Composition and application of microprosthesis
Compound
The prosthetic structure consists of a pin part that completely follows the shape of the root canal, and a stump that imitates the crown being restored. Most often, stump inlays are made from various metal alloys through precision casting. However, zirconium or aluminum oxide can also be used to produce prostheses.
Application
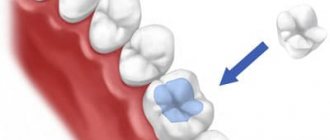
Standard cast pins are used to create tooth stumps with pronounced destruction of their supragingival part and the presence of healthy, strong roots. In this case, the tab is tightly fixed in the root canal so that its stump part protrudes above the gum. The stump can be used as a support for crowns, splinting structures, removable and fixed dentures.
In modern dental practice, collapsible and non-removable stump inlays are used.
Non-removable structures are used to restore teeth with one root, and collapsible ones are used to create tooth stumps with two or more roots.
Which material to choose
The selected material for making the inlay must meet a number of requirements: be hard and elastic, bioinert, shrink to a minimum during casting, and have low thermal conductivity.
Modern dentistry can offer the following options:
| Ceramic | Best suited for patients who prefer non-metallic crowns. Such inlays are also called cosmopost and are most often used to restore front teeth. The color of the inlay itself can be perfectly matched to the natural color of the tooth. For manufacturing, zirconium or carbon pins are used, onto which a ceramic crown is subsequently built up. There is also a mixed option - a stump inlay with metal-ceramics, it is much stronger than ordinary ceramic, so it can be freely used on teeth that perform the chewing function. |
| KHS (cobalt chromium) | Ideal for restoring chewing teeth that bear heavy loads is a cobalt-chrome core inlay. Such inserts are distinguished by high hardness and strength, but they are difficult to process, so the KHS insert is not suitable for a collapsible design. Moreover, the alloy of cobalt and chromium may cause an allergic reaction in some patients. |
| From gold | The safest, most aesthetic and hypoallergenic are gold stump inlays. Gold is a universal material that does not enter into chemical reactions, so products made from it are not subject to corrosion and destruction; moreover, it is more convenient to work with gold, since this metal is easy to melt, forge and post-installation processing. |
| Metal | Among metal stump inlays, inserts made of noble (silver, palladium) and non-precious (titanium, steel, cobalt, nickel, chromium) alloys are popular. The advantage of silver is its bactericidal properties, however, after installing a silver alloy insert, an oxide film begins to form around the tooth and on its surface, causing darkening of the enamel and pigmentation of the gum tissue. Titanium has the highest bioinert properties and high hardness, but it is not very convenient to work with due to its fragility. And the alloy of chromium and nickel is subject to severe shrinkage. |
In any case, if you decide to restore a damaged tooth using an inlay, rather than using standard factory pins, discuss your decision with your doctor in advance and get detailed advice on this issue.
Indications and contraindications for the installation of stump inlays
Indications for installation
Restoring teeth with core inlays is possible only if there is firm confidence in the reliability of the root and in the absence of any pathological processes in the periodontal tissues. The length of the root canal into which the cast post is installed must be greater than the height of the artificial crown, and the walls of the tooth must be thick enough to withstand the chewing load.
Contraindications for use
The main contraindications to prosthetics with stump inlays are:
- obstruction of the root canal or its curvature;
- pronounced changes in periodontal tissues in the absence of the ability to block the development of the pathological process;
- improper root length or tooth wall thickness;
- pathological mobility of teeth;
- incomplete filling of root canals.
Ceramic dental inlay: care features
The ceramic inlay and onlay do not require complex care. You need to care for your teeth like you would for regular teeth - brush twice a day, use floss and mouth rinses after each meal. It is worth noting that ceramic inlays, due to their physical properties, do not require additional care (unlike light fillings) - professional cleaning.
