The nerves of the eye are usually divided into three groups: motor, secretory and sensory.
Sensory nerves are responsible for regulating metabolic processes and also provide protection, warning of any external influences. For example, a foreign body entering the eye or an inflammatory process occurring inside the eye.
The task of the motor nerves is to ensure movement of the eyeball through coordinated tension of the motor muscles of the eye. They are responsible for the functioning of the dilator and sphincter of the pupil, and regulate the width of the palpebral fissure. The motor muscles of the eye, in their work to ensure the depth and volume of vision, are under the control of the oculomotor, abducens and trochlear nerves. The width of the palpebral fissure is controlled by the facial nerve.
The muscles of the pupil itself are controlled by nerve fibers in the autonomic nervous system.
Secretory fibers located in the facial nerve regulate the functions of the lacrimal gland of the organ of vision.
Innervation of the eyeball
All nerves involved in the functioning of the eye originate in groups of nerve cells localized in the brain and nerve ganglia. The task of the nervous system of the eye is to regulate muscle function, ensure sensitivity of the eyeball, and the auxiliary apparatus of the eye. In addition, it regulates metabolic reactions and blood vessel tone.
The innervation of the eye involves 5 pairs of 12 available cranial nerves: oculomotor, facial, trigeminal, as well as abducens and trochlear.
The oculomotor nerve originates from nerve cells in the brain and has a close connection with the nerve cells of the abducens and trochlear nerves, as well as the auditory and facial nerves. In addition, there is its connection with the spinal cord, providing a coordinated reaction of the eyes, torso and head in response to auditory and visual stimuli or changes in the position of the torso.
The oculomotor nerve enters the orbit through the opening of the superior orbital fissure. Its role is to raise the upper eyelid, ensuring the work of the internal, superior, inferior rectus muscles, as well as the inferior oblique muscle. Also, the oculomotor nerve includes branches that regulate the activity of the ciliary muscle and the work of the pupillary sphincter.
Together with the oculomotor nerve, 2 more nerves enter the orbit through the opening of the superior orbital fissure: the trochlear nerve and the abducens nerve. Their task is to innervate, respectively, the superior oblique and external rectus muscles.
The facial nerve contains motor nerve fibers, as well as branches that regulate the activity of the lacrimal gland. It regulates the facial movements of the facial muscles and the work of the orbicularis oculi muscle.
The function of the trigeminal nerve is mixed; it regulates muscle function, is responsible for sensitivity and includes autonomic nerve fibers. In accordance with its name, the trigeminal nerve splits into three large branches.
The first main branch of the trigeminal nerve is the ophthalmic nerve. Passing into the orbit through the opening of the superior orbital fissure, the optic nerve gives rise to three main nerves: nasociliary, frontal and lacrimal.
The nasolacrimal nerve passes through the muscular funnel, in turn dividing into ethmoidal (anterior and posterior), long ciliary, and nasal branches. It also gives off a connecting branch to the ciliary ganglion.
The ethmoidal nerves are involved in providing sensitivity to cells in the ethmoidal labyrinth, the nasal cavity, and the skin of the tip of the nose and its wings.
The long ciliary nerves lie in the sclera in the area of the optic nerve. Then their path continues in the supravascular space in the direction of the anterior segment of the eye, where they and the short ciliary nerves extending from the ciliary ganglion create a nerve plexus around the circumference of the cornea and the ciliary body. This nerve plexus regulates metabolic processes and provides sensitivity to the anterior segment of the eye. Also, the long ciliary nerves include sympathetic nerve fibers that branch from the nerve plexus belonging to the internal carotid artery. They regulate the activity of the pupillary dilator.
The short ciliary nerves begin in the region of the ciliary ganglion; they run through the sclera, surrounding the optic nerve. Their role is to ensure nervous regulation of the choroid. The ciliary ganglion, also called the ciliary ganglion, is a union of nerve cells that take part in the sensory (via the nasociliary root), motor (via the oculomotor root), and also the autonomic (via sympathetic nerve fibers) direct innervation of the eye. The ciliary ganglion is localized at a distance of 7 mm posterior to the eyeball below the external rectus muscle, in contact with the optic nerve. At the same time, the ciliary nerves jointly regulate the activity of the pupillary sphincter and dilator, providing special sensitivity to the cornea, iris, and ciliary body. They maintain the tone of blood vessels and regulate metabolic processes. The subtrochlear nerve is considered the last branch of the nasociliary nerve; it is involved in the sensitive innervation of the skin of the root of the nose, as well as the inner corner of the eyelids, part of the conjunctiva of the eye.
Entering the orbit, the frontal nerve splits into two branches: the supraorbital nerve and the supratrochlear nerve. These nerves provide sensitivity to the skin of the forehead and the middle zone of the upper eyelid.
The lacrimal nerve, at the entrance to the orbit, splits into two branches - upper and lower. At the same time, the upper branch is responsible for the nervous regulation of the lacrimal gland, as well as the sensitivity of the conjunctiva. At the same time, it provides innervation to the skin of the outer corner of the eye, covering the area of the upper eyelid. The inferior branch unites with the zygomaticotemporal nerve, a branch of the zygomatic nerve, and provides sensation to the skin of the cheekbone.
The second branch becomes the maxillary nerve and is divided into two main lines - the infraorbital and zygomatic. They innervate the auxiliary organs of the eye: the middle of the lower eyelid, the lower half of the lacrimal sac, the upper half of the lacrimal duct, the skin of the forehead and zygomatic region.
The last, third branch, having separated from the trigeminal nerve, does not take part in the innervation of the eye.
Neuropathy of the buccal nerve.
