When there is a lack of oxygen in the tissues, the skin turns blue. When a tight bandage is applied to any part of the body, such as a hand or foot, due to decreased blood flow, you may observe bluish skin. After exposure to the cold, you may see blue fingers and lips. Skin color will return after warming up. Often during feeding, newborns will develop a blue and white triangle around their mouth. After finishing feeding, it disappears. If there is blue discoloration in other areas of the skin, this may mean oxygen starvation.
URGENT CARE
Call an ambulance if:
- if the child has a fever, difficulty breathing and blue lips and tongue
- The child's whole body begins to turn blue
ATTENTION!
Call “emergency help” if the child cannot breathe, speak, or turns blue. At this time, begin first aid measures.
| ASK YOURSELF A QUESTION | POSSIBLE REASON | WHAT TO DO |
| The child is trembling, has been in water or cold for a long time | Hypothermia | Try to dress your baby according to the weather. If he is very cold, you can dry the child and take him to a warm room or let him take a warm bath. |
| The child has difficulty and noisy breathing, hoarseness, barking cough | Croup | Call the pediatrician |
| The child has difficulty exhaling, strained breathing, wheezing and wheezing can be heard. The skin around the mouth and lips turns blue | An attack of obstruction or asthma | Call "emergency" |
| The skin around the mouth and lips turn blue after a quarrel or outburst of anger | Holding your breath | Consult your pediatrician as planned ; he will recommend an examination to rule out organic causes of the disease and give advice on what to do if the attack recurs. |
| A child under one year old has been sick with a viral infection for a couple of days, breathing has become difficult and noisy, irritation is present, and appetite is reduced (does not eat at all). | Bronchitis, bronchiolitis | Call a pediatrician for an examination , “emergency care” . Once the diagnosis is confirmed, the issue of hospitalization may be decided. |
| The child suffered a viral infection. He has rapid breathing, wheezing, increased temperature, blue lips and nasolabial triangle, lethargy and poor health. | Pneumonia | Call the pediatrician ; if the diagnosis is confirmed, hospitalization is possible |
| A child's fingers, tongue, mucous membranes and lips turn blue after physical activity or during active play | Lung or heart disease | Avoid physical activity until the cause is determined. Make an appointment with your pediatrician , and after the examination, treatment will be prescribed. You may need to consult specialists. |
| The child has seizures and involuntary urination | Seizure | Call "emergency" |
FOR INFORMATION
What to do if you hold your breath?
When a child screams or cries, is close to hysteria, he cannot take another breath. His face may become pale or blue. There may be convulsions, and the child falls unconscious. This situation scares more parents than the baby. Parents try to get the child to take another breath. But even if the baby is very angry, he will not be able to hold his breath for a long time without harming himself.
After convulsions or loss of consciousness, breathing will restore itself. But be sure to consult a doctor after an episode of loss of consciousness or convulsions, to rule out a serious illness in your baby. You may need to consult a psychologist if your child has an emotional disorder. This condition does not threaten the child's health. Do not show your child your concern by holding your breath against an emotional background. Over time, he himself will find another way of emotional relief. Holding his breath can become a habit if he sees that he is achieving his goal in this way. Your task is not to show your concern. If after loss of consciousness the child does not begin to breathe immediately, then perform artificial respiration immediately. And call “emergency help.”
What can cause an attack?
Infections that cause fever. The infection can be caused by bacteria, but more often febrile attacks occur with viral diseases (for example, roseola and influenza).
Vaccinations that cause fever. There is a small chance of febrile seizures after vaccination against measles, rubella and mumps, and diphtheria, tetanus and whooping cough. But the risks from incomplete vaccination are higher than the risk from a febrile attack after vaccination.
Heredity. If either parent has had a febrile seizure, the child is more likely to have seizures with fever.
A febrile attack, especially one occurring for the first time in life, is very frightening for parents. In fact, most of these attacks are not dangerous and do not lead to complications or brain damage. A child with simple febrile seizures is only slightly more likely to develop epilepsy than children who have never had a febrile seizure.
Additional symptoms
Hyperthermia is sometimes accompanied by the following symptoms:
Marbled leather
A network of vessels. This is not a disease, but a vascular reaction to an irritant. It occurs more often in infants under six months of age. If the child is older and this phenomenon bothers him, he should consult a doctor.
Diarrhea and vomiting
Signal of intestinal disease. Vomiting also occurs during heat stroke; in this case, there is general dehydration in the body, and there may be blood in the stool.
