Many of our patients (as well as patients, for example, of chiropractors or neurologists) do not even realize how interconnected the problems they are being treated with are. For example, the jaw joint hurts, the head hurts, shooting in the ear, clicking in the jaw, pulling at the base of the skull... it would seem that these are different symptoms, but the reason may be the same for everyone: TMJ dysfunction
.
Functions of the TMJ
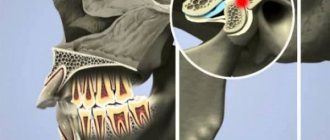
TMJ
or
temporomandibular joint
is a joint located above the ear that connects the temporal bone to the lower jaw and the lower jaw to the skull. The muscles that are attached to this joint are actively involved in speaking, facial expressions, chewing, and swallowing. Together, muscles, ligaments, cartilage and joints make up the apparatus, thanks to which we can generally open and close our mouth, move our jaw back and forth and left and right, and the load on this apparatus is significant - comparable to the load, for example, on the knee joint.
The temporomandibular joint is the only paired and symmetrically moving joint in the human body, and problems with its functioning lead to numerous unpleasant diseases. TMJ dysfunction—limited work and mobility of the jaw joint—occurs when the joint on the right and left sides of the skull does not move synchronously or evenly. For example, to open the mouth, the patient must first move the lower jaw from side to side, “until it clicks.” Or when you open your mouth, you feel pain in your jaw or temples.
This disease has many names: arthritis (arthrosis) of the TMJ, myofacial syndrome, myoarthropathy of the TMJ, chronic dislocation of the lower jaw, Costen's syndrome (named after the American doctor who first identified this disease). This pathology is difficult to diagnose and treat, and at the same time it can cause a wide variety of pain - from headaches to neck pain.
Statistical fact: from 30% to 70% of dental patients suffer from functional pathology of the temporomandibular joint. And these are not always older people, as one might expect. On the contrary, people of all ages, including children, suffer from TMJ pain and related pain.
TMJ dysfunction was first described by otolaryngologist (ENT doctor) Kosten in 1934. Kosten studied pain and noise in the ears and burning in the nose, which intensified during or after eating, and was the first to think of linking them with malfunction of the temporomandibular joint. Subsequently, his colleagues and other doctors who examined this problem expanded and supplemented the list of symptoms. Now this list is quite extensive, and often not all symptoms can be associated specifically with TMJ problems.
Diagnostics
Pain when opening the mouth requires, first of all, diagnosis; only an experienced doctor can make a correct diagnosis. There may be several reasons for this pathology, and the doctor’s task is to correctly diagnose the disease, since the treatment method will depend on this. During the consultation, the doctor examines the patient and finds out, the patient’s posture is also assessed, and how difficult the functions of swallowing, chewing and breathing are.
During the examination, the doctor will also pay attention to the location of the pain, whether it manifests itself on one side or is bilateral. Based on the results, an additional examination will be prescribed: x-rays, manual functional analysis and other procedures.
An individual and comprehensive approach is the priority of the Orto-Artel clinic. Therefore, to establish the root cause of the problem and its further solution, consultations with specialists such as:
- osteopath;
- neurologist;
- kinesiologist;
- psychologist.
The joint efforts of dentists and general specialists will make it possible to make the correct diagnosis.
If your jaw hurts when chewing or opening your mouth, then in most cases, the pain is a sign of inflammation. Therefore, often, when ear pain or tinnitus is detected, it is associated with purely “ear” problems. And with pain localized in the area of the temporomandibular joint, doctors who do not have adequate experience in diagnosing and treating TMJ dysfunctions usually make a standard diagnosis - “arthritis of the temporomandibular joint.”
The diagnosis of arthritis in medicine means inflammation of the joint, but this formulation does not include information about the specific causes of such inflammation. Therefore, making such a diagnosis is a very general formulation. It's a very general diagnosis. Non-binding. Does not reflect the root cause of inflammation. In fact, it is only a statement of the fact of inflammation in the joint.
But the causes of this inflammation can be very different, and accordingly, treatment, depending on the causes of inflammation, will differ significantly in different patients, even those who have common symptoms - pain in the jaw joint when opening the mouth. Or ear pain. Inflammation is the body's normal response to injury. And injury can be caused by various factors.
