From this article you will learn:
- the gums around the wisdom tooth are inflamed: what to do,
- wisdom tooth: hood and its removal (price for 2021),
- how to relieve inflammation.
The article was written by a dental surgeon with more than 19 years of experience.
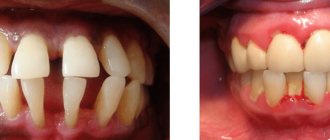
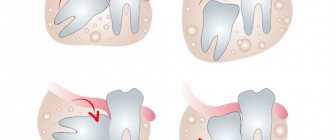
Difficulty in the eruption of wisdom teeth is often accompanied by the development of inflammation of the gums around them. The mucous membrane of the gums, which partially covers the crown of the erupting wisdom tooth, is called the wisdom tooth hood (Fig. 1-3).
Because The hood over the wisdom tooth is not tightly adjacent to the crown of the tooth - a semi-closed space is formed between them, in which favorable conditions are created for the proliferation of pathogenic bacteria and the development of inflammation. In dentistry, an inflamed hood on a wisdom tooth is usually called “pericoronitis.”
What is complex wisdom tooth extraction?
Tooth extraction is called complex if the tooth has several roots, and the operation will require an incision into the soft tissue of the gums and, possibly, the periosteum. Another difference from classic removal is the need to use additional tools (except for forceps and an elevator). The difficulty of performing surgical intervention is due to the difficulty of accessing the extreme elements of the dentition, the root features of the “eights” and the specifics of the clinical case (they are often dystopic or impacted).
Important: you cannot postpone the removal of the defective “eight”. This can lead to suppuration and, as a consequence, to the formation of an abscess and the development of sepsis.
Causes of caries
The main reason for the appearance of caries in wisdom teeth is their location. The third molars erupt last and at the very end of the dentition. The distant location greatly complicates the process of daily brushing of teeth. If the lower eights are visually accessible and if the cleaning with a toothbrush is poor, the procedure can be repeated, then the upper molars remain in a “blind” and hard-to-reach area.
Bacterial plaque, which gradually accumulates on the walls of the tooth, begins to destroy the enamel. Due to the absence of signs of damage at the initial stage and poor visibility of the tooth itself, the carious process progresses and penetrates deeper. As a rule, people turn to the dentist already at the stage of deep caries or pulpitis.
The cause of wisdom teeth caries can also be:
- carious lesion of the adjacent tooth;
- caries of the opposite eight.
Impacted, that is, partially erupted figure eights, are also often affected by caries, despite the fact that they are partially hidden by the gum. With insufficient hygiene, food particles and bacterial deposits penetrate under the gingival hood. As a result, the process of tissue destruction begins.
Indications and contraindications for surgery
Indications
Surgery is necessary if the wisdom tooth:
- Dystopic (the direction of growth is changed towards adjacent teeth, tongue or cheek)
- Impacted (not fully or not fully erupted)
- Has roots that are too long (this may initiate their penetration into the maxillary sinus or fusion with the jaw)
- Caused inflammation of the “hood” of the gums or periodontal tissue (pericoronitis)
- Caused the formation of a follicular cyst, phlegmon, gumboil or fistula
- Destroyed due to the development of caries or other dental disease
- Caused inflammation of the trigeminal nerve
- Became a source of permanent injury to the oral mucosa
- Interferes with the eruption of other molars with a narrow jaw
Absolute contraindications:
- Malignant tumor in the root zone
- Hemangioma (benign formation)
- Serious chronic cardiovascular problems
Relative (temporary) prohibitions:
- Infectious diseases, including those of the oral mucosa
- Having had a heart attack or stroke
- Taking anticoagulants
- Exacerbation of psychoneurological diseases
- Pregnancy and breastfeeding (except for emergency indications)
Differences between figure eight removal on the lower and upper jaws
Removing a third molar in the lower jaw is considered a more complex procedure than removing a wisdom tooth in the upper jaw for a number of reasons.
- Access to the lower molars is more difficult than to the upper ones.
- The lower jaw bone is more massive and dense, it holds the tooth more firmly.
- The pressure on the teeth of the lower jaw is greater than on the upper teeth, so the roots of the lower molars are more developed. In addition, due to improper growth, they can be curved or misaligned.
- It is easier to perform local anesthesia from above, and anesthesia from the bottom often involves the muscles of the face, tongue, throat and ears.
All this makes the procedure for removing the 8th tooth from below a difficult task. If the upper molars in most cases can be easily rocked and pulled out with special forceps, then the lower molars often have to be removed in parts, cutting with a drill.
Removing the "hood"
Often, difficult eruption of a wisdom tooth leads to inflammation of the gums that cover it (“hood”). This causes enlargement of the lymph nodes, increased temperature, pain when chewing, injury to the gums and, as a result, rapid proliferation of pathogenic bacteria, leading to inevitable suppuration. This situation occurs quite often and is an indication for excision of gum tissue. If the “eight” under the hood is viable and does not cause inconvenience, then it is not removed.
When to carry out the procedure and when to refrain from it
Indications for the procedure:
- strong pain;
- the appearance of putrid odor from the mouth;
- discharge of pus from the gums;
- swelling, bleeding and soreness of the gums;
- general weakness, elevated body temperature, dizziness and nausea (such symptoms are a sign of intoxication of the body).
