Pharmacokinetics
Metabolized to form the main metabolite 4N-methylaminoantipyrine (MAA) and other metabolites - 4N-aminoantipyrine (AA), 4N-acetylaminoantipyrine (AAA) and 4N-formylaminoantipyrine (FAA).
Metabolites AAA and PAA do not have pharmacological activity. All metabolites have nonlinear pharmacokinetics; with short-term use, the accumulation of metabolites does not play a big role. Plasma protein binding is 58% for MAA, 48% for AA, 18% for FAA, and 14% for AAA.
Metamizole sodium crosses the placenta. Metamizole sodium metabolites pass into breast milk. Approximately 96% is excreted by the kidneys in the form of metabolites. After intravenous administration, the half-life of metamizole sodium is 14 minutes.
When high doses of metamizole sodium are administered, the kidneys may excrete a metabolite, rubazonic acid, which can turn urine red.
Elderly
In elderly patients, the area under the concentration-time curve increases by 2-3 times.
Liver dysfunction
In patients with liver cirrhosis, the half-life of MAA and FAA with a single dose of the drug increases approximately 3 times, the half-life of AA and AAA does not change. In such patients, high doses should be avoided.
Renal dysfunction
In renal failure, the rate of elimination of some metabolites (AAA and FAA) is reduced. In such patients, high doses should be avoided.
Pharmacological properties
Pharmacodynamics.
NSAIDs, pyrazolone derivative. non-selectively blocks cog, reduces the formation of prostaglandins from arachidonic acid. prevents the conduction of painful extra- and proprioceptive impulses along the Gaulle and Burdach fascicles, increases the threshold of excitability of the thalamic centers of pain sensitivity, and increases heat transfer. A distinctive feature is the insignificant severity of the anti-inflammatory effect, which causes a weak effect on water-salt metabolism (retention of na+ and water) and the gastrointestinal mucosa. has an analgesic, antipyretic and some antispasmodic (in relation to the smooth muscles of the urinary and biliary tract) effect. Pharmacokinetics. When administered intramuscularly, it is quickly and completely absorbed into the blood. In the liver it undergoes oxidative deamination to form an active metabolite. The connection of the active metabolite with proteins is 50–60%. In children, deamination processes occur more slowly than in adults. With frequent administration (more than 4 times a day), drug accumulation and intoxication are possible in children. Quickly and evenly distributed in tissues. Cmax is achieved 1–1.5 hours after IM administration. T½ is about 7 hours. It is excreted in the urine.
When administered orally, it is quickly absorbed into the gastrointestinal tract. In the intestinal wall it is hydrolyzed to form an active metabolite. It is not found in the blood unchanged. The active metabolite is 50–60% bound to plasma proteins. The time to reach Cmax in blood plasma is 1–2 hours. T½ is 2.5 hours. It is excreted mainly by the kidneys.
Contraindications
- hypersensitivity to pyrazolone derivatives (propyphenazone, phenazone or phenylbutazone);
- bronchial asthma induced by taking acetylsalicylic acid, salicylates or other non-steroidal anti-inflammatory drugs (NSAIDs);
— bronchial obstruction, rhinitis, urticaria, provoked by taking acetylsalicylic acid or other NSAIDs (including a history);
— condition after coronary artery bypass grafting;
- inhibition of hematopoiesis (agranulocytosis, cytostatic or infectious neutropenia);
- acute renal or liver failure;
- acute intermittent hepatic porphyria;
- confirmed hyperkalemia;
- erosive and ulcerative changes in the mucous membrane of the stomach and duodenum, active gastrointestinal bleeding, inflammatory bowel diseases;
- anemia, leukopenia;
- hereditary hemolytic anemia associated with deficiency of glucose-6-phosphate dehydrogenase;
— pregnancy (I and III trimester), breastfeeding period;
— infancy (up to 3 months with body weight less than 5 kg);
- for intravenous administration - children up to 12 months (body weight up to 9 kg).
Carefully
Arterial hypotension (systolic blood pressure (BP) below 100 mm Hg); decrease in circulating blood volume (CBV); hemodynamic instability (myocardial infarction, multiple trauma, incipient shock); incipient heart failure; high fever (increased risk of a sharp decrease in blood pressure).
