT
After collecting all the necessary information, the periodontist will discuss the condition of your gums with you and suggest the most optimal treatment. Most importantly, it must be comprehensive - that is, treatment must cover all identified causes and associated factors that support the disease. Only in this case can it be possible to completely cure or stabilize periodontal disease for a long time.
Treatment will be much more effective if the patient strictly follows all instructions and strictly follows the chosen treatment plan.
Typically, a comprehensive treatment plan consists of general and local treatment and includes all or part of the methods listed below.
Diagnostics
To determine the disease and its severity, various diagnostic methods are used. For generalized periodontitis, differential diagnosis includes an extensive consultation examination to draw up a medical history (formation plan):
- collection of complaints (mobility of units, discomfort when chewing, periodic sharp pain in the attached gum);
- visual and instrumental examination (gingival pockets, recession of gingival tissue, dental plaque, reddish gums);
- determination of the color, shape and structure of gum tissue;
- finding out what condition the dental units are in: percussion, palpation, degree of mobility;
- determination of hygiene indices;
- RG images.
Sometimes, a specialist may prescribe a blood test to clarify the etiology.
Diagnostic measures should take into account not only all the symptoms of the pathology and the patient’s complaints, but also the mandatory performance of an X-ray. Basically, in case of periodontitis, it is recommended to perform an OPTG (orthopantomogram) - a panoramic image. In such an extensive image, all dental structures and the degree of bone damage in each unit are immediately visible.
ARE THERE METHODS FOR PREVENTION OF PERIODONTAL DISEASES?
- Prevention of periodontal disease consists of several simple points:
- Brush your teeth 2 times (morning and evening) after meals. Use a toothpaste recommended by your doctor to protect your gums. Use an electric toothbrush - it perfectly cleans your teeth and massages your gums.
- Do professional oral hygiene at least 2 times a year, and at the same time you can undergo an examination by a periodontist. Do not use any medications for the treatment or prevention of periodontal disease (gels, ointments, tablets, etc.) without consulting your dentist.
- Do not eat only soft and delicate foods - your teeth should receive normal, natural stress.
- Your diet should be well balanced, contain the required amount of proteins, fats, carbohydrates, and vitamins. If you are deficient in vitamins, take multivitamin complexes.
- Lead a healthy lifestyle.
Mild degree
As usual, mild degrees are not given any importance. A subgingival pocket is formed near the dental unit, where microorganisms accumulate. There are signs of periodontal inflammation, and on the Rg image there is destruction of bone tissue by 1/3 of the root, gum pockets up to 3.5 mm. In the cervical area of the teeth, hard deposits are observed, the gums are loose, slightly inflamed and swollen. There is slight bleeding when cleaning, and discomfort when chewing solid food. Mobility and movement of teeth is not observed at this stage.
WHAT IS PERIODONTAL
The periodontium is the complex of tissues surrounding the tooth. These include not only the gums, but also the bone socket in which the tooth root is located, and the tooth ligaments that hold the tooth in the socket, intertwined with the tooth root and bone. All these tissues represent a single system that performs several important functions at once: fixation of teeth, perception and regulation of chewing load, control of the work of masticatory muscles, protection against penetration of pathogenic bacteria and a number of damaging factors into the bone tissue.
Average degree
With moderate severity, periodontal pockets up to 5 mm are observed. The x-ray shows damage to the bone septa on half the root. In the oral cavity, upon examination, there is a sufficient number of dental deposits, mobility of teeth I-II degrees, inflammation of the gums. A small amount of pus may ooze from under the gums. When the process worsens, slight mobility and displacement of units occurs.
Patients complain of pain in the gums; pain and bleeding when eating; the necks of the teeth are exposed; a reaction to cold and hot food is formed.