The causes of the disease can be periostitis, inflammatory diseases of the teeth and gums, traumatic removal of teeth in the lower jaw.
Clinic.
The pain occurs subacutely, is constant, and its intensity gradually increases. First it occurs on the front surface of the gum, transitional fold, and then spreads to the entire front surface of the teeth of the lower jaw and covers the entire area of innervation of the buccal nerve. Numbness is uncharacteristic; an objective examination reveals a decrease in all types of sensitivity in the area of innervation of the mucous membrane of the cheek and vestibular surface of the gums, as well as the skin of the corner of the mouth.
Main functions
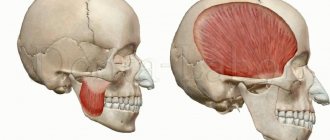
The trigeminal nerve is the most sensitive nerve in the face and mouth. It also contains motor tissues responsible for the innervation of the masticatory muscles. Has two sensors:
- The superficial nucleus of the trigeminal nerve, responsible for pain and tactile sensitivity.
- Deep nucleus (proprioceptive), responsible for the perception of free receptors.
Its motor part originates from the motor nucleus. Sensitive tissues are branched processes of neurons of the Gasserian ganglion. Nerve impulses depart from them to nerve cells embedded in the substance of the secreted part of the third brain, which continues the spinal cord.
The superficial nucleus is a continuation of sections of the spinal cord that look like horns. It runs through the medullary pons and bulb of the brain, and also covers the two upper cervical spinal segments.
The deep nucleus is located in the dorsal part of the pontine tegmentum. Receiving sensitive impulses from touch and pressure, it conducts them along the spinal cord through the posterior cords.
The motor nucleus is located in the middle of the deep nucleus. Its impulses exit near the sensory root, connecting with the mandibular nerve, innervating the facial and digastric muscles.
The layout and structure of the trigeminal nerve allows it to perform several important functions for the body:
- provide deep and superficial sensitivity of the eyes, mouth, nose, brain;
- responsible for the motor ability of the head muscles (temporal, chewing).
The trigeminal nerve perceives any touch, including pain, and transmits a sensory signal from the elements eaten or exhaled.
Causes of inflammation
The installation of a dental implant should be carried out taking into account the parameters of the jaw, size, characteristics of the alveolar process and bone tissue of the implanted area. The relief of the canal through which the mandibular nerve bundle passes must be thoroughly studied.
Lack of preparation for implantation and lack of professionalism are the main causes of damage to the mandibular branch.
You can touch or damage the neurovascular bundle:
- needle during anesthesia;
- direct pressure with a long implant;
- tool when forming a dental bed.
Damaging factors include a long period of flap retraction and bone graft harvesting. Restoring sensitivity is a long and problematic process; the task of implantologists is to reduce potential risks to a minimum .
Diagnosis and prevention of pathologies
When alarming symptoms appear, the doctor collects anamnesis, listens to the patient’s complaints, and conducts a visual examination. Next, he probes the exit points of the trigeminal nerve branches, assessing the degree of their sensitivity and pain. If triggers are identified, a preliminary diagnosis is made, which is confirmed using computed tomography and magnetic resonance imaging. These examinations make it possible to exclude the presence of other pathologies, as well as to detect vascular compression of the trigeminal nerve roots.
There are no specific preventive measures for trigeminal nerve diseases. Experts advise strengthening the immune system, treating infectious diseases in a timely manner, and not overcooling, especially in the summer, sitting under fans and air conditioners.
Neuropathy of the superior alveolar nerve.
The causes of the disease may be chronic pulpitis and periodontitis, nerve damage in case of complex tooth extraction, sinusitis, and surgical intervention for sinusitis.
It manifests itself as pain and a feeling of numbness in the teeth of the upper jaw. Objectively, there is a decrease or absence of sensitivity in the gum area of the upper jaw, as well as the adjacent area of the buccal mucosa. The electrical excitability of the pulp in the corresponding teeth of the upper jaw is reduced or absent.
If the cause of the disease is stenosis of the infraorbital canal, then patients will complain of pain and numbness of the skin in the area of innervation of the infraorbital nerve (wing of the nose, area above the canine fossa, upper lip).
Complications and treatment
Facial asymmetry is one of the possible complications.
Chronic diseases develop with untimely or illiterate treatment of neuralgia and neuritis. As a result, dangerous complications are diagnosed, leading to the following pathologies:
- muscle atrophy;
- decreased sensitivity of the skin, mouth, and nasal cavity;
- facial asymmetry;
- violation of diction;
- deterioration of hearing and vision acuity.
Inflammatory and non-inflammatory processes affecting TN require complex therapy with the use of medications, physiotherapy sessions, and massage. Pharmacological agents include nonsteroidal anti-inflammatory drugs, muscle relaxants, anticonvulsants together with Novocaine blockades, antispasmodics, and sedative tablets.
If traditional therapy does not help, they resort to radiofrequency and microvascular destruction, which causes virtually no complications. In severe cases, surgical intervention is used through microvascular decompression with the placement of a special “protector” between the nerve and the vessel, which helps protect the nerve fibers from clamping and further damage.
Anatomical structure
The character of TN is mixed. At the base of the brain structures, emerging from the thickness of the bridge with sensitive and motor roots, it is directed forward and slightly to the side, penetrating into the cleft of the dura mater. The sensitive root forms the trigeminal cavity, in which a fairly long ganglion (Gasserian ganglion) lies. The concave part is placed back, and the convex part is placed forward.
From the convex edge, which is located in front, there are three main branches: the ophthalmic, maxillary and non-maxillary nerves. On the inside, the node goes around the motor root, heading towards the cranial foramen ovale. There it reunites with the third branch of TN.