Diseases in which a significant decrease in blood pressure may be of increased danger (severe coronary heart disease, stenosis of cerebral arteries).
Chronic alcohol abuse.
Bronchial asthma, especially in combination with concomitant polypous rhinosinusitis; chronic urticaria and other types of atopy (allergic diseases, in the development of which a significant role is played by a hereditary predisposition to sensitization: hay fever, allergic rhinitis, etc.) (increased risk of developing anaphylactic/anaphylactoid reactions).
Alcohol intolerance (reaction to even small amounts of certain alcoholic beverages in the form of itching, watery eyes and severe redness of the face) (increased risk of developing anaphylactic/anaphylactoid reactions).
Intolerance or hypersensitivity to dyes (eg, tartrazine) or preservatives (eg, benzoate) (increased risk of anaphylactic/anaphylactoid reactions).
Severe impairment of liver and kidney function (the use of low doses is recommended due to the possibility of slowing the rate of excretion of metamizole sodium).
Pregnancy (II trimester).
Use during pregnancy and breastfeeding
Pregnancy
Metamizole sodium penetrates the placental barrier. Data on the use of metamizole sodium during pregnancy are limited. Since there are no adequate data on use in humans, metamizole sodium should not be used in the first trimester of pregnancy; in the second trimester of pregnancy, the drug can be used if the expected benefit to the mother outweighs the potential risk to the fetus. Despite the fact that metamizole sodium weakly inhibits the synthesis of prostaglandins, the possibility of premature (intrauterine) closure of the ductus arteriosus, as well as perinatal complications caused by impaired platelet aggregation in the mother or newborn cannot be excluded. In this regard, metamizole sodium is contraindicated in the third trimester of pregnancy.
Breastfeeding period
Metamizole sodium metabolites pass into breast milk, therefore, when using the drug, as well as within 48 hours after taking the last dose, breastfeeding should be stopped.
special instructions
In patients receiving cytotoxic drugs, as well as in children under 5 years of age, the use of metamizole sodium should only be carried out under medical supervision.
Anaphylactic/anaphylactoid reactions
When choosing a method of drug administration, it should be taken into account that parenteral administration is associated with a higher risk of anaphylactic/anaphylactoid reactions. An increased risk of developing hypersensitivity reactions to metamizole sodium may be due to the following conditions: - analgesic bronchial asthma, especially with concomitant polypous rhinosinusitis; - chronic urticaria; - alcohol intolerance (increased sensitivity to alcohol), against the background of which, even when taking a small amount of certain alcoholic beverages, patients experience sneezing, lacrimation and severe redness of the face.
Alcohol intolerance may indicate previously unidentified aspirin asthma syndrome; - intolerance or hypersensitivity to dyes (for example, tartrazine) or preservatives (for example, benzoate).
Before using metamizole sodium, it is necessary to conduct a thorough survey of the patient in order to determine medical history. If the risk of developing anaphylactic reactions is identified, use is possible only after a thorough assessment of the ratio of the expected benefit to the possible risk of using metamizole sodium.
In the case of using metamizole sodium in such patients, it is necessary to ensure the availability of funds to provide them with emergency assistance in the event of the development of anaphylactic/anaphylactoid reactions and strict medical monitoring of their condition.
Metamizole sodium should be used with caution in patients with asthma or atopy.
Patients who experience anaphylactoid reactions when using metamizole sodium are also at risk of developing them when using other non-narcotic analgesics/NSAIDs.
Patients who experience anaphylactic or other immune-mediated reactions (eg, agranulocytosis) in response to the use of metamizole sodium are also at risk of developing them when using other pyrazolones and pyrazolidines.
Severe skin reactions
Life-threatening skin reactions, such as Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), have been described with the use of metamizole sodium.
If symptoms of SJS and TEN appear, including a progressive skin rash, often with blisters or lesions of the mucous membrane, treatment with metamizole sodium should be stopped immediately and should not be continued in this category of patients. Patients should be aware of the symptoms of these skin reactions.
They should be carefully monitored for skin reactions, especially during the first days of treatment.