Headache
More often it warns of ARVI, but tumor development processes are also possible. When the heat rises, blood flow increases, which increases the pressure inside the skull, causing headaches.
Acute respiratory infections or acute respiratory viral infections often cause hyperthermia and are dangerous for complications, especially in toddlers
Hot body but cool head
This is how the fever begins. The forehead is cold, but the body and part of the head are hot. In this state, a state of almost fainting may occur, sometimes accompanied by delusions and hallucinations. Don't hesitate, call an ambulance.
Reduced pressure
This often means that the body is infected with a virus. Blood pressure decreases due to decreased tone and the release of certain hormones. For five days, it is necessary to measure the child’s temperature three times a day, and the pressure twice. If after this time the condition does not improve, you should consult a doctor and undergo an examination.
How to help a child during an attack?
- Place your baby on his side on a flat surface and make sure he won't fall or hit anything during the cramp (such as crib bars).
- Record the time and tell the doctor when the attack began and how long it lasted.
Attention! Do not try to open the jaw, do not put anything into the child’s mouth during an attack, this can lead to injuries (broken teeth of the child and injured fingers of the person providing assistance). Do not try to restrict the child's movements during seizures, do not restrain him.
The child may be even more afraid of the attack than the parents. Try to calm him down and support him.
If the attack occurs for the first time in life, lasts longer than 5 minutes, the child is unusually sleepy and lethargic before or after the attack, call an ambulance.
In other cases, immediately show the child to the pediatrician. The doctor should examine the child after the attack to make sure there are no signs of a central nervous system infection (meningitis or encephalitis).
Additional recommendations
It is extremely important to combine antipyretics and antispasmodics under the supervision of a physician. You cannot decide on your own which drugs to combine. Only a pediatrician can say for sure.
What happens when the ambulance arrives
It is not necessary that the baby will be taken to the hospital. Doctors often give consultations over the phone. If the ambulance team does arrive, they can simply inject the necessary injections. If the condition is truly serious, hospitalization will be suggested. But only you can give final consent or write a refusal to be hospitalized.
The ambulance does not prescribe treatment
How to treat fever in a child who has previously had febrile seizures?
If the child does not have an increase in temperature during illness or after vaccination, it is not recommended to give antipyretic drugs! This does not reduce the risk of an attack.
If the temperature has risen, medications to reduce it make you feel better overall, but do not help with attacks.
The harm from anticonvulsants for the prevention of febrile seizures outweighs the benefits; they are almost never prescribed.
If a child’s febrile convulsions are prolonged, at the beginning of the attack it is recommended to administer a drug from the benzodiazepine group in the form of an enema, a spray in the nose or a gel on the cheek. Unfortunately, none of these forms are registered in Russia. Therefore, if an attack lasts longer than 5 minutes, an emergency doctor may give an injection of such a medicine.
For antipyretic drugs, children can be given ibuprofen at a dose of 10 mg/kg every 8 hours or paracetamol at a dose of 15 mg/kg every 6 hours. Don't give children aspirin!
Pneumonia
This is one of the leading causes of child mortality. Unfortunately, pneumonia is very often diagnosed too late, on the 6-7th day of illness, when irreversible complications occur.
The symptoms of the disease are similar to the symptoms of ARVI, so if the temperature is low, parents do not take any measures, but simply wait for the child to recover. Pneumonia can occur without coughing or wheezing in the lungs, so even a pediatrician can miss it at home.
Article on the topic
Dangerous for babies. How to avoid pneumonia? Remember: if the child is weak, pale, sweats a lot, complains of chest pain when breathing and coughing, first of all you need to rule out pneumonia.
Another reliable symptom of pneumonia, by which the disease can be recognized even at an early stage, is shortness of breath.
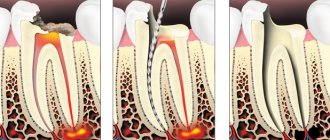
The “gold standard” for diagnosing pneumonia includes general and biochemical blood tests, urinalysis, and chest x-ray.
It is important to know
Parents often mistake normal chills associated with fever for febrile seizures. With such chills, the child's arms and legs may shake rhythmically. This is similar to a seizure, but the child is conscious and reacts if spoken to. So that the doctor can better determine whether what happened was a seizure, and if so, what kind, try to clearly record the duration of the seizure, describe it as specifically as possible, and ideally, record what is happening on video (one person helps the child, the other films it on the phone).
What to do if you have a chill
If you experience severe chills and the temperature exceeds 38 degrees, call an ambulance.