Diagnostics is the first and key step in treating pain in the jaw when opening the mouth. Do you want to know why it’s impossible to do without diagnostics?
In the case of joints, most often the injury will be mechanical. It occurs when the bones that form a given joint (in particular the head of the mandibular condyle) exceed their normal range of mobility. And they overstretch the joint capsule, ligaments and muscles associated with this joint. Every person has encountered this at least once in their life. Because this process has a well-known name - joint dislocation.
The dislocation may be acute. This is when it happens sharply and suddenly. In the case of the temporomandibular joint - with sudden opening of the mouth (for example, when yawning). Or due to a blow to the lower jaw area.
The dislocation can be chronic. This is when the bones that form a joint regularly (constantly, for a long time) exceed the amount of their normal mobility. In the case of TMJ, this happens when the bite is incorrect. Then each closure of the teeth will direct the lower jaw into the “wrong” position. And it is chronic injury that is more dangerous. Because, unlike an acute injury, a gradual stretching of the capsule and ligaments of the joint occurs, which camouflages (hides) the painful manifestations of the problem. After all, pain will occur in the later stages, when the process has already gone quite far, which often leads to untimely (belated) seeking medical help. Chronic injury is the cause of 90% of all TMJ problems. And it refers to functional problems (dysfunctions). When the daily, seemingly normal functioning of this joint leads to its gradual wear and tear and, ultimately, destruction.
The generally accepted traditional allopathic approach to the treatment of TMJ pathology with a banal (simplified) diagnosis of arthritis, and the resulting treatment (all this anti-inflammatory therapy, using pills, physiotherapy and other “traditional” methods) is erroneous and ineffective, since it does not eliminate the root cause of the problem .
Treatment in installments
The Orto-Artel clinic offers installments for the entire process of treating any disease. Personal conditions are considered on an individual basis.
Find out more
or call 8 (495) 128-11-74
In addition, I would like to note that pain in the jaw when opening the mouth is not always associated with problems in the TMJ (just as pain in the ear or tinnitus is not always associated directly with “ear” problems). Therefore, to differentiate the cause of the problem, to determine the true source of pain, consultation and assistance from a qualified specialist who understands these subtleties is necessary.
Symptoms of TMJ dysfunction
- Pain in the jaw, increasing when opening the mouth, chewing, speaking, yawning;
Clicking in the joint of the lower jaw, the jaw “jams”, it does not open, does not close, or has begun to close differently;- Pain in the temples, in the eye area, visual impairment, photophobia (sensitivity to light);
- Pain, ringing and noise in the ears, in the ear area, feeling of pressure in the ears;
- Frequent headaches, dizziness, migraines;
- Sleep disorders, insomnia, anxiety, depression;
- Pain in the neck, in the lower part of the skull;
- Tooth pain from sweets, hot, cold.
This diversity in symptoms, which often makes it difficult for doctors to diagnose, is explained by the fact that the joint is connected to many important organs and parts of the body (eyes, ears, neck, head) and errors in its functioning can affect everything at once, or they can only affect something one. It is usually possible to determine that the problem is in the temporomandibular joint only in a complex manner.
In most cases, TMJ dysfunction is manifested by pain in the face, joints of the jaw, neck, shoulders, ears, crunching and clicking. Complaints of dizziness, difficulty chewing food, speech and hearing disorders, difficulty opening the mouth, “jamming” of the jaw, or even the appearance of swelling and fever are also common.
What else do you need to know?
As mentioned above, it is impossible to independently identify the cause of unpleasant sensations when opening your mouth. Even when the patient consults a doctor, additional examination is required. The specialist usually prescribes an X-ray of the jaw, computed tomography, and MRI. Do not forget that each specific ailment requires a special approach to treatment. The general condition of the patient, the nature of the disease, and its stage are taken into account. Usually the pathology disappears when the cause that provoked it is eliminated. So:
- Injuries. A fixing bandage is applied and analgesics are prescribed. Cold compresses are recommended for patients; they will help relieve swelling and pain.
