Have questions?
Viral stomatitis is an inflammation of the soft tissues of the oral cavity caused by a virus.
The disease itself is a reaction of the human body to certain factors. So, most often the cause of the disease is infection with chickenpox, herpes, measles, and influenza.
Typically, infectious stomatitis is manifested by damage to the corners of the lips and mucous membrane of the mouth. Such symptoms are characteristic of the herpes virus and are most often found in children under three years of age. If a person’s immunity is strong and can resist the virus, the disease passes without a trace. In weakened patients, the disease can develop into a chronic form.
Causes of viral stomatitis
The occurrence of the disease is caused by a complication of the primary disease (chickenpox, herpes, etc.). The following may cause signs of the disease:
- poor oral hygiene;
- untreated caries;
- gingivitis, periodontal disease;
- unbalanced diet;
- avitaminosis;
- general weakening of the body;
- long-term antibiotic therapy.
Inflammation in other organs and systems of the body also causes viral stomatitis in children and adults.
Ways of transmission of stomatitis
Let's summarize. Viral, bacterial and herpetic forms of stomatitis are contagious. Knowing how the disease is transmitted, you can protect yourself and your loved ones. Ways of transmission of infection:
- airborne - sneezing, coughing;
- household items - common dishes, linen, personal items;
- toys, raw pacifiers, rattles;
- dirty hands;
- unwashed food;
- biological fluids - through saliva, blood, breast milk;
- Pets can carry the virus.
It is possible to catch the infection anywhere – from the street to your own home. You can get infected from both a child and an adult.
Features of the clinical picture
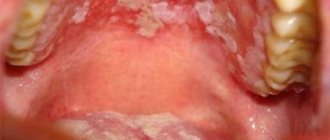
The symptoms of viral stomatitis at the initial stage of its development are easily confused with the symptoms of a common cold. The patient's body temperature rises and a headache appears. Gradually, the oral mucosa becomes very swollen and red, making it difficult for the patient to chew and swallow.
A few days after the onset of the inflammatory process, rashes characteristic of the disease appear:
- ulcers on the inside of the cheeks, palate, gums and tongue;
- groups of bubbles with clear liquid inside;
- “cold” on the lips, on the mucous membranes of the cheeks and in the nose;
- erosions that itch and hurt.
A whitish coating appears in the mouth of a sick person. The patient is concerned about general malaise, lack of appetite, bad breath and swollen lymph nodes.
Stomatitis
Cold
HIV
Fungus
Scarlet fever
Gastritis
12142 24 September
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Stomatitis: causes, symptoms, diagnosis and treatment methods.
Definition
Stomatitis is a collective name for diseases of the oral mucosa, manifested by its redness, swelling with the formation of areas of erosion, ulcers or blistering rashes. Stomatitis affects approximately 20% of the population, most often children. Stomatitis can be either an independent disease or a complication or manifestation of other diseases (for example, scarlet fever, influenza, measles, etc.).
Causes of stomatitis
There is no single factor that is the sole cause of oral inflammation. With stomatitis, bacteria or viruses are detected, especially in ulcers on the mucous membrane. However, a diverse microflora is always present in the oral cavity, but stomatitis makes itself felt only when there is a strong additional impact on this microflora.
These impacts include:
- trauma to the mucous membrane caused by overzealous brushing of teeth, rough food, etc.;
- decreased immunity due to colds, vitamin deficiencies, chronic diseases, stress, poor nutrition, as well as more serious diseases (anemia, cancer and autoimmune diseases, HIV);
- entry of a large number of pathogenic microorganisms into the oral cavity through dirty hands, unwashed foods, etc.;
- conditions for the proliferation of pathogenic microflora due to the presence of caries, tartar and plaque, lack of proper teeth cleaning, etc.;
- uncontrolled use of drugs that affect the quantity and quality of saliva and reduce its antimicrobial potential;
- inhibition of normal microflora by antibiotics;
- dehydration of the body with a decrease in the amount of saliva;
- diseases of the gastrointestinal tract (gastritis, pancreatitis, etc.).
Classification of the disease
Due to its occurrence:
- traumatic stomatitis
occurs as a result of the influence of physical (wound, burn from hot food, etc.) or chemical (burn of the oral mucosa with caustic substances, etc.) factors on the mucous membrane; - infectious stomatitis
occurs as a result of a viral, bacterial or fungal infection; - specific stomatitis
occurs as a result of a specific infection (tuberculosis, syphilis); this group includes radiation, drug, and stomatitis due to occupational diseases; - symptomatic stomatitis
develops against the background of diseases of the gastrointestinal tract, cardiovascular, nervous, endocrine systems, and blood diseases; - allergic stomatitis
develops upon contact with allergens.