Differences between periodontitis and periodontal disease
| Periodontal disease | Periodontitis | |
| Pathogenesis | Systemic dystrophic periodontal disease | Infectious and inflammatory periodontal disease |
| Character of the course | Develops slowly, asymptomatically | Develops quickly, often recurs, symptoms clearly manifest themselves in the acute period |
| Causes | Mainly systemic pathologies of the body, hereditary predisposition | Poor hygiene, excessive bacterial plaque, tartar, malocclusion, jaw injuries |
| Prevalence | A segment of teeth or the entire dentition is affected | Inflammation is localized in the area of one, several teeth or affects the entire jaw |
| Inflammation and bleeding gums | Absent | Main features |
| Tooth mobility | Occurs when gum recession extends more than 1/2 the length of the tooth root | It is observed in the acute period of the disease, against the background of looseness, swelling, and bleeding of the gums. Disappears after treatment |
| Forecast | Requires constant, maintenance therapy. In moderate and severe forms, the process only needs to be stabilized. The overall prognosis is poor (tooth loss) | With timely treatment, complete recovery |
Severe degree
Chronic generalized severe periodontitis, as diagnosed, is determined by deep periodontal pockets over 5 mm and 2/3 of the tooth root being exposed. With this degree of pathology, great swelling, bleeding and hyperemia of the gums occurs, and eating is quite painful. In periodontal pockets there is a large accumulation of pus and microorganisms in the form of dental deposits. Patients have complaints of pain, itching, burning and pulsation in the gums. It is impossible to carry out high-quality hygienic cleaning on your own; a persistent unpleasant odor persists for a long time. In the absence of proper therapy, severe suppuration and mobility of grade III-IV units are observed, up to prolapse. Complications may develop in the form of abscess formation of foci of infection and periodontal disease.
Also, this pathology is manifested by a violation of the general condition of the body. A person is worried about weakness, fever, and in connection with this, fatigue. Regional submandibular lymph nodes enlarge and become painful on palpation.
Is it possible to treat at home?
Decoctions of medicinal herbs (tricolor violet, calendula, lingonberry leaf, calamus, oak bark) will help relieve symptoms of acute inflammation. But no amount of rinsing will get rid of supragingival, and especially subgingival dental plaque. Only professional hygienic cleaning at the dentist's office can handle this. Folk remedies in the form of formulations of hydrogen peroxide, soda and lemon will only aggravate the situation. But maintaining the condition of your gums after treatment at home is not only possible, but also necessary. The dentist will give you all the necessary recommendations on how to treat periodontitis at home.
Treatment
When the pathological process has taken the form of chronic generalized periodontitis, it is more difficult to carry out effective treatment. It is important to address the underlying cause of the disease. In this regard, the generalized form of periodontitis requires consultation with dentists in related fields to identify the source of the pathology. The general dentist/periodontist can provide recommendations for consultation with an endocrinologist, hematologist, immunologist, etc. After general interaction and identification of the cause of periodontitis, the attending physician prescribes the necessary therapy.
Treatment of the pathological process consists of the following measures:
- Professional oral cleaning and hygiene training. A specialist removes soft and hard dental deposits, including those under the gums. The tooth enamel is polished with special brushes with paste and coated with a protective gel with fluoride. Oral care products are selected and instructions on their use are provided.
- Treatment of associated dental problems. To cure periodontitis, it is important to treat caries, pulp disease, and pathological processes in the gums and bones.
- Drug therapy. Oral baths with solutions, application ointments, NSAIDs and painkillers, and sometimes antimicrobial drugs are used.
- Removal of subgingival pockets by a dental surgeon. In case of moderate and severe severity, it is possible to perform open and closed curettage of pockets, as well as gum plastic surgery.
- Treatment using orthopedic structures. As part of complex measures, temporary splinting of mobile units is performed with an orthodontic retainer or fiberglass; selective grinding of the chewing surfaces of teeth; prosthetics of large dental defects to redistribute chewing pressure.
- Physiotherapeutic manipulations. Many physiotherapy procedures have a positive effect on recovery: UHF, infrared radiation, magnet and laser therapy, electrophoresis, direct and alternating current, vacuum and acupressure massage, paraffin therapy, mud therapy.
For effective treatment of pathology and the occurrence of remission of the process, it is important to fully comply with the specialist’s instructions.
Medical Internet conferences
Acute periodontitis
It is often focal and has a sudden onset with a pronounced clinical picture. Severe pain appears, bleeding gums, inflammation of the gums in a certain area, pain when chewing with teeth located in this area.
There are three stages of the disease:
• Mild degree - there are no visible changes, but itching, bleeding and hypersthesia in the gum area appear.
• Moderate degree - pain, increased bleeding and looseness of gums, periodontal pockets, and tooth mobility appear.