In order to promptly detect leaks in the Emax tab, you need to regularly visit the dentist’s office (once every six months). When a dark stripe appears, there is a high probability that pathogenic microorganisms have begun to penetrate under the ceramic inlay, which provoke the development of a carious process. On average, the service life of ceramic structures is about 7-8 years. Subject to all rules and hygiene standards, as well as the absence of increased stress, they can last several years longer.
You can install a ceramic inlay in Moscow at the reliable A-Medic clinic. Qualified specialists with extensive experience work here, which guarantees a positive result. The orthopedic design is no different from natural teeth and can last for many years. In the event that there are contraindications to the installation of this product, A-Medic dentists will be able to select another method of tooth restoration.
Stages of manufacturing and installation of cast pins
Prosthetics with core inlays involves a number of clinical and dental measures. In particular, the main steps in the manufacture and installation of cast pins are:
- preparing a damaged tooth for installation of a stump inlay (unsealing the root canals by 2/3 of their length, preparing the tooth aimed at eliminating possible undercuts);
- taking a two-layer silicone impression from both jaws;
- covering the prepared tooth with a temporary filling (crown);
- transfer of the silicone impression to the dental department;
- making a plaster model based on the cast made;
- modeling a cast wax pin;
- casting of the prosthetic structure in the dental department;
- transfer of the finished cast pin from the dental laboratory to the dentist;
- fitting and fitting of the prosthesis;
- final installation of the core inlay and its fixation using dental cement (glass ionomer is most often used) or dual-curing composite.
- After fixing the cast pin, a suitable crown or prosthetic structure is installed on the stump.
Stump inlay with a pin in the arsenal of dentists at the ALTEYDENT clinic
Despite the growing popularity of direct restoration with composite materials using build-up technology, it cannot be used:
- After repeated treatment using a resorcinol-formalin mixture, since the degree of adhesion of epoxy resins to the walls in this case decreases sharply.
- With a large volume of cavities after mechanical treatment of dentin, which leads to significant shrinkage of glass composites.
- When the crown is completely lost, or its borders are at least partially under the gum.
In all these situations, we strongly recommend that patients install a stump pin insert. This method of restoration is optimal for the loss of one tooth bordering on vital “neighbors.” The limitation for working with inlays is the violation of the integrity of the roots, which leads to the need for removal and subsequent implantation.
Our laboratory allows us to work at a high technical level using two technologies: model casting of chrome-cobalt inlays and CAD/CAM production methods from zirconium dioxide. The cost of metal cast stump pin inlays is RUB 3,000 . The price of a pin stump inlay made of zirconium dioxide is 8,000 rubles . Additional costs for inlay placement are related to the cost of pretreatment and the type of cement used.
Advantages and disadvantages of prosthetics with stump inlays
Prosthetics with cast pins, just like any other dental procedure, has a number of advantages and disadvantages.
Benefits of Tabs
The positive features of using core inlays to restore damaged teeth are:
- the possibility of completely restoring the natural shape of the replaced crown (lateral enamel ridges on its chewing surface, cusps, etc.);
- rapid normalization of the functions of the masticatory apparatus;
- monolithic structure (no risk of separation of the stump and pin);
- tight fit of the prosthesis to the root surface (minimizing wedging load).
Disadvantages of microprostheses
The main disadvantages of orthopedic dental treatment with cast pins include:
- the need for extensive preparation of the damaged tooth;
- long lead times for the manufacture and installation of a prosthetic structure (the presence of a laboratory stage, during which the pin is cast by a dental technician);
- high cost of stump inlays compared to standard pins.
NeoStom – Dentistry website
The manufacturing method and the sequence of clinical and laboratory stages of making the inlay depend on the material for its manufacture. The following methods are used: • with the preliminary creation of a wax model of the inlay with its subsequent replacement with metal (by model-free casting or casting on a refractory model), with plastic (by molding method), with ceramics (by injection molding method);• modeling an inlay made of composite materials directly on a working model of a tooth stump made of supergypsum or ceramic masses on a refractory model; • computer milling of ceramic inlays.