According to the clinical picture:
- catarrhal stomatitis;
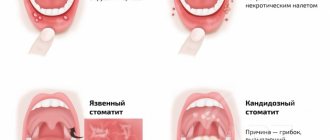
- ulcerative stomatitis;
- aphthous stomatitis.
With the flow:
- spicy;
- chronic.
There are stomatitis associated with dental problems - for example, denture stomatitis occurs due to damage to the mucous membrane by dental structures, due to poor care of removable dentures, and the patient’s failure to comply with oral hygiene.
Symptoms of stomatitis
In children, the disease is more severe than in adults: body temperature may rise significantly and intoxication may be present.
In adults, oral stomatitis, as a rule, is not accompanied by fever, except in cases of deep damage to the mucous membranes in the ulcerative form of the disease.
The most common is catarrhal stomatitis, which is characterized by inflammation of the oral mucosa without the formation of deep defects (ulcers). For those around you, catarrhal stomatitis manifests itself as “stale breath”, for the patient himself – pain, swelling and redness of the mucous membrane. Gingival papillae are easily injured and bleed.
In persons with pathologies of the gastrointestinal tract, as well as with inadequate treatment, catarrhal stomatitis tends to progress to the next stage - ulcerative with the formation of defects throughout the entire depth of the mucous membrane. It is accompanied by an unpleasant odor from the mouth, even putrefactive, the ulcers are covered with a gray coating, and eating any food leads to increased pain. Ulcerative stomatitis is more severe than catarrhal stomatitis and can cause a slight increase in temperature and enlargement of regional lymph nodes.
Aphthous stomatitis manifests itself in the form of small (3-5 mm) single or multiple defects of the mucous membrane of an oval or round shape, surrounded by a thin bright red border and covered with a yellow-gray fibrin coating. Aphthae do not form simultaneously, so you can see different stages of their development. Healing of aphthae begins after the fibrin plaque peels off on its own and ends with the complete disappearance of the defect.
Allergic stomatitis in the mouth occurs against the background of an exacerbation of the underlying disease - allergies. Increased sensitivity of the body can occur to food, medications, pollen, animal hair, cosmetics and care products, and even clothing. Most often, stomatitis is provoked by toothpastes that contain flavorings and chemical components.
Among viral stomatitis, the most common is herpetic stomatitis, which worsens against the background of ARVI. The disease begins with general malaise and lasts 7-10 days.
The oral mucosa becomes red and swollen, and regional lymph nodes become enlarged. After a few days, a blistering rash appears on the tongue and inner surface of the cheeks, and inside the rash there is a translucent liquid. After the bubbles open, small erosions appear, which are covered with a yellowish film.
Diagnosis of the disease
Adequate treatment of stomatitis can be prescribed by determining what caused it - bacteria, fungi or viruses.
If a fungal infection is suspected and to assess the effectiveness of therapy,
Candida albicans
in an oropharyngeal scraping and culture is performed for yeast-like fungi of the genus
Candida
and
Cryptococcus to determine sensitivity to antifungal drugs.
How is viral stomatitis treated?
Often, treatment of viral stomatitis is based on local exposure to damaged areas of the mucous membrane and skin. Ulcers and erosions are treated with an antiseptic and painkillers, the dentist prescribes applications (application of the drug) with anti-inflammatory and wound-healing compounds. To strengthen the immune system, the patient is prescribed medications based on echinacea and vitamins.
It is also important to follow a diet during therapy. All products consumed must be neutral in taste, pureed, and not hot.
You cannot self-medicate: without the help of a doctor, the disease can develop into a chronic form.
It is advisable to reduce home treatment of viral stomatitis in adults and children only to procedures that will speed up the healing process of lesions. The doctor will recommend rinsing with decoctions of herbs and oak bark.
What is stomatitis
Stomatitis (mucositis) is a disease that is accompanied by damage to soft tissues in the oral cavity.
It can be either an independent disease or a complication of various pathological processes, for example, measles, influenza, scarlet fever, etc. Until recently, stomatitis was considered a childhood disease. Today it is becoming more common in adults too. This trend raises questions about whether stomatitis is transmitted and, if so, how to protect yourself and your child. It all depends on the form of manifestation of the disease
What happens if stomatitis is not treated?