Agranulocytosis
With long-term use (more than 7 days), it is necessary to monitor the peripheral blood picture. With the use of metamizole sodium, agranulocytosis may develop. It occurs very rarely, lasts at least a week, is not dose-dependent, can be severe, life-threatening and, in some cases, fatal. Therefore, if you identify symptoms such as an unmotivated rise in temperature, chills, sore throat, difficulty swallowing, stomatitis, erosive and ulcerative lesions of the oral cavity, vaginitis or proctitis, a decrease in the number of neutrophils in the peripheral blood less than 1500/mm3, you must immediately contact See your doctor and stop taking the drug.
Pancytopenia
If pancytopenia develops, use of the drug should be stopped immediately, and complete blood count indicators should also be monitored until they return to normal. All patients should be aware that pathological changes in the blood during the use of metamizole sodium may be accompanied by the appearance of symptoms such as general malaise, infections, persistent fever, hematoma formation, bleeding, pale skin, which requires immediate consultation with a doctor.
Isolated hypotensive reactions
Metamizole sodium may cause isolated hypotensive reactions, which may be dose-dependent. The risk of reactions is increased with previous arterial hypotension, decreased blood volume or dehydration, unstable hemodynamics or acute circulatory disorders (for example, in patients with myocardial infarction or trauma), in patients with fever. Such patients should be assessed in detail and closely monitored.
In order to reduce the risk of developing hypotensive reactions, preventive measures (hemodynamic stabilization) may be required. In patients in whom blood pressure reduction should be avoided at all costs (for example, with severe coronary artery disease or significant cerebral artery stenosis), the drug can be used with careful monitoring of hemodynamic parameters.
Abdominal pain
It is unacceptable to use metamizole sodium to relieve acute abdominal pain (until the cause is determined).
Liver and kidney dysfunction
In patients with impaired liver or kidney function, it is recommended to avoid the use of metamizole sodium in high doses due to a decrease in its elimination rate. The drug contains sodium, which should be taken into account by people on a low sodium diet.
Rules for administering the drug
Intravenous administration should be carried out very slowly (no more than 1 ml per minute) in order to quickly stop the drug at the first signs of anaphylactic/anaphylactoid reactions and/or to minimize the occurrence of isolated hypotensive reactions.
For intramuscular administration, it is necessary to use a long intramuscular needle.
Impact on the ability to drive vehicles and machinery
Considering the profile of adverse reactions when using metamizole sodium, caution should be exercised when driving vehicles, machinery, as well as when performing work that requires increased concentration and speed of psychomotor reactions.
Note!
Description of the drug Analgin-Darnitsa solution d/in. 500mg/ml amp. 2ml No. 10 on this page is a simplified author’s version of the apteka911 website, created on the basis of the instructions for use.
Before purchasing or using the drug, you should consult your doctor and read the manufacturer's original instructions (attached to each package of the drug). Information about the drug is provided for informational purposes only and should not be used as a guide to self-medication. Only a doctor can decide to prescribe the drug, as well as determine the dose and methods of its use.
Directions for use and doses
Intravenously, intramuscularly deep into the muscle.
Parenteral administration of the drug is indicated only if it is impossible to take it orally. Before administration, it is recommended to warm the drug to body temperature.
Adults and adolescents over 15 years of age: 1.0-2.0 ml (500 mg/ml) of metamizole solution (intramuscular or intravenous) is recommended as a single dose. The maximum daily dose is 2000 mg, divided into 2-3 administrations per day. The maximum daily dose is 1000 mg.
For children aged 3-11 months (body weight more than 5 kg to 9 kg), the drug is administered only intramuscularly at a dose of 50-100 mg per 10 kg of body weight (0.1-0.2 ml of a 500 mg/ml solution). A single dose can be divided into 2-3 injections.
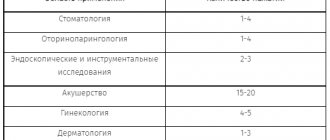
The following table contains recommended doses of the drug.