• Severe degree - atrophy of the gums and alveolar processes occurs with exposed necks of the teeth, which ultimately leads to their loss.
Treatment of all stages of acute periodontitis should be carried out comprehensively. General treatment consists of boosting the body’s immune system with a balanced diet, biologically active substances and vitamins. Local treatment includes: removal of tartar, massage of the gums and rinsing of the gums with disinfectant solutions, followed by proper hygienic care of the oral cavity and, if necessary, prosthetics.
Chronic periodontitis
During the course of the disease, alternating phases of exacerbation and remission occur.
Depending on the severity of pathological changes in the periodontium, there are 4 degrees of severity of chronic periodontitis:
• Initial degree - there is itching and pulsation in the gums, loose bleeding gums, a feeling of discomfort when chewing food, and bad breath. When examining the oral cavity, signs of catarrhal gingivitis, the presence of dental plaque and shallow periodontal pockets are revealed, but the teeth remain immobile.
• Mild degree - characterized by the progression of pathological changes. Pain, swelling and bleeding of the gums increases. Soft plaque quickly accumulates, tartar forms, the necks of the teeth become exposed and become hypersensitive. When examining the oral cavity, signs of gingivitis are revealed; periodontal pockets, when pressed on them, release pus. The teeth begin to loosen.
• Moderate degree – increased bad breath, bleeding gums, gums change color, purulent discharge from pockets, gaps between teeth, exposure and hypersensitivity of the necks of teeth to temperature and chemical influences. The teeth are mobile.
• Severe degree - characterized by severe symptoms: increased pain, bleeding gums, mobility and displacement of teeth, swelling of the gums, abundant dental plaque, diffuse gingivitis. Loss of individual teeth is noted.
Exacerbation of chronic periodontitis is accompanied by a sharp deterioration in the general condition of the patient, severe general intoxication is observed, and sharp throbbing pain appears. The severity of chronic periodontitis is determined based on X-ray and orthopantomography data. To determine the microbial contamination of periodontal pockets, PCR scraping and bacteriological inoculation on nutrient media are performed. Chronic periodontitis is differentiated from gingivitis and periodontal disease based on gum biopsy data.
Treatment depends on the severity and includes non-surgical and surgical methods. In the initial and mild form, conservative treatment is carried out, which includes the removal of dental plaque and treatment of the oral mucosa with antiseptic drugs: hydrogen peroxide, chlorhexidine, furatsilin, and anti-inflammatory applications complement the treatment. Physiotherapeutic procedures are prescribed: electrophoresis, laser therapy, darsonvalization, ultraphonophoresis, ozone therapy. Next, the patient is given recommendations on maintaining oral hygiene and using hygiene products [1-3, 5].
Moderate treatment is supplemented with antibacterial therapy to increase immunity, followed by closed and open curettage with medicinal treatment of periodontal pockets. If necessary, therapeutic splinting of mobile teeth is performed.
Severe cases are treated with a combination of therapeutic and surgical methods. In addition to the procedures of local and systemic anti-inflammatory therapy, according to indications, teeth with pathological mobility are removed, gingivectomy, flap operations are performed, and periodontal abscesses are opened.
With timely and correctly carried out complex treatment of chronic periodontitis and the patient’s further compliance with recommendations, the function of the dental system can be restored for a long time.
Generalized periodontitis
It is characterized by bleeding, swelling and looseness of the gums, itching, pulsation and burning in the gum area, pain when chewing food, bad breath, the presence of dental plaque, and the formation of periodontal pockets. In addition to the listed symptoms, loosening and displacement of teeth, increased sensitivity of teeth to temperature stimuli, and difficulty chewing food are also typical.
In severe cases, generalized periodontitis may be accompanied by general intoxication, enlarged regional lymph nodes, and acute pain in the gum area. In this case, there is an abundant accumulation of soft plaque and tartar, multiple periodontal pockets, often with purulent contents. In advanced stages, generalized periodontitis can lead to the formation of periodontal abscesses, fistulas and tooth loss.
In chronic generalized periodontitis in the remission stage, there is no dental plaque or suppuration. The gums are pale pink, the roots of the teeth may be exposed, but there is no bone resorption.