- Dental diseases are quite common. Caries, cysts, and other ailments require immediate treatment. After eliminating the problems, the pain usually goes away. Patients are also prescribed antibiotics.
- Neuralgia. This category includes a number of dangerous ailments. For their treatment, vitamins, antiviral drugs, and special physical training are recommended (exercises will help strengthen the jaw and relieve discomfort when it opens).
- ENT diseases. With otitis media, sinusitis and other ailments, patients often complain of pain that occurs when opening the mouth. For treatment, antipyretics, antibiotics, physiotherapeutic procedures, and drugs to strengthen the immune system are prescribed.
Pain in the jaw joint: causes
- Defects in the dentition - lack of teeth, overestimation of fillings;
Pathological abrasion of teeth;- Broken bite
;
- Overload of the masticatory muscles (for example, if you chew on only one side for a long time);
- Inaccurate prosthetics, errors in orthodontic treatment;
- Other anomalies of the oral cavity and jaw structure;
- Bruxism, involuntary grinding of teeth.
- Birth trauma, trauma to the skull and jaw;
- Osteochondrosis and scoliosis of the spine;
- Severe constant stress
;
- An infection in the joint cavity that provokes inflammation of the TMJ.
Treatment
Conservative therapy
Therapeutic tactics are determined by the cause of the symptom. For patients with dental pathologies, local treatment is indicated. Removable dentures and orthopedic structures are replaced, and other types of prosthetics are selected. In case of pulpitis, the cavity is treated with antiseptics, antibiotics, proteolytic enzymes, pastes are applied to eliminate inflammation and stimulate regeneration, and after a few days a filling is performed. For other diseases, the following methods are recommended:
- Inflammatory processes
. Antibiotic therapy is carried out in the pre- and postoperative period. At the initial stage, broad-spectrum drugs are administered parenterally. After receiving culture results, the medication is changed taking into account antibiotic sensitivity. Dressings are performed and rinsing is performed. Analgesics are prescribed to reduce pain. - Traumatic injuries
. In case of fractures of the angle, the body of the lower jaw without displacement, conservative immobilization is carried out by double-jaw wire splinting. To prevent inflammation, antibacterial agents are used, and painkillers are used to reduce pain. - Neuralgia
. Anticonvulsants are used to eliminate pain attacks. To enhance the effect, the treatment program is supplemented with antispasmodics, antihistamines, and microcirculation correctors. Trigger point blockade is carried out with a mixture of glucocorticoids and local anesthetics. They give a referral for ultraphonophoresis and galvanization with novocaine. - Muscle pathologies
. For bruxism, an integrated approach is effective, including medication, dental, physiotherapeutic, psychotherapeutic methods, and the use of protective mouthguards. Patients with myofascial syndrome are prescribed muscle relaxants, NSAIDs, and antidepressants. - IHD
. As part of drug therapy, antianginal agents, beta-blockers, calcium channel blockers, antioxidants, antiplatelet agents, and antisclerotic drugs are indicated.
Surgery
The choice of surgical technique depends on the cause of the symptom:
- Inflammatory diseases
: opening, drainage of abscesses and phlegmons, sequestrectomy for osteomyelitis. - Injuries
: open osteosynthesis using bone sutures, polyamide thread, mini-plates. - Neoplasms
: curettage, excision of benign neoplasia within healthy tissue (often with extraction of teeth), resection or disarticulation of the lower jaw for a malignant tumor. - Neuralgia
: microsurgical decompression, percutaneous radiofrequency destruction, stereotactic radiosurgery. - IHD
: thrombolysis, emergency coronary angioplasty in the acute period of a heart attack; planned coronary artery bypass surgery, balloon angioplasty for angina pectoris, post-infarction conditions.
Diagnostics and x-ray of the temporomandibular joint
Diagnosis of TMJ when it is dysfunctional is difficult due to the variety of clinical complaints. This leads to the fact that the patient can undergo examination by different specialists for a long time, wasting time. A full examination is carried out by dentists
(primarily an orthopedist or orthodontist) and neurologists.
Diagnosis with the naked eye is difficult, and TMJ problems can only be directly noticed if the malocclusion is clearly visible. Most often, dysfunction of the temporomandibular joint is associated precisely with disorders of bite and jaw closure.