To remove the inlay from the cavity, use a metal pin made of orthodontic wire with a diameter of 0.8-1.0 mm and a length of 1.5-2.0 cm, the heated end of which is carefully inserted into the wax. The position of the pin in the wax should correspond to the path of insertion and removal of the insert from the cavity in one direction. Large tabs are removed from the cavity using a U-shaped bent wire pin. If there are no signs of deformation, the wax model of the inlay is sent to a technical laboratory, and the cavity is closed with a temporary filling. The technique of making a cast metal inlay from a wax model obtained in the mouth was first described by Taggart in 1907. The direct method of making inlays has certain advantages and disadvantages. Advantages of the direct method: • higher accuracy of the resulting wax model of the inlay - there is no need to obtain an impression and a plaster model, for the production of which auxiliary materials with volumetric changes are used; • the ability to eliminate deficiencies in the preparation of the tooth cavity: if the inlay becomes deformed when removed from the cavity, during the same visit it is possible to identify and eliminate the deficiencies of the preparation with repeated modeling of the inlay; • the ability to control the boundaries of the inlay in the area of the gingival margin, which is important for the prevention of inflammatory changes in the mucous membrane; • the ability to model an inlay taking into account the articulatory relationships of the restored and antagonizing pairs of teeth. Disadvantages of the direct method: • difficulties associated with insufficient visibility of the surgical field in the area of the lateral group of teeth, increased salivation; • the possibility of thermal injury to the oral mucosa with a hot modeling tool when working with wax; To obtain a tab model, two traditional methods are used: direct and indirect. Direct method of making inlays In the direct method, the inlay is modeled directly in the patient's oral cavity, followed by replacing the wax with the main material of the inlay in a dental laboratory (Fig. 1-7).
Rice. 1-7. Scheme of clinical and laboratory stages of manufacturing inlays using the direct method
Modeling an inlay in the oral cavity is performed as follows. First, in order to control the quality of cavity formation, a stick of modeling wax, heated to a plastic state, is pressed into it. After hardening, the wax is removed from the cavity. If the cavity is formed correctly, then the wax is removed from the cavity and reintroduced into it without deforming the surface. If areas of deformation of the cavity imprint on the wax or difficulties in removing wax from the cavity are determined, then areas of retention are identified and they are ground off. After this, they proceed directly to modeling the tab. A stick of heated wax is again pressed into the formed cavity and its excess is cut off. While the wax remains flexible, the patient is asked to close the teeth in a position of central occlusion, and then simulate chewing movements. In this case, the surface of the inlay takes on a shape characteristic of functional occlusion. Subsequent modeling is aimed at restoring the anatomical shape of the destroyed part of the tooth crown (deepening fissures, forming cusp slopes, restoring the equator). Modeling of the chewing surface is carried out taking into account the age-related characteristics of the structure of the teeth.
• a large amount of time spent by a doctor on performing the technical procedure for modeling inlays with a large number of teeth being restored; • tediousness of the procedure for modeling inlays with a large number of teeth being restored for the patient. For these reasons, the range of indications for the use of the direct method of making inlays is limited to easily accessible cavities on the chewing or cervical surfaces. Indirect method of making inlays In modern orthopedic dentistry, inlays are often made by an indirect method, the use of which is indicated for all types of dental defects, including: • for defects of molar and premolar crowns of the MO, OD, MOD types; • defects in the contact surfaces of incisors and canines, both with and without damage to the cutting edge; • making inlays for adjacent teeth. Using this method, inlays can be made from all types of materials: metals, plastics, composites, cast ceramics, porcelain, combinations of materials. With the indirect method, the entire process of making an inlay - from the moment of creating the wax composition or the inlay itself - is carried out directly in the dental laboratory on a model (Fig. 1-8-1-10).
Rice. 1-8. Scheme of clinical and laboratory stages of manufacturing metal and plastic inlays by indirect (reverse) method
After the cavity is formed in the tooth, the doctor takes an impression using elastomeric impression compounds (silicone, polysulfide, polyester). The impression must convey all the details of the tissues of the prosthetic bed with the maximum degree of accuracy, which is achieved by obtaining a two-layer impression. Based on the impression received, the technician casts a working model. The working model of the dentition is usually made using a combined collapsible model. The collapsible model allows you to pre-fit the insert and control the tightness of its fit. Depending on the material used to make the inlay, the model of the prepared tooth can be made of supergypsum or duplicated from a refractory material.