Depending on the severity of the disease, there are three degrees of generalized periodontitis:
• Mild degree – the depth of the periodontal pockets is 3.5 mm; bone resorption does not exceed 1/3 of the length of the tooth root;
• Medium degree - depth of periodontal pockets up to 5 mm; bone resorption is 1/2 the length of the tooth root;
• Severe degree – the depth of periodontal pockets is more than 5 mm; bone resorption exceeds half the length of the tooth root.
Treatment of generalized periodontitis should be comprehensive. Includes local conservative and surgical treatment; general anti-inflammatory and immunomodulatory therapy. Complex therapy, according to indications, includes physiotherapy (medicinal electrophoresis, darsonvalization, ultraphonophoresis, laser therapy, magnetophoresis), hirudotherapy, ozone therapy, apitherapy, herbal medicine.
In case of mild disease, plaque removal, medicinal treatment of periodontal pockets with antiseptics, and periodontal applications are carried out [11 - 14].
When treating moderate periodontitis, the above procedures include curettage of periodontal pockets, application of therapeutic dressings, and grinding of tooth surfaces. If necessary, tooth roots or individual teeth are removed, therapeutic splinting and orthopedic treatment are performed, as well as general therapy.
Treatment of severe generalized periodontitis may require additional surgical intervention: removal of teeth of III-IV degree of mobility, gingivotomy or gingivectomy, flap surgery, opening of periodontal abscesses. According to indications, plastic surgery of the oral vestibule, osteogingivoplasty, and plastic surgery of the frenulum of the tongue and lips are performed. In severe cases of the disease, anti-inflammatory immunomodulatory therapy and vitamin therapy are mandatory.
Localized periodontitis
The localization zone of focal periodontitis is a small group of teeth or tissues around them. This form of the disease has an acute form, which, if left untreated, becomes chronic.
The disease occurs suddenly with the following pronounced symptoms in a certain area of the gum: pain when chewing, bleeding, redness, swelling.
Treatment of focal periodontitis should be comprehensive. The first stage eliminates the causes that contributed to the occurrence of the disease, and the second stage is aimed directly at treating the lesion itself. General treatment for focal periodontitis is not required, since the process is local in nature.
Elimination of the causes of the disease includes the removal of traumatic crowns and overhanging fillings, removal of dental plaque and antibacterial therapy. With a deep bite, deep incisal overlap, or progeny, selective grinding of the tooth tissues is performed. Antibiotic therapy is prescribed to eliminate the source of infection; the choice is made in favor of broad-spectrum antibiotics, which can be tetracycline or metronidazole.
Surgical methods are used when identifying an abscess and deep periodontal pockets: opening the suppuration, cleaning the damaged surfaces and subsequently treating the periodontal pockets.
Next, the patient is referred to dentists - orthopedists, where the design of medical orthopedic devices is selected.
Juvenile periodontitis
Juvenile periodontitis is characterized by the rapid destruction of periodontal tissues with the subsequent formation of periodontal pockets, displacement and pathological mobility of teeth. The process can begin almost asymptomatically, without the presence of a large amount of plaque and pain. At the onset of the disease, symmetrical periodontal damage occurs in the area of the incisors and first molars. Displacement of the first incisors and molars occurs in the labial, buccal and distal directions. Diastemas appear.
Juvenile periodontitis, in the absence of proper treatment, can also take a generalized form, when the entire dentition is involved in the pathological process.
When treatment for desmodontosis is started, it opens up the possibility of preserving teeth in patients. Treatment of juvenile periodontitis is currently carried out using antibiotics in combination with local treatment: curettage, gingivotomy with preliminary depulpation of teeth and the introduction of drugs that enhance reparative regeneration of bone tissue. With already developed stages, it may be necessary to remove damaged teeth and carry out orthopedic treatment.
Refractory periodontitis
Refractory periodontitis is a type of periodontitis that continues to develop despite ongoing therapeutic measures.
The disease occurs with a large number of complications and is accompanied by loss of bone tissue in several areas simultaneously.
After massive loss of supporting tissues, tooth loss occurs. Antibacterial therapy is used in treatment. The prognosis is not favorable. The lack of remission and cure is caused by poor oral hygiene, irregular visits for repeated examinations and, accordingly, lack of maintenance treatment.