The most reliable and effective way is to conduct x-ray diagnostics and orthopantomogram
jaws. In some cases, an MRI may also be done.
Treatment tactics
If there is no arthrosis, but there is dysfunction, the tactics are as follows:
- determine the root cause and eliminate it, for example, grind teeth and fillings that impede the functioning of the joint, correct prosthetic errors, and correct the bite;
- reduce the load on the joint - the patient is recommended to switch to soft foods, massage the facial muscles and exercises to relax the jaws;
- if the defects are serious, surgical treatment is performed - bone or muscle plastic surgery of the area of dysfunction.
If the doctor determines degenerative changes in the cartilage tissue, treatment for osteoarthritis will be prescribed. With the help of painkillers, they relieve pain. If necessary, a complex of physical therapy is prescribed, for example, laser or ultrasound. Good results are achieved by intra-articular injections of the Noltrex synovial fluid prosthesis, which restore the functionality of the joint by replenishing the missing lubrication.
Arthrosis of the TMJ is successfully treated with intra-articular injections of Noltrex
Treatment of the temporomandibular joint
Complex treatment of TMJ is possible only in dentistry, and is possible thanks to:
- surgery on the lower jaw;
- orthodontic treatment
(prescribing special trainers that will be worn at night and reduce pain by adjusting the load on the joint - the same trainers are recommended for bruxism) and bite correction with braces;
- orthopedic treatment
and
implantation
(insert a suitable prosthesis to restore the correct closure of the jaws).
Treatment is always prescribed individually, based on the results of an examination by an orthodontist, and is most often carried out comprehensively. It is dangerous to neglect TMJ diseases: this can lead to arthrosis, in which connective tissue grows in the joint cavity, which, in turn, threatens complete immobilization of the joint (ankylosis).
Severe pain and joint spasms can be relieved with compresses and painkillers; Stresses that provoke tension in the joint can be relieved with sedatives, but all these are half measures that do not treat the root cause of the pain.
Self-help methods for diseases of the temporomandibular joint:
The following self-help methods may provide temporary pain relief:
- Moist Heat: Compressing with a hot pack or bottle wrapped in a warm, damp towel can improve chewing function and reduce pain. Be careful to avoid burns when using high temperature.
- Ice: Ice packs can reduce inflammation, numb pain, and promote healing. Do not place the ice pack directly on your skin. When using, wrap the bag with a clean cloth. Do not use the ice pack for more than 10-15 minutes.
- Diet - Soft Foods: Soft or mixed foods allow the jaw to rest temporarily. Remember to avoid hard, crunchy, and chewy* foods. Do not stretch your mouth when trying to bite off large pieces or the whole fruit.
- Over-the-counter analgesics: Over-the-counter (over-the-counter) analgesics are useful for temporarily reducing pain. Together with your doctor, carefully read the instructions for each medication before using it.
- Lower jaw exercises: Slow, gentle exercises of the lower jaw can help increase jaw mobility. Your doctor or physical therapist can evaluate your condition and suggest appropriate exercises based on your individual needs.
- Relaxation techniques (relaxation techniques): Relaxation can help combat the pain that accompanies TMJ dysfunction. Deep, slow breathing increases relaxation and reduces pain sensitivity.
If you find an error, please select a piece of text and hold LEFT Ctrl and press Enter.
You can send no more than 5 messages in 30 minutes!
Liked? Tell your friends!
Why does wisdom tooth hurt?
Wisdom teeth almost always grow crooked. Problems with teething are dictated by the following anatomical features:
- “Eights” appear later than all other teeth. As a rule, the jaw bones are fully formed, the dentition is stable, and the “newbie” simply does not have enough space;
- The third molars do not have milk “predecessors”, and the rudiments of wisdom teeth developed for too long and not in very favorable conditions. Because of this, they erupt chaotically, damaging the adjacent tooth or causing inflammation of the gums.
When talking about the causes of pain associated with one or more molars, it is worth distinguishing between some concepts. Toothache can occur against the background of abnormal eruption, due to deformations of soft tissues of neighboring teeth. This clinical picture is typical only for “eights”; other teeth are cut much more smoothly.