Inlays from polymeric materials can be created without first making a wax model of the inlay. For this, light-curing polymers are used, which are sequentially introduced layer by layer (in layers up to 2 mm) into the cavity and polymerized layer by layer in special devices. Inlays are usually fixed using dual-curing composite materials or glass ionomer cements. Before fixing, the internal surfaces of the inlay must be specially prepared depending on the construction material used. Before fixing the composite tab, its internal surfaces are treated in a sandblasting machine. This promotes effective adhesion of the inlay surface to the fixing material by creating a larger contact area and micromechanical retention. Before fixing the ceramic inlays, the inner surface of the inlay is etched with hydrofluoric acid and silanized. The production of combined inlays involves the sequential creation of two parts of the structure - a metal frame and a polymer (compomer or ceramic) lining. When making a metal-plastic insert, a metal frame is first made, which is adjacent to the bottom and walls of the cavity. The frame is modeled on a collapsible wax model so that its thickness is 1.5-2.0 mm less than the thickness of the inlay. Retention balls with a diameter of up to 0.6 mm are applied to the outer surfaces of the wax frame, with the help of which conditions are created for the mechanical fastening of the polymer lining. Replacing the wax composition of the frame with a metal alloy is carried out according to generally accepted methods. After casting, the metal frame is fitted onto the collapsible combined model and into the oral cavity.
The manufacture of polymer cladding is carried out in one of the following ways: • modeling the cladding directly on the metal frame of the inlay with polymer; • modeling of wax lining with its subsequent replacement with polymer material;
• the impossibility of using methods to compensate for metal shrinkage during casting and to provide free space for the fixing material (coating the walls and bottom of the cavity on the model with an insulating varnish); • insufficient accuracy when modeling the approximal walls of the tooth in the area of the gingival papilla; • the need to re-model the inlay if its casting is unsuccessful; • the impossibility of preliminary fitting on the model, which increases the time of its correction in the oral cavity.
Rice. 1-9. Scheme of clinical and laboratory stages of manufacturing composite and ceramic inlays using an indirect (indirect) method
Rice. 1-10. Scheme of the clinical and laboratory stages of making a porcelain inlay
The technology of lining the metal frame of the inlay with a compomer or keromer is similar to the sequence of manufacturing a metal-plastic inlay with some features: • applying a binder layer to the metal frame of the inlay; • sequential layer-by-layer application of compomer material; • light curing in a special apparatus. To make a metal-ceramic inlay, the metal frame is cast from a cobalt-chrome alloy, and before applying the ceramic it is subjected to heat treatment - firing to create an oxide film for reliable adhesion to the ceramic coating. Method for computer milling of ceramic inlays In order to optimize and increase the efficiency of a doctor’s work, computer technologies for milling inlays from ceramic materials ( CEREC ) have been created. The use of this technology eliminates the use of dental technician labor and allows the manufacture and installation of ceramic inlays directly in the clinic during one patient visit.
Using this method, inlays are made from a standard ceramic block, so such microprostheses are characterized by higher strength indicators. The advantages of computer technology for making inlays include the elimination of the clinical stage of obtaining impressions and the technical stage of obtaining models, which saves time for the doctor, technician, and patient. In addition, the absence of the need to obtain impressions and models (materials for the manufacture of which differ in the variability of volumetric parameters) leads to an increase in the accuracy of manufacturing inlays. The formation of a cavity for an inlay is carried out according to generally accepted rules, with the peculiarities of preparation for ceramic structures. The cavity is formed with slightly diverging walls (no more than 4-6°). This is necessary to obtain an accurate “optical impression”, in which the inner and outer edges of the cavity are simultaneously visible in one projection. After this, an “optical impression” of the prosthetic tooth and adjacent teeth, as well as the occlusal surface of antagonist teeth, is obtained using an intraoral video camera. The image of the cavity, information about its size and shape, as well as the contours of the chewing surface of the antagonist teeth are transmitted to the monitor screen. Using a special program, the image is processed, and the dentist carries out computer modeling of the structure, taking into account approximal contacts, static and dynamic occlusion. Based on the virtual model of the inlay, the inlay is manufactured from a standard ceramic blank on a special milling and grinding machine with program control. The process of milling the inlay takes no more than 15 minutes, after which the inlay is fitted in the oral cavity. After appropriate preparation, the tab is fixed. Occlusal contacts are finally adjusted after its fixation.