Contraindications:
- mucosal infections (stomatitis, herpes, gingivitis, periodontitis);
- infectious diseases of the upper respiratory tract (sore throat, pharyngitis, laryngitis, etc.);
- exacerbation of chronic diseases.
Types of anesthesia
Performing surgical interventions is impossible without high-quality anesthesia. During extractions, the following types of anesthesia can be used:
- infiltration anesthesia – provides a local effect. Injected with a syringe into the gum or intraosseously. This is the most common option for dental procedures;
- conductive - has a more powerful effect and is used when operating on particularly complex cases. The injection is carried out to the branches of the trigeminal nerve;
- intraligamentary - used to anesthetize one tooth. The medicine is injected with a syringe into the ligament that holds the tooth in the alveolus.
Expert opinion: Some patients want dental surgery to be performed under general anesthesia. But this type of anesthesia is not as harmless as it is described in advertising articles. It has been proven that it negatively affects the patient's health. An operation to remove teeth, even such complex ones as the “eight”, is not a direct indication for the use of general anesthesia (with rare exceptions). Surgery is painless with the correct selection of local anesthetic. Therefore, you should not strive for general anesthesia and put unnecessary drug burden on the body.
Expert opinion
Emir Romanovich Omerelli
Maxillofacial surgeon, implantologist
Experience: more than 13 years
Impacted wisdom teeth are a “popular” reason for patients to visit dental clinics. In approximately half of all cases, the eighth teeth erupt with problems, and retention is the most common. It is interesting that the age of patients can be different - from 18 years to deep retirement age. It all depends on how much the impacted tooth bothers the patient. However, the sooner the problem is solved, the less problems an unerupted tooth will cause.
After surgery, it is very important to follow the precautions recommended by your doctor: you must refrain from eating for two hours after tooth extraction. For a couple of days, the food consumed should be warm - not too hot and in no case cold. It is necessary to chew on the side opposite to the operation site. You should also avoid physical activity for a while. You can brush your teeth, but as carefully as possible so as not to damage the sutures. Do not forget about the need to take antibiotics and medications that restore the body’s immune system - they will be prescribed by your doctor.
Other jobs
Instruments used during surgery
When performing complex extractions, the surgeon may need the following instruments:
- forceps – for extracting a tooth or its elements if they can be grasped. There are different shapes: straight, curved, S-shaped;
- elevator - for loosening entire dental units or their roots in the alveolus;
- excavator - for removing fragments from a deep root fracture;
- scalpel - for cutting soft tissues;
- drill or chisel - for sawing (splitting) large elements of the root or coronal parts with a very dense bone structure.
Stages of surgery
The G8 extraction protocol implies a strict sequence of certain stages:
- diagnosis of the clinical situation. It is carried out by the surgeon when the patient comes for an appointment. First, the doctor conducts a visual examination, determining the extent of damage to the tooth and surrounding tissues. Next - mandatory radiography for an objective assessment of the current condition. The image allows you to clarify the details of the clinical case: the number of roots, possible interweaving, angle of inclination. If necessary, the examination is supplemented by orthopantomography (obtaining an image in 3D format);
- determination of the type of anesthetic and its dose. Questioning the patient about the presence of allergic reactions to any medications;
- injection of an anesthetic drug into the surgical area. The mechanism of action of the anesthetic is as follows: the substance acts on the nerve, it stops transmitting impulses to the brain. As a result, after 5 to 10 minutes a person stops feeling pain in the place where the medicine was injected. After some time (up to 6 hours), it stops working, the transmission of nerve impulses is restored;
- the operation itself. Typically lasts from 30 minutes to one and a half hours. Complex removal involves cutting the gums with a scalpel and stitching them together upon completion of surgical procedures. An incision into the gum tissue allows the surgeon to reach the root system. Then the doctor, using a drill and/or chisel, saws (splits) the molar into several parts and takes it out in separate pieces. If necessary, the roots are taken out in the same way. After all parts are removed, the hole is treated with an antiseptic, and the incision is sutured with surgical threads;
- At this point the operation ends, the surgeon gives the patient recommendations on oral care.
Note: extraction can only be performed by a qualified dental surgeon in a medical institution in compliance with aseptic and antiseptic standards.
How is the procedure performed?
Before starting the procedure, the dental surgeon takes into account all the individual characteristics of the patient: age, allergic reactions, chronic diseases, etc. After making sure that the procedure can be carried out, the doctor begins excision.
Stages of excision of the hood:
- X-ray diagnostics.
- Local anesthesia.
- Gum incision.
- Washing the wound.
- Applying a therapeutic bandage.
After surgery, the doctor schedules a follow-up appointment to examine the wound. As a rule, the gums heal in about ten days. If the process is delayed, this may be a symptom of complications.
Possible complications
Successfully performed surgery and following the doctor’s recommendations minimize the risk of complications. But they are still possible. This:
- severe pain that continues for several days;
- heavy bleeding from the surgical wound;
- inflammatory process (characterized by swelling of the gums, cheeks, and a significant increase in temperature);
- osteomyelitis of the jaw;
- loss of sensitivity in some areas of the face (parasthesia). Possible if the facial nerve is damaged.
Attention! All of the above symptoms are a good reason to immediately consult a doctor. Waiting “for it to resolve on its own” is unacceptable; this can lead to serious consequences, including sepsis.