Introduction
Damage to the mucous membrane of the gastrointestinal tract (GIT) and gastrointestinal bleeding (GIB) in cardiac patients are quite common. According to the Russian Register of Patients with Stable Coronary Heart Disease (REGATA), the incidence of serious bleeding in such patients is 1.9 per 100 patients per year [1]. According to the Russian multicenter ORACLE study, the incidence of serious bleeding in patients who suffered acute coronary syndrome was 0.8%, clinically significant - 2.4%. Of these, about 20% are represented by gastrointestinal tract diseases [2]. It is known that the risk of death and atherothrombotic complications in patients who have suffered bleeding is higher [3]. The most commonly used antithrombotic drug in cardiological practice is acetylsalicylic acid (ASA). A recently published meta-analysis analyzed the bleeding risks associated with long-term use of ASA in real-world clinical practice. The analysis was conducted on studies published between 1946 and 2015. Overall, the incidence of upper GI bleeding was estimated to be 0.48 to 3.64 per 1000 person-years. The frequency varied quite markedly depending on the dose of ASA. Neither the form nor the total duration of use had a significant effect on the risk of bleeding. The risk of gastrointestinal lesions increased with the combined use of ASA and nonsteroidal anti-inflammatory drugs (NSAIDs), anticoagulants, and serotonin reuptake inhibitors [4]. All this makes us look for possible ways to minimize the risk of bleeding without compromising antithrombotic therapy (“bleeding avoidance strategy”).
Bleeding prevention and proton pump inhibitors
Modern recommendations consider the administration of proton pump inhibitors (PPIs) as the main method of preventing gastrointestinal lesions and preventing gastrointestinal tract infections. Russian guidelines for the management of patients with stable coronary artery disease (CAD) report that “patients with stable ischemic heart disease with a high risk of gastrointestinal bleeding or with a history of gastrointestinal bleeding receiving ASA or a combination of several antithrombotic agents to protect the gastric mucosa and for the prevention of gastrointestinal tract infections, it is recommended to use PPIs (if indicated - prevention of erosive and ulcerative lesions of the stomach and duodenum associated with the use of non-steroidal anti-inflammatory drugs)" [5]. A meta-analysis of studies on the prevention of gastrointestinal lesions showed that, in general, PPIs are more effective in terms of preventing bleeding and erosive and ulcerative lesions of the gastrointestinal tract. During therapy with H2-histamine receptor blockers, the risk of bleeding was 2.102 times higher, and the risk of other gastrointestinal lesions was 2.257 times higher [6]. The previously existing approach suggested replacing ASA with other antiplatelet agents, primarily clopidogrel, as a means of preventing gastrointestinal tract infections. Currently, this approach is not used, since in high-risk patients who have already suffered bleeding, it turned out to be less effective than adding a PPI to ASA. This was shown in a meta-analysis of 2 small studies that included 490 patients who suffered from gastrointestinal tract while taking low doses of ASA. The risk of rebleeding with PPI therapy was much lower than with clopidogrel therapy (OR 0.06; 95% CI 0.01–0.34) [7].
The use of PPIs is an effective, but not absolute, way to prevent gastrointestinal pathology. Among patients receiving low doses of ASA and PPI for a long time, risk factors for the development of erosive and ulcerative lesions of the upper gastrointestinal tract were analyzed. Of the 237 patients observed, severe gastrointestinal lesions were detected in 65. Independent predictors of gastrointestinal lesions were the use of anticoagulants and initial anemia. Smoking and a history of chronic gastritis tended to influence the risk of gastrointestinal lesions [8]. Thus, in a significant number of patients from the highest risk categories, despite preventive therapy, the likelihood of complications remains.
Proton pump inhibitors are effective primarily as a means of preventing upper gastrointestinal lesions. A randomized multicenter trial showed that the use of the PPI pantoprazole in patients receiving rivaroxaban or ASA led to a reduction in the risk of upper gastrointestinal bleeding, but not in a reduction in the risk of developing any gastrointestinal lesions, including erosive-ulcerative lesions without bleeding, penetrance, etc. p. [9].