You might be interested in:
- Manufacturing of temporary dentures using matrix technology
- Manufacturing of temporary dentures
- Methods for making veneers
- Preparation of teeth for veneers. Fixation of veneers
- Treatment with veneers
Related materials:
- Preparing cavities for an inlay
- Application of tabs (classification of tabs)
- Theoretical foundations of tooth preparation
- Types of dentures
- Examination methods for defects of hard dental tissues
Next >>
Materials for the manufacture of microprostheses
In prosthetics, various types of dental inlays made of different materials are used. It is important that the product is durable and can withstand intense chewing loads. Read more about common variants of such designs below.
Hardware
Most often these are products based on a chromium-cobalt alloy, but they can also be made of gold or with the addition of platinum and palladium. The option is quite durable, but if such a choice is made, aesthetics may suffer - over time, the gums will recede somewhat, and then a strip of a characteristic gray or yellowish tint will be visible. A good option for teeth that are invisible during conversation.
“Once one of my back teeth first cracked and then almost completely crumbled. The doctors said that the wrong bite was to blame, but I still have some doubts. I think it was simply poorly treated at the time, so it began to gradually deteriorate. In general, they restored it to me on a metal tab. They said it was too late for the pin. Either completely remove and install an implant, or a crown on an artificial stump. I chose the second option because it's cheaper. It’s been about a year now, and so far everything is fine, nothing bothers me.”
TolikSun88, from correspondence on the forum www.32top.ru
All-ceramic models
When people talk about ceramic structures, they usually mean zirconium (zirconium dioxide) products - they are quite strong and wear-resistant, but do not in any way affect the aesthetics of the smile. The dioxide is white and at the same time translucent - it most accurately matches the shade of natural enamel. Even if the gums recede a little over time, the zirconium base will not be noticeable. Products made from this material are much more expensive than their metal counterparts.
Metal-ceramic products
Metal-ceramic structures are used extremely rarely today. This is not the most reliable and durable prosthetic option. Such models often fall out, which is due to a mismatch between the degree of expansion of ceramics and metal. It is better to give preference to a metal-ceramic or zirconium crown, but the base for its fixation must be made of metal or zirconium.
Composite inlays
Composite models are used less and less. The material is not strong enough, often cracks under mechanical stress, and reacts poorly to sudden temperature changes in food and drinks. Sometimes they are used as temporary structures until a permanent orthopedic product is ready.
Care after prosthetics
Caring for your teeth after installing a core prosthesis differs little from normal oral hygiene. This should include brushing your teeth twice daily. In this case, it is better to use a brush with soft bristles.
After each eating session, it is advisable to rinse your mouth with warm water, herbal infusions (chamomile, sage) or special ready-made mouth rinses.
To clean the interdental spaces, use floss or a brush.
It is advisable to visit a dentist every six months.
When is this method contraindicated?
Prosthetics with this method are not performed in dentistry if the nerve is still alive. For such cases, traditional filling is recommended, which will help hide the aesthetic defect. Among other contraindications, experts identify the following conditions:
- the root is severely damaged and does not adhere well to the periodontium,
- the channels are not treated, inflammatory and purulent processes continue in them,
- the teeth are too loose, and it is no longer possible to fix them in one position, which means it is useless to install inlays,
- There is a pronounced recession of gingival and bone tissue around the affected element.