Forbidden:
- rub the body with alcohol or vinegar;
- wrap up;
- give aspirin;
- apply cold compresses to the entire body, only to the forehead. The towel should be cool.
Necessary:
- Create a temperature in the room no higher than 20 degrees.
- Rub your baby's legs and arms with your own hands.
- Give your baby plenty of fluids to drink.
- To relieve spasm, give the child No-Shpu, Drotaverine or use Papaverine suppositories. Next, give an antihistamine - Zyrtec, Suprastin, etc. They will enhance the effect of drugs that relieve spasms.
- When the limbs turn pink, blood circulation has been restored and the fever can be reduced. Use paracetamol-based medications.
- If the condition does not improve, take the child to the hospital.
The child rolls up when crying and his face turns blue, what should I do?
Ignoring problems can lead to epilepsy and occasional fainting. The situation is somewhat different with children of conscious age who have reached the 1 year mark. Often children turn blue while screaming because they want to achieve what is forbidden. In this way, the child seems to be blackmailing his parents.
The child rolls up when crying and his face turns blue, what to do:
- Such children often fall to the floor, jerk their legs and throw tantrums in the most inappropriate places. In most cases, the problem here is not neurology at all, but incorrect upbringing. Under no circumstances should such children be indulged. It has been noted that such children are very often prone to fainting already at conscious, school age. Therefore, it is necessary to correct their behavior in time.
- Such children need to be sent to preschool educational institutions, that is, to a nursery or kindergarten. Usually outside the family, attacks of screaming and blueness of the face practically do not recur. Children behave completely differently in the presence of strangers, more restrained, and rarely show aggression. In addition, it is necessary to raise such children correctly. It is necessary to talk with all household members and discuss the correct line of behavior.
- The whole family needs to be together, and no one approves of such hysterics. The simplest thing is to satisfy the child’s request, but in this case this is the most wrong way to resolve the conflict. In this way, it will be fixed in the child’s memory, and he will constantly manipulate his cry.
Face turns blue
What to do and who to contact?
A pediatric cardiologist or pediatric neurologist will help you understand the problem in detail. These specialists will determine whether there are pathological abnormalities in vascular activity or in the autonomic nervous system. If necessary, your pediatrician will prescribe a referral to specialists.
At home, while bathing, you can perform contrast baths for the limbs . They have a remarkable effect on vascular tone, improving and enhancing blood supply to the extremities. Gymnastics and hardening are also your helpers.
Children with low immunity are advised to take courses of vitamin therapy and restorative procedures. The pediatrician will tell you how to carry them out correctly. Self-indulgence in this matter is unacceptable.
The child starts crying and turns blue: Komarovsky
As soon as a child starts screaming in order to get what he wants, that is, to manipulate adults, it is necessary to explain to him in a calm tone that such an activity will not bring results.
The child starts crying and turns blue, Komarovsky:
- Dr. Komarovsky believes that it is necessary to explain to the child the consequences of such behavior. For example, if you don’t stop the hysterics now, I will send you my room and deprive you of games. It is necessary to tell the child that punishment will follow.
- Try to be disciplined, and be sure to carry out threats and punish the child if he disobeys. Thus, over time, the child develops the correct model of behavior, in society, in public and in the family.
- The less the child screams, the less likely such attacks will occur.
Newborn
“Gray” syndrome is a form of cyanosis in children in the first months of life associated with the use of chloramphenicol
“Gray” syndrome is a form of cyanosis in children in the first months of life associated with the use of chloramphenicol. In children, regardless of age (especially with glucose-6-phosphate dehydrogenase deficiency), sulfonamides in high doses can cause sulfhemoglobinemia, and for clinical signs of cyanosis to appear, a blood level of 5 g/l of sulfhemoglobin is sufficient. Ingestion of 100-300 mg of methylene blue per day restores the oxygen transport function of the blood in all forms of methemoglobinemia, while ascorbic acid in a dose of 100 to 500 mg is effective in congenital methemoglobinemia. Sulfhemoglobin is a strong compound, and methylene blue has no effect on the restoration of the oxygen-containing space of the blood.
The light blue coloration of the skin in argyria may resemble cyanosis, but abnormal skin pigmentation due to skin color can occur in Addison's disease or hemochromatosis.