It should be noted that the prevention of gastrointestinal damage in cardiac diseases requires a fairly long-term use of PPIs. In particular, prophylactic PPI is recommended for the entire period of triple antithrombotic therapy, including 2 antiplatelet agents and an anticoagulant. The maximum duration of such therapy can reach 6 months. [10]. If long-term treatment is necessary, the question arises about the safety and risks associated with this therapy.
A recently published meta-analysis provided data on the side effects of long-term PPI use. With long-term prophylactic use of these drugs, an increase in the risk of infectious diseases, primarily intestinal infections, has been described, which is associated with suppression of gastric acid production. Clostridioides difficile infection
increases by 1.74 times, other gastroenteritis - by 3.3 times, salmonellosis - by 4.2 times. The meta-analysis did not show a significant increase in the risk of liver disease. 2 studies showed a significant increase in the risk of pneumonia. A decrease in the acidity of gastric juice can lead to a decrease in the ionization of calcium compounds and impaired absorption. This theoretical assumption, although confirmed by several studies, however, the evidence obtained in them turned out to be weak and unreliable. There are also conflicting data regarding vitamin B12 malabsorption. More uniform data have been obtained regarding the risk of hypomagnesemia, especially pronounced with the combined use of PPIs and diuretics. Theoretically, it is also possible that the absorption of iron ions may be impaired, but this apparently has no clinical significance. Cases of the development of acute kidney injury have also been described, but they are isolated and their risk is not associated with the duration of the drug [11]. Observational studies also provided evidence of an increased risk of dementia with long-term PPI therapy [12]. It should be noted that there is no evidence of an association of dementia risk with PPI use in controlled studies. Overall, although there is a risk of some adverse effects, PPI therapy remains the primary means of reducing bleeding risks during antithrombotic treatment.
Prevention of oral inflammation
Timely visit to the dentist.
The main prevention of inflammatory diseases is timely visit to the dentist. The doctor will prescribe a course of treatment for the oral cavity, eliminate traumatic factors (inappropriate dentures, sharp edges of teeth) and sources of infection (periodontal pockets, carious teeth).
Proper nutrition.
The diet should include food that is complete in composition and quality. It is recommended to consume foods rich in vitamins A, B, C and microelements (fluorine, copper, calcium) that are beneficial for healthy teeth and gums. Carbohydrates are a breeding ground for the development of pathogenic microflora, so their abuse can lead to oral diseases. Food should contain a balanced amount of proteins, fats and carbohydrates. The condition of teeth is negatively affected by the consumption of soft foods, so the diet should include solid foods, especially vegetables and fruits. This is necessary to “train” the chewing apparatus. Special diets for the prevention of diseases have not been developed; the main thing is to adhere to the rules of a healthy diet.
Oral hygiene.
You should brush your teeth 2 times a day: in the morning and before bed. The toothbrush must be chosen individually. Its head should be curved and slightly tapering towards the end. Excessively thick bristles reduce the cleaning effect of the toothbrush and make it difficult to care for. After brushing your teeth, rinse the brush thoroughly under running water and place the bristles up in a glass. Once every 2-3 months, the brush must be changed, as it wears out, which reduces the cleaning effect and leads to the accumulation of microorganisms - the cause of infections that affect the oral cavity. You can clean the interdental spaces using interdental brushes or dental floss. It is also recommended to use mouthwash regularly. Check out the LISTERINE® range of mouth rinses - used twice daily to help maintain healthy teeth and gums.