Prepubertal periodontitis
Occurs after the eruption of baby teeth. The disease is characterized by almost complete premature tooth loss in children at an early age due to disruption of the attachment of the gums to the teeth and severe destruction of the alveolar bone. In this case, the gum tissue shows pronounced signs of inflammation. Sometimes gum retraction occurs with the formation of cracks. The process, starting with the loss of baby teeth, extends further to the rudiments of permanent teeth. The first sign of the disease is the coating of teeth with a soft coating. Then extreme tooth mobility occurs. At the same time, the child does not feel pain.
Non-surgical methods for treating the inflammatory process of periodontal tissue are the same as in adults - these are professional oral hygiene and various physiotherapeutic procedures. Surgical interventions, such as lip frenulum correction, may also be required.
Rapidly progressing periodontitis
The pathological process is localized simultaneously in the area of several teeth. Sometimes rapidly progressing periodontitis can be accompanied by systemic diseases such as diabetes [7, 9, 12], or Down syndrome. In this form of the disease, immediate destruction of bone tissue occurs, with active periods alternating with periods of remission. During the active period, there are pronounced signs of periodontal inflammation, the release of purulent exudate from periodontal pockets, which entails extensive damage to bone tissue. During periods of remission, the gums are slightly inflamed, bone tissue destruction does not progress.
Rapidly progressing periodontitis can be stopped as a result of therapy, but it is known that the disease often recurs.
Treatment is carried out in several stages:
o Conservative treatment includes removal of dental plaque, physiotherapeutic procedures, antiseptic treatment and anti-inflammatory applications.
o Antibiotic therapy to suppress pathological microorganisms that cause inflammation.
o Surgical treatment includes the elimination of periodontal pockets with treatment of tooth roots and bone defects of the alveolar process, which are filled with a synthetic graft, and subsequently the periodontal tissues are sutured. In case of pronounced destruction of bone tissue and alveolar process after flap operations of pathologically changed tissues and filling of bone pockets with a drug for filling bone cavities - “Kollapan”, 10-12 days after surgical treatment there should be a stabilization of the process and a significant decrease in the pathological mobility of teeth in the area of the performed surgical intervention. This will allow you to preserve and strengthen mobile teeth as much as possible, and subsequently use them as a support for various types of dentures at the stages of orthopedic treatment.
Ulcer – necrotizing periodontitis.
It has an acute onset; the preceding period can last up to two days. During this period, general symptoms appear. In parallel with them, catarrhal phenomena are observed in the form of swelling, redness of the gums, itching and pain appear. When brushing your teeth or chewing, your gums begin to bleed. Over time, ulcers form in the upper part of the gum edge, which are surrounded by a white-gray border and represent areas of tissue necrosis. When trying to remove plaque, bleeding will occur.
As a result of tissue necrosis, a putrid odor appears from the mouth. Even regular brushing of your teeth does not get rid of this unpleasant odor. In such patients, there is often an accumulation of food debris between the teeth. The disease can occur in mild, moderate and severe forms.
The main symptoms are general intoxication, dyspepsia, sleep disturbance, enlarged lymph nodes, bad breath, bleeding and sore gums, itching, and the appearance of viscous and viscous saliva.
Treatment of necrotizing ulcerative periodontitis can be both general and local. The main methods of treating this disease include: professional teeth cleaning to remove plaque and tartar, grinding sharp edges of teeth, using local anesthetics (Lidocaine or Novocaine), using antibacterial agents in the form of solutions and suspensions, and following a diet.
Painkillers should be used to lubricate the ulcerated areas in the gum area. The most commonly used antimicrobial drugs are chlorhexidine solution, hydrogen peroxide or Metronidazole in the form of a suspension.
It can be treated by applying proteolytic enzymes (trypsin). To eliminate inflammation of the gums, applications are used or rinsing is performed.
Of no small importance in the treatment of ulcerative-necrotic form of gingivitis are physiotherapeutic methods, which include laser therapy, ultraphonophoresis, and ultraviolet irradiation. To strengthen the body, it is advisable to prescribe vitamins. The diet involves excluding from the diet foods that can irritate the mucous membrane of the gums.
If conservative therapy is ineffective, when there are extensive necrotic areas, surgical intervention may be required. Necrotic tissue is removed. To prevent relapses of the disease, thorough sanitation of the oral cavity is organized after treatment. With adequate and timely treatment, the patient’s well-being improves within a few days. During drug therapy, epithelization of ulcers occurs.