Don't know what type of prosthetics to choose?
We will help in the selection, advise where to read more information and compare types of prosthetics.
Consultation with an orthopedic doctor in Moscow clinics is free! Call now or request a call
Working hours: from 9:00 to 21:00 - seven days a week
You need to understand that the pin structure goes deep enough into the root. If the patient is intolerant to metals, an allergic reaction may occur. Therefore, it is better to take an allergy test in advance or choose an option made from a different material.
Artificial crown
An artificial crown is a type of fixed prosthesis made of metal alloys, porcelain, polymer, composite materials or combinations thereof, designed to cover the clinical crown of a natural tooth. They restore the anatomical shape of the tooth, the interalveolar height - the distance between the jaws and prevent further loss of hard tissue.
Artificial crowns
Indications for prosthetics with artificial crowns:
- Extensive dental defects of traumatic or carious origin when filling or prosthetics with inlays or veneers is impossible;
- Increased tooth wear, wedge-shaped defects;
- Anomalies in the shape and/or position of the teeth;
- Congenital disorders of the structure of hard tissues (hypoplasia and aplasia of enamel - less than normal amount or complete absence);
- Change in tooth color;
- Improving the fixation of removable dentures (creating a pronounced shape with expansion and contraction towards the neck for better connection with the retaining elements).
In addition, crowns are used as supporting elements of bridges, removable dentures, orthodontic and maxillofacial devices, and clasps for removable dentures.
Purpose of artificial crowns:
- Restorative – recreating the anatomical shape of the tooth, color and function;
- Support;
- Splinting – combined into groups and used to immobilize mobile teeth;
- Preventive – counter crowns on the teeth of the upper and lower jaws (antagonists) to prevent the progression of increased abrasion.
According to the technology, artificial crowns can be cast, stamped, obtained by firing or pressing ceramic mass, polymerization of plastics or composite materials, or milling.
In terms of material, they are all-metal (alloys of noble or base metals), porcelain, ceramic, polymer, composite, combined (metal-polymer, metal-ceramic, composite fiberglass). Typically, the crown material covers the stump on all sides (full crowns).
The choice of material and technology depends on the objectives of the individual clinical situation.
Their use requires preparation of teeth - preparation - creation of a stump shape that will ensure the possibility of application and fixation, as well as correct relationship with the gum edge and neighboring teeth. Retention occurs due to a layer of fixing cement.
The need to remove hard tissue is perhaps the only fatal drawback of this technology. Limitations in the use of crowns may be due to malocclusion pathology, increased tone of the masticatory muscles, the presence of dissimilar metals in the oral cavity, allergic reactions to materials, and young age.
Prosthetics on implants is in general similar to that on natural teeth (an implant is an artificial analogue of a root, onto which a crown is attached through an adapter - an abutment or directly). The only distinguishing feature will be screw fixation, which is impossible on natural teeth.
Advantages of artificial crowns:
- Increasing the physical and mechanical characteristics of the crown of a natural tooth due to the circular coverage of the dental stump with a single strength structure;
- The ability to reproduce or correct the appearance of the crown in the desired direction;
- The ability to perform the function of a supporting element of a fixed or removable prosthesis.
A generalized sequence of stages in the manufacture of artificial crowns (after the stages of examination, determination of indications, selection of type and preparatory measures) for natural teeth:
- Color determination;
- Obtaining impressions and diagnostic models (as needed - for example, in case of severe destruction of the crown and the need for preliminary modeling to obtain temporary crowns, tilting of the tooth);
- Preparation according to crown type and clinical situation;
- Obtaining final (working) prints;
- Fixation of temporary crowns;
- Obtaining working models;
- Wax crown modeling;
- Replacing wax with a permanent structural material;
- Model fitting, evaluation and correction;
- Oral fitting, assessment and correction;
- Temporary and permanent fixation.
Accordingly, when prosthetics on implants, when taking impressions, the position of the latter in the jaws will be recorded using transfers (impression modules).