Up to contents
The problem of gastric dyspepsia and adherence to therapy
It should be noted that the problem of bleeding does not exhaust the risks associated with the use of antithrombotic drugs, and in particular the most commonly prescribed ASA. A significantly larger number of patients receiving antiplatelet agents have gastrointestinal pathology (gastritis, erosions, ulcers). Thus, according to a Japanese study, among 400 patients receiving low doses of ASA (75–325 mg/day), endoscopy revealed various pathological changes in the stomach or duodenum in 64% of those examined, and ulcerative defects in 10% [13 ]. In general, symptoms of gastric dyspepsia when using ASA occur 1.46 times more often than when using NSAIDs, antipyretics, etc. This was shown in a meta-analysis that included more than 19,000 patients [14]. The presence of gastrointestinal pathology, even in the absence of bleeding, is a very significant problem for a practicing physician, since the presence of clinical symptoms of gastric dyspepsia, as a rule, reduces patients’ adherence to treatment. It should be noted that low adherence often determines the phenomenon of pseudo-resistance to ASA, when due to non-compliance with the drug regimen it is not possible to achieve the desired effectiveness of therapy. A meta-analysis of studies in which ASA was used in patients with stable coronary artery disease showed that low adherence to treatment can increase the risk of major atherothrombotic events by 2.4 times [15].
Low adherence to therapy in patients receiving ASA is often associated with the presence of clinical symptoms of damage to the upper gastrointestinal tract - heartburn, belching, epigastric pain, etc. Secondary feelings of anxiety and sleep disturbances may develop. In patients with low adherence to treatment with ASA, the prescription of PPIs for the management of gastrointestinal lesions often does not lead to success, since adherence to the use of PPIs also turns out to be low against the background of existing symptoms [16]. A population-based study conducted in China from 2000 to 2009 showed that the prescription of NSAIDs was decreasing slightly and the number of people receiving low-dose ASA for various indications was increasing, with 76% of patients receiving ASA being classified as high risk of bleeding . Adherence to gastroprotective therapy among patients receiving ASA was low (only about 35%), which may affect the incidence of gastrointestinal tract and gastrointestinal lesions in these patients [17].
Protected forms of ASA: features of their effectiveness and safety
Acetylsalicylic acid in cardiological practice can be used both in simple (unprotected) form and in protected forms. To protect the gastrointestinal mucosa, forms of ASA are used, which contain a small amount of antacid - buffer forms, which, like regular ASA, dissolve in the stomach, as well as enteric-coated forms (coated), which dissolve and are absorbed in the alkaline environment of the small intestine , which may affect the bioavailability of drugs. Buffer forms include a drug such as Cardiomagnyl (“Stada”).
The presence of an enteric coating can change the form of ASA and the bioavailability of the drug. Modern experiments using electron microscopy have shown that when using coated forms of ASA, the release of the drug can be reduced by 10–20%, while its crystal structure changes, which may affect its effectiveness and raises the question of the development of new forms of protected ASA [18] .
Using mass spectrometry, the pharmacokinetic parameters of ASA were assessed in patients receiving coated and conventional forms of the drug. When using enteric forms, there was generally greater variability in the pharmacokinetics of the drug. In one of the patients, there was a significant (8 hour) delay in the onset of increase in drug concentration in the blood plasma. The area under the curve of ASA concentration when using coated forms was also smaller, although in general a decrease in thromboxane concentration was noted in both groups [19].
An experiment on animals (rats) also showed that buffer forms of ASA are practically no different in kinetics from simple forms, while the enteric coating can reduce the adsorption of ASA due to the alkaline pH of the intestine [20].
An analysis of the effectiveness of the enteric form of ASA was carried out on a group of 131 patients who received the enteric form of ASA at a dose of 75 mg/day in connection with coronary artery disease. In this group, 44% of patients while taking ASA had high levels of thromboxane A2. These patients were more likely to have high levels of platelet aggregation. Predictors of insufficient effectiveness of ASA were patient age and body weight. Apparently, the lack of effectiveness of ASA is associated with a decrease in drug absorption [21].