Causes
However, the cause of toothache may also lie in fairly classic causes associated with common dental pathologies: caries, periodontal disease or periodontitis. If you systematize all the reasons that cause tooth pain, you will get the following list:
- The wisdom tooth rests too much on the tissues of the oral cavity, squeezing and injuring them;
- The tooth is rotated around its axis. The greater the angle of rotation, the more tense the dental nerve is, which provokes pain;
- Carious cavities have formed on the surface of the wisdom teeth; if they reach the dental tissues, the pain will intensify;
- Tartar deposits have formed, which rub the gums and cause inflammation;
- Due to the fact that the rapid growth of the “eight” and crooked eruption damaged the root system of the neighboring molar, it is this neighboring tooth that hurts;
- If the wisdom tooth, due to its incorrect position, begins to pinch the jaw nerve, pain occurs in the lower jaw. In this case, neuritis manifests itself in this way;
- A follicular cyst has formed at the neck of the tooth. It often occurs against the background of permanent damage to the gum tissue and the tooth itself.
It is worth noting the fact that a follicular cyst near wisdom teeth is often accompanied by all sorts of complications. For example, an abscess may occur that can even deform the jaw in a neglected state. The periodontal tissues may also become inflamed and pericoronitis may develop.
Inflammatory processes of the tissue covering the wisdom tooth
Inflammation of the hood is a common phenomenon. If a wisdom tooth erupts through several crown cusps at once, phenomena may occur when the chewing surface of the crown is partially covered by tissue. The part of the gum and mucous membrane that overhangs the molar and is called the hood. He is constantly susceptible to injury and prone to inflammation.
Under the surface of the hood, particularly favorable conditions arise for the accumulation of various biological “garbage” and the proliferation of pathogenic bacteria. Often even the slightest damage causes irritation. The gums around the “eight” may not hurt much, so they don’t always turn to people with such a problem.
However, if the inflammatory process is severe, the tissues not only swell, but are also irritated. The patient complains of painful swallowing, sometimes it is difficult even to simply open his mouth. There may be pus and severe hyperemia on the gum near the wisdom tooth. Only a doctor can save you from such an obsessive and severe dental inflammation by excision of the hood.
Lack of space during teething
If there is not enough space for the wisdom tooth in the dentition, neighboring tissues are injured during eruption. The pain is total. It hurts not only the place where the molar erupts, but also the neighboring teeth. Swelling, hyperemia, and severe pain that are permanent may also be observed. It is difficult for the patient to open his mouth, especially if the “eights” grow in the direction opposite to the jaw. Such teeth must be removed. This is due to the fact that a crooked tooth can damage the entire dentition, up to its noticeable curvature.
Caries
If a wisdom tooth is affected by caries, the first symptom indicating the disease will be pathological increased sensitivity of the teeth. They will react painfully to any irritants - sour, spicy, salty foods, sweets, cold irritants.
Situations often occur when the curvature of a wisdom tooth injures the neighboring tooth, which causes caries in it. The most dangerous situation is when the “eight” damages the root of the neighboring “seven”. Caries develops just below the gum, and the doctor is not always able to visually identify the carious lesion. At the same time, a severely advanced form of “root” caries is difficult to treat and the tooth can almost never be saved.
Pulpitis
In acute pulpitis that affects the wisdom tooth, patients complain of acute pain that occurs in attacks. The disease and its main manifestations are characterized by a spontaneous nature. Unpleasant sensations can occur spontaneously and last up to 15 - 30 minutes. At night the pain intensifies.
In the chronic form of wisdom tooth pulpitis, the pain is not so pronounced. Unpleasant, aching sensations occur against the background of exposure to cold or heat. If the irritant is removed, the pain continues for some time.
Periodontitis
Periodontitis is characterized by aching pain that constantly worries the patient. At the same time, the diseased tooth will react to any irritant with acute pulsating, shooting pain. Slight mobility of the affected tooth is also noted, and swelling and soreness of the gums are often observed.
It is interesting that with chronic periodontitis the pain is almost not disturbing. Very minor unpleasant sensations can only appear when the “figure eight” is tapped on the patient’s tissues.