There are total and regional cyanosis
There are total and regional cyanosis (perioral - around the mouth, cyanosis of the nasolabial triangle, cyanosis of the distal parts of the body (acrocyanosis) - the tip of the nose, earlobes, lips, tip of the tongue, hands, feet). More often, cyanosis is observed in diseases of the respiratory system and cardiovascular system. In lung diseases, cyanosis occurs as a result of blood passing through poorly ventilated areas of the lungs, while the amount of unsaturated hemoglobin increases as a result of a mismatch between ventilation and perfusion. In congenital heart defects, cyanosis is caused by intracardiac mixing of venous and arterial blood. Peripheral cyanosis can occur as a result of a decrease in peripheral blood flow; the amount of unsaturated hemoglobin in the capillary bed increases due to increased extraction of oxygen by tissues. Cyanosis in a healthy child can develop at high altitudes, where the partial pressure of oxygen in the inspired air is reduced.
The nasolabial triangle turns blue, the baby's face: reviews
Many parents tend to exaggerate, so they often run to the doctor when the first sneeze appears. Below you can read reviews from mothers who have experienced this pathology.
The nasolabial triangle turns blue, the baby's face, reviews:
Alina. My son is 2 years old, after birth I did not notice any blueness in his face, but he practically did not cry as a child. Upon reaching the age of two, he began to behave strangely. The child is very emotional and actively reacts to refusal. May throw tantrums. Very often, while crying during this period, there is a blue face, and even holding your breath. I was worried about this and went to a neurologist. We were prescribed Glycine and also told to follow a daily routine.
Veronica . My child is 6 months old, he was born very weak, with hypoxia. But after an ultrasound we were diagnosed with intracranial pressure. When crying, the nasolabial triangle often turns blue. The condition of the lungs and heart were checked and no pathologies were found. The neurologist prescribed us Cortexin and Neuroxon. After taking the medications, my condition improved significantly.
Olga . I gave birth to a premature baby, so my health is not all right. During screaming and crying, the face turns blue and arches. We are under the supervision of a neurologist. It is very difficult to watch such a child grow and develop. We are doing everything possible to get him back on his feet. We go for massages, bathe in soothing baths and do not exclude the use of medications. To calm me down, the doctor prescribed Pantogam and Glycine. We take medications as prescribed by the doctor.
Sleeps
Many interesting articles can be found on our website:
- A newborn baby sneezes: reasons, what to do. A child sneezes often: advice from pediatricians, reviews
- The child shudders in his sleep: reasons, what to do? Why does a child flinch when falling asleep due to sounds?
- Why does a child or infant curl his toes when walking? Why does a child curl his toes when walking, what should I do?
- Why does a child suck his thumb, is it harmful, what should parents do?
If blueness is observed only in a state of crying, there is no need to sound the alarm. When a child screams, blood circulation in the head worsens, and the capillaries become bluish. This is what provokes the blueness of the face in this area. If this happens constantly, and it doesn’t matter whether the child is at rest or emotionally overexcited, then it makes sense to consult a doctor.
The child starts up and turns blue
In a state of emotional overstrain, a child needs somewhere to put his energy and negativity. That is, if a child is very angry, aggressive, angry at someone, or reacts very emotionally to what is happening, then a blue face with stopping breathing can sometimes occur.
The child starts up and turns blue:
- Some children, when crying strongly or emotionally excited, may arch, scream, stop breathing and turn blue. In this case, infants need careful care and observation.
- Try to prevent such a child from overheating, feed him regularly, and try to create a favorable, calm atmosphere in the house. It is necessary that older children do not scream or make noise. The calmer the family, the better this affects the condition of the baby.
- Such children respond very well to discipline, with constant rituals. Try to feed your child and walk outside with him at the same time. It is necessary for the child to feel safe.
- Thus, the number of hysterics will be significantly reduced, which will minimize the possibility of such attacks, turning blue in the face and stopping breathing.
Face turns blue
Peripheral (cold, venous) cyanosis
Peripheral (cold, venous) cyanosis is a condition in which the blood in the arterioles of the cutaneous vascular plexuses has a normal oxygen content, warming the skin is accompanied by redness, and after pressing, a pink spot first appears, which later acquires a bluish tint. It is observed with a decrease in minute blood volume (heart failure, pericarditis, armored heart), local stasis in the final sections of the bloodstream (cooling, collapse and shock of various origins, arterial embolism, polycythemia, etc.).
In case of carbon monoxide poisoning (carbon monoxide, CO), carbon monoxide, entering the blood, combines with the iron of hemoglobin, converting it into carboxyhemoglobin, whose concentration in the blood is more than 35 g/l, hemic hypoxia, respiratory failure and neurological disorders occur (children's neurologist - polyclinic "Markushka"). Typically, patients have a bright red (cherry-red) face, acrocyanosis, and in a later stage severe cyanosis develops.