| Age (body weight) | Dose |
| Children 3-11 months (over 5 kg to 8 kg) Intramuscular administration only!!! | 0.1-0.2 ml (corresponding to 50-100 mg of metamizole) |
| Children 1-3 years old (approx. 9-15 kg) | 0.2-0.5 ml (corresponding to 100-250 mg of metamizole) |
| Children 4-6 years old (approx. 16-23 kg) | 0.3-0.8 ml (corresponding to 150-400 mg of metamizole) |
| Children 7-9 years old (about 24-30 kg) | 0.4-1.0 ml (corresponding to 200-500 mg of metamizole) |
| Children 10-12 years old (approx. 31-45 kg) | 0.5-1.0 ml (corresponding to 250-500 mg of metamizole) |
| Children 13-14 years old (approx. 46-53 kg) | 0.8-1.8 ml (corresponding to 400-900 mg of metamizole) |
| Adults and adolescents over 15 years of age (weighing more than 53 kg) | 1.0-2.0 ml (corresponding to 500-1000 mg of metamizole) |
Intravenous administration should be carried out very slowly (infusion rate no more than 1 ml/min) with the patient lying down, under blood pressure control. At the first signs of the development of anaphylactic/anaphylactoid reactions, it is necessary to stop administering the drug.
Since the hypotensive reactions are dose-dependent, parenteral administration of a dose of 1000 mg of metamizole should be carried out with extreme caution. If the drug is administered too quickly, a critical drop in blood pressure and shock may occur.
Elderly patients need to use lower dosages due to a possible decrease in the excretion of metamizole metabolites from the body. Patients in serious condition and with impaired creatinine clearance should use smaller doses due to a possible decrease in the excretion of metamizole metabolites from the body.
In patients with impaired liver and kidney function, the rate of elimination of the drug is slowed down, so repeated use of the drug should be avoided. There is no experience with long-term use. For short-term therapy, no dose adjustment is required.
When used as an analgesic, the duration of therapy is 1-5 days. When used as an antipyretic – 1-3 days.
Side effect
Adverse reactions are classified as follows according to the World Health Organization (WHO) classification: very common (>1/10), common (>1/100 to <1/10), uncommon (>1/1000 to <1/100), rare (>1/10000 to <1/1000), very rare (up to <1/10000) and frequency unknown (cannot be estimated from available data).
Immune system disorders
Rarely: anaphylactic or anaphylactoid reactions.
Very rare: analgesic bronchial asthma.
Frequency unknown: anaphylactic shock.
Metamizole sodium may cause anaphylactic or anaphylactoid reactions, which in very rare cases can be severe and life-threatening. They can occur even if metamizole sodium has been previously used many times without any complications. Such drug reactions may develop immediately or some time after using metamizole sodium, usually within one hour. In milder cases, reactions manifest themselves in the form of skin and mucous membrane symptoms (itching, burning, flushing, urticaria, swelling); shortness of breath or patient complaints of gastrointestinal symptoms. In severe cases, they develop into generalized urticaria, severe angioedema (especially involving the larynx), severe bronchospasm, cardiac arrhythmias, a sharp decrease in blood pressure (which is sometimes preceded by an increase in blood pressure) and the development of circulatory shock.
In persons with analgesic bronchial asthma syndrome and intolerance to analgesic drugs, these reactions usually manifest themselves in the form of attacks of bronchial asthma.
From the blood and lymphatic system
Rarely: leukopenia.
Very rare: agranulocytosis (including fatal cases), thrombocytopenia.
Frequency unknown: aplastic anemia, pancytopenia (including fatal cases).
These reactions are immunological and can occur even if metamizole sodium has been previously used many times without any complications. Typical symptoms of agranulocytosis are lesions of the mucous membranes (oral cavity and pharynx, anorectal area, genital organs), sore throat, fever. However, when antibiotics are used, these phenomena may be mild. Sometimes, but not always, there is a slight enlargement of the lymph nodes or spleen. The erythrocyte sedimentation rate increases significantly, the content of granulocytes is sharply reduced or not determined. As a rule, hemoglobin, red blood cells and platelets remain normal, but deviations may occur. Typical symptoms of thrombocytopenia are an increased tendency to bleeding and the appearance of petechiae on the skin and mucous membranes.
If there is an unexpected deterioration in the general condition, the fever does not go away or ulcerations appear on the mucous membranes, especially the oral cavity, nose, and larynx, treatment tactics involve immediate discontinuation of the drug without waiting for the results of laboratory tests.
If pancytopenia develops, metamizole sodium should be discontinued and a complete blood count should be monitored until its values return to normal (see section “Special Instructions”).
Heart disorders
Frequency unknown: Kounis syndrome (allergic coronary syndrome, manifested by clinical and laboratory signs of angina caused by inflammatory mediators).
Vascular disorders
Uncommon: isolated decrease in blood pressure.
An isolated