The lack of effectiveness of enteric forms may be especially significant for patients with diabetes mellitus (DM). In such patients, on the one hand, the risk of cardiovascular complications is significantly higher, and on the other hand, changes in the gastrointestinal mucosa cause disturbances in the bioavailability of drugs. A study of the pharmacokinetics and pharmacodynamics of 3 forms of ASA was conducted on a group of 40 patients with diabetes. A conventional, enteric form of ASA and a new, fat-soluble, sustained-release form were used. When using the enteric form, more than 50% of patients demonstrated resistance to ASA (when using other forms, the proportion of such patients was 15% and 8%). Resistance was assessed by thromboxane levels. The large number of patients with an insufficient response to the enteric form of ASA correlated with reduced parameters of ASA kinetics in the blood plasma in these patients [22]. Similar data were obtained in a Russian single-center study that compared enteric and buffered forms of ASA. In patients with diabetes, the decrease in sensitivity to the enteric form was significant [23].
A meta-analysis of 7 studies was conducted that examined the pharmacodynamic parameters of unprotected and enteric forms of ASA. The studies included a small number of patients, but it was shown that the use of enteric forms of ASA leads to a decrease in the effectiveness of ASA, and the effect on thromboxane levels and platelet aggregation was less. These effects may be due to decreased bioavailability. When using enteric forms of ASA, larger doses may be required than when using simple and buffer forms [24].
In a small meta-analysis of 3 studies using the enteric form of ASA, 54% of patients showed a reduced response to the drug. When using the conventional form of ASA, the proportion of patients with an insufficient response was only 8%. A predictor of insufficient effectiveness of the drug was the patient’s excess body weight [25].
Similar data were obtained in the treatment of patients with essential thrombocythemia. The use of enteric-coated ASA in this case led not only to greater variability in pharmacokinetic parameters, but also to a decrease in the antiplatelet effect compared to the conventional form of the drug [26].
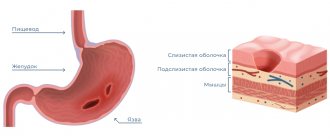
It should be noted that the main mechanism of damage to the gastrointestinal mucosa during treatment with ASA drugs is associated with the systemic effects of ASA, the influence on the synthesis of protective factors of the mucosa. This has been demonstrated, in particular, in animal experiments. In an experiment on rats, it was shown that ASA infusion causes dose-dependent damage to the gastrointestinal mucosa in animals, and the addition of clopidogrel and ticlopidine increases the risk of gastrointestinal tract infections [27]. The incidence and severity of gastric mucosal lesions during treatment with low doses of ASA were analyzed in an observational study that included 259 initially healthy individuals over the age of 45 years receiving ASA. The average follow-up period was about 5 years. More than 2,000 endoscopic examinations were performed as part of the study. It has been shown that the maximum frequency and severity of mucosal lesions are observed in the first 2 years of taking ASA. Erosion is most often recorded. The frequency of detection of lesions of the gastric mucosa increases with the age of patients [28].
There are data from some studies that have shown the advantage of protected forms, primarily buffer forms. A small 12-week study compared endoscopy findings in patients taking regular, buffered, and enteric ASA. With regard to damage to the gastric mucosa, the buffer form turned out to be somewhat safer, and with regard to damage to the duodenal mucosa, no significant differences were found between the drugs [29]. An analysis of 550 cases of gastrointestinal tract and 1220 control cases showed that the risk of bleeding increases with the use of ASA, and at dosages less than 325 mg/day, no significant differences in the risk of bleeding were found when using regular, buffered and enteric forms of ASA. For dosages greater than 325 mg/day, data are only available for regular and buffered forms of ASA. The risk of bleeding is higher when using larger doses, but no significant differences were found between the regular and protected forms [30]. A large meta-analysis of 50 studies of antithrombotic therapy showed that ASA doses of 100 mg or less had a lower risk of all bleeding events than higher doses of ASA and other antithrombotic agents. It should be noted that when using different doses of ASA, the risk of minor (“minor”) bleedings differed mainly, but the risk of significant bleedings did not differ significantly [31].