To avoid the question “To treat or not to treat?”, you should remember two facts about inflammatory processes:
- Neglected inflammation eventually progresses to the chronic stage. This means that problems with the mucous membrane will continue in the future. Chronic inflammation not only causes constant discomfort, but can also develop into a more serious problem.
- Inflammation of one area of the mucous membrane can spread to others. Thus, inflammation of the gums and inner surface of the lips can spread to the respiratory tract and further.
Here are some of the possible complications:
- chronic stomatitis,
- respiratory diseases (for example, laryngitis),
- periodontitis,
- loosening of teeth (after periodontitis),
- scars on the mucous membrane after healing of numerous ulcers,
- gastrointestinal diseases
- vision problems (with a herpetic infection, inflammation can rise there too).
Prevention
It is not possible to completely prevent the development of this infection in a child. Most people are already infected with viruses at birth, but it is quite possible to reduce the incidence of the disease.
To do this, the following measures are used:
- if one of the adults is infected, they should not be allowed to contact the child;
- choose a group in kindergarten with a small number of children;
- If possible, do not attend mass events during epidemics;
- it is necessary to harden the child (walk barefoot at home, go to the pool);
- stop bad habits (sucking fingers, toys, other objects);
- thoroughly wash and treat the child’s toys and dishes;
- treatment of all surfaces in the apartment using antiseptics.
Infectious stomatitis in children is a rather unpleasant disease. If you follow all the doctor’s recommendations and preventive measures, you can minimize the occurrence of this disease in your baby.
Aphthous stomatitis
This form of the disease is characterized by the appearance of single ulcers (ulcers) on the inflamed mucosa. Typical localization of erosions: mucous membranes of the cheeks, lips, palate, tonsils and surface of the tongue. Less commonly, aphthae form along the edges of the lips or on the gums. The general condition of a child with aphthous stomatitis rarely worsens, but the temperature may rise slightly and the submandibular lymph nodes may enlarge. The diameter of the ulcers usually does not exceed 10 mm.
It is generally accepted that the following factors can provoke aphthous stomatitis:
- An allergic reaction to certain foods, as well as components of toothpastes, in particular sodium lauryl sulfate.
- Systematic injury to the buccal mucosa, tongue biting.
- Exposure to nitrates in food and drinking water.
- Some chronic diseases, pathologies of the immune system, blood and gastrointestinal diseases.
How to avoid getting stomatitis again
To avoid getting stomatitis again, you need to follow 3 rules:
- Maintain hygiene.
- Treat teeth, check and change orthopedic structures in a timely manner.
- Monitor your general health.
The first rule for preventing recurrent stomatitis is hygiene. It is best to have your teeth professionally cleaned by a dental hygienist after the symptoms of the disease have disappeared. A specialist will use ultrasonic equipment to remove tartar and old plaque and advise on further dental care tactics in each specific case. The professional cleaning procedure should be carried out 2 times a year to remove accumulated dirt that regular cleaning cannot remove. This is especially true for patients with braces or dentures - the presence of foreign structures in the mouth requires regular professional cleaning.
It is necessary to treat teeth so that there are no putrefactive processes in the mouth, and there are as few pathogenic bacteria in the microflora as possible. And if the cause of stomatitis or contributing factors were disturbances in the functioning of the body, then you need to closely monitor your health and maintain your immunity.
Candidal stomatitis
In 80% of healthy children, Candida fungi can be found in the oral cavity. They get there during childbirth, from nipples and pacifiers, from care products, in contact with the mother's skin, with food during eating and usually do not cause any problems. Candidal stomatitis, or thrush, occurs when immunity decreases1.
Predispose to the disease:
- prematurity and postmaturity;
- developmental defects and concomitant diseases;
- treatment with antibiotics and hormones;
- artificial feeding;
- poor care and poor feeding hygiene;
- Using the wrong nipples1.
What does candidal stomatitis look like? In children's mouths, whitish or whitish-gray dotted formations appear on the reddened mucous membrane. They merge into films of a cheesy nature; when the films are rejected, bright red painful erosions are formed. Because of the pain, the baby becomes restless, cries often, sleeps poorly, and refuses to eat1.
In severe cases of candidiasis, a cheesy coating may appear on the palate and on the lateral surfaces of the tongue, on the tonsils and the back wall of the pharynx - candidal tonsillitis and pharyngitis develop1.
If your child has a fungal infection, you should always consult a doctor; he will tell you how and what to treat the mucous membrane with candidal stomatitis, so that the child does not have complications and recovers faster. Treatment, as a rule, involves treating the oral cavity with drugs with antifungal activity (chlorhexidine, hexethidine). In severe cases of the disease, antifungal agents, probiotics and immunomodulators are prescribed1.
Up to contents
Incubation period
When any virus enters the human body, there is an incubation period during which symptoms do not appear or do not indicate a specific type of virus. It is impossible to predict the incubation period of the virus before the onset of stomatitis, because:
- The type of virus itself is not known.
- It is not known whether stomatitis will occur at all or whether it can be avoided.
However, in cases of stomatitis, it is noticed that the virus is activated within a period of several days (herpes, measles, adenoviruses) to two weeks (chickenpox). And with proper treatment it goes away in about a week or two.
In cases of herpes, the virus most often remains dormant in the host’s body after treatment. At the same time, others can become infected, and the person himself, until the level of immunity sharply decreases against the background of other diseases, will feel completely healthy.
How to treat stomatitis
For any form of stomatitis, treatment begin with a visit to the doctor's office. The dentist must determine the form and severity of the disease in order to prescribe appropriate therapy. Self-medication may not bring results and thus aggravate the situation, allowing the disease to progress to a more severe stage.
The diagnosis of “stomatitis” is made by the doctor after an examination, and after that he can prescribe the patient to take an oral smear to find out the exact cause of the disease. PCR analysis of the biomaterial will show the presence or absence of a pathogen, for example a Candida fungus or a herpes virus. If the cause is not the pathogen, an additional visit to another doctor may be required. Thus, if allergic stomatitis is suspected, the patient will be referred to an allergist, and if immunity or metabolic disorders are suspected, the patient will be referred to an immunologist or gastroenterologist.
In addition to establishing the cause of the disease, the patient receives recommendations on how to treat stomatitis in his case , including:
- ✔️ Bringing oral hygiene back to normal and further supporting it;
- ✔️ Treatment of ulcers with special means, depending on the diagnosis - antiseptic, antiviral or antifungal;
- ✔️ Pain relief with anesthetics;
- ✔️ Use of products that eliminate inflammation and swelling;
- ✔️ Following a diet to restore the mucous membrane.
Although stomatitis is treated with drugs , the patient needs to adhere to a diet so that food does not cause mechanical damage to the already inflamed mucosa. You will have to exclude hard, sour, spicy and overly salty foods from your diet. The menu will be similar to what is prescribed for gastrointestinal diseases: boiled products crushed to a puree state, liquid porridges and broths, fermented milk products. Everything is warm temperature, nothing hot or cold. Even soft bread will have to be removed, as it can scratch irritated areas in the mouth. For children, the doctor gives recommendations depending on their age.
Features of treatment
As is often the case with diseases that are at the intersection of several areas of medicine, inflammatory lesions of the oral mucosa are one of the least studied areas of dentistry. Therefore, several specialists can be involved in the treatment of stomatitis in children in the mouth: pediatrician, dentist, dermatologist, immunologist-allergist, otolaryngologist, etc. This is especially convenient when you go to a multidisciplinary clinic.
Self-medication of stomatitis is unacceptable, and although it is now easy to find ready-made treatment regimens and folk recipes, it is important not to experiment with the baby’s health.
Conservative treatment is mainly used, which involves treating the underlying cause of the disease. Your doctor may prescribe the following medications:
- antibacterial drugs (systemic and local in the form of ointments): for bacterial inflammation;
- antiviral agents for herpes and other types of viral stomatitis;
- antifungal drugs for fungal diseases;
- antihistamines - both for allergic origin of stomatitis, and as part of complex therapy to reduce swelling and itching;
- symptomatic drugs - anti-inflammatory, analgesic, antipyretic.
Treatment of candidal stomatitis in infants should be carried out with caution. At the same time, it is important to pay attention to your health; sometimes the cause of such a disease can be insufficient breast hygiene during lactation.
Often, only local remedies are sufficient, but make sure that the entire oral cavity is treated with the rinse - inflammatory agents can be found on the entire surface of the mucous membranes. Healing applications can be used to a limited extent, only on areas of inflammation.
Treatment of stomatitis of any kind in children involves strict adherence to a diet. The diet should be gentle, it is important to avoid salty, spicy, sour foods and drinks, serve the child warm meals, and limit the consumption of sweets.
If traumatic stomatitis occurs, the doctor will prescribe medications to speed up healing. However, it is very important to prevent re-injury. If it was caused by sharp edges of a tooth or filling, this cause should be eliminated. The doctor will suggest grinding off the filling or replacing it, and will also choose the appropriate option for restoring the shape of the crown in case of chips and cracks.
Is stomatitis contagious?
Canker sores can be contracted if the condition is caused by a virus, fungus, or infection. The pathogen is easily transmitted through shared objects and airborne droplets.
Children are especially susceptible to infectious stomatitis - due to their age, the mucous membranes of the oral cavity have not yet formed the required level of protection. Aphthous stomatitis is especially severe in infants, including those with damage to internal organs. Adults have a chance of getting sick only when they have microcracks or abrasions in the mouth.
Fungal stomatitis is transmitted through water, dishes, and food.
Stomatitis that develops as a result of vitamin deficiency, stress or mechanical trauma is not contagious.
Stomatitis in adults
Stomatitis affects the oral mucosa, causing inflammation and the appearance of painful ulcers (ulcers) of varying sizes. If left untreated, erosions can affect the pharynx, tongue, lips and cheeks. The disease mainly affects children, however, among the adult population, the incidence of stomatitis is at a fairly high level - according to WHO statistics, every fifth person experiences the disease. Stomatitis in adults can develop for various reasons, the main ones include:
- diseases of the gastrointestinal tract,
- nerve diseases,
- taking certain medications,
- incorrectly installed dentures,
- avitaminosis,
- allergic reaction.
The risk group also includes people with bad habits and weakened immune systems.
Diagnostic features
A dentist can detect stomatitis during the first visual examination. But in controversial cases, laboratory tests may be required. Thus, bacterial inflammation may require identification of the causative agent of the disease and its sensitivity to antibiotics. A scraping and/or virological study will help determine the cause of the disease and prescribe appropriate treatment.
If a combination of several ailments with a similar picture is suspected, as well as if the child’s general well-being deteriorates, laboratory tests of blood and urine and consultations with other specialists may be prescribed.
Sometimes stomatitis can be the first manifestation of systemic diseases, general somatic pathology, for example, diabetes mellitus or malignant neoplasms. Therefore, a timely visit to the doctor is extremely important.
Preventive measures
A very important part of prevention is timely treatment of dental and ENT diseases.
Stomatitis can occur in anyone, regardless of age and lifestyle, but compliance with the following preventive measures can reduce this risk:
- Maintaining oral hygiene and timely treatment of dental diseases.
- Providing a balanced diet to supply the body with the necessary amount of vitamins and nutrients.
- Taking vitamin complexes in spring and autumn.
- Timely treatment of diseases of the ENT organs and digestive system.
- Rejection of bad habits.
Causes
Viral stomatitis begins as a complication of the underlying disease, be it herpes, chickenpox or any other. The likelihood of developing stomatitis in a healthy person who takes care of his teeth and does not neglect the rules of personal hygiene is very small, so the root cause of stomatitis may not even be the virus itself, but the initial problems of the oral cavity. For example, chronic advanced caries, periodontal disease, gingivitis, against the background of which the degree of resistance to viral infections is significantly reduced.
Even poor nutrition, vitamin deficiency and lack of minerals in the body can be a prerequisite for the development of viral stomatitis. With low local immunity of the oral cavity, any virus can provoke serious consequences.
Another reason is the presence of sick pets in the house. Unfortunately, vesicular stomatitis is transmitted from animals to humans, so the owners of an animal with an acute infection must maintain careful hygiene and limit close contact with the pet as much as possible until it recovers.
What it is
Like any other, viral stomatitis is an inflammation of the soft tissues of the oral cavity, caused by a virus and accompanied by pain and rashes of various kinds.
The initial stage of the disease, depending on the type of virus and the strength of the immune system, can be characterized by a slight sore throat, lethargy and the first signs of viral infections (fever, chills, enlarged lymph nodes and even a cough with a runny nose). If the body's resistance is low, the reaction can be much more serious, including complete refusal of food due to severe pain. 1-3 days after the onset of the disease, rashes appear in the mouth (aphthae, blisters, ulcers), bleeding of the gums may occur with obvious swelling, and most often a putrid odor appears from the mouth.
The “stomatitis” virus, or more precisely, the virus that causes it, can be anything, since stomatitis itself is simply a reaction of the body that may or may not occur for a number of reasons. Most often, viral stomatitis appears against the background of infection with chickenpox, herpes, influenza, measles, adenovirus and rotavirus infections.
Most often, the lesion occurs in the corners of the lips or on the oral mucosa and is popularly called fever. This manifestation of stomatitis is inherent in the herpes virus, and children under three years of age are most susceptible to this disease. In 80% of sick children this virus will be the cause. With good body resistance and a high level of immunity, viral stomatitis passes without a trace, however, in weakened people it can also acquire a chronic form.