The use of protected forms of ASA can still affect the severity of clinical symptoms and symptoms of dyspepsia. In the work of E.P. Yakovenko et al. [32] showed that pain and gastric dyspeptic disorders were detected significantly more often in patients taking enteric-coated ASA. The buffer form of ASA was better tolerated. The frequency of detection of erythematous-hemorrhagic changes in the mucous membrane of the stomach and duodenum without ulcers and erosions in the group of patients receiving a buffer form of ASA was much lower. The frequency of detection of erosions and ulcers, as well as the severity of damage to the mucous membrane of the stomach and duodenal bulb did not differ significantly between the groups. In a large Danish population-based study, symptoms of gastric dyspepsia associated with taking different forms of ASA were analyzed based on a survey of patients. More than 50,000 questionnaires were distributed, and 16,715 questionnaires (32%) were received: 911 (5%) patients reported taking the regular form of ASA, 633 (4%) reported taking the enteric form of ASA. The frequency of dyspepsia symptoms while taking a protected form of ASA was even slightly higher than when using a simple form (27.5% and 26.3%, respectively). The frequency of individual symptoms also did not differ, thus, the enteric form of ASA did not protect against gastric dyspepsia [33].
Lesions of the gastrointestinal tract when using ASA are not limited only to the gastric mucosa. From studies conducted using cassule endoscopy, it is known that with the use of ASA, the frequency of lesions of the small intestine also increases. It has been shown that when using enteric forms, the number of intestinal ulcers increases. The incidence of erosive lesions when using enteric forms was also higher than when using buffer forms [34].
The frequency of erosive and ulcerative lesions of the gastrointestinal tract was studied in elderly patients (over 60 years old) and middle-aged patients (45–60 years old). All patients were comparable in terms of basic clinical characteristics (except age) and received low doses of enteric-coated ASA. The condition of the small intestine was studied using capsule endoscopy. The frequency of erosive lesions of the gastrointestinal tract was significantly higher in the elderly (88.2% and 44.1%; p<0.001), and the frequency of severe damage to the intestinal mucosa also differed significantly (32.4% and 8.8%; p=0.033) [35 ].
Causes of oral diseases
Infectious diseases.
Sometimes inflammation occurs against the background of an infectious disease. The provoking factor can be a herpes virus, influenza, etc. The most common cause of inflammation is the herpes simplex virus.
Mechanical damage.
The oral cavity can become damaged as a result of a blow, injury from a foreign object, or unsuccessful biting. Usually, after an injury, pain immediately occurs, and then a small hemorrhage forms in the form of erosion, ulcer or hematoma. Mechanical damage can be chronic, and this problem is not uncommon. For example, the cause of regular injuries to the mucous membrane are sharp edges of the teeth, dentures that are not fitted correctly, as well as bad habits such as biting the cheek, lips, etc.
Physical damage.
Physical damage includes electrical shock, exposure to low or high temperatures, and radiation. If left untreated, the oral cavity becomes inflamed and ulcers and blisters can form.
Chemical damage.
The oral cavity can be injured when the mucous membrane comes into contact with acids or highly concentrated alkalis, for example, due to an error in production or carelessness at home. After an acid burn, a thick film appears on the mucous membrane, and redness and swelling appear at the edges. When an alkali burn occurs, the deep layers of the mucous membrane are often affected, so a film does not form, but erosions and ulcers occur, which take a long time to heal and painfully.
Note!
Contact your doctor immediately if the following symptoms appear:
- acute pain at the site of injury, increased body temperature;
- discharge of purulent contents when pressing on the gums;
- the formation of sores or areas covered with a white coating on the gums, tongue or mucous membrane;
- appearance (increase) of tooth mobility;
- difficulty chewing food;
- the duration of the inflammatory process is more than 3-5 days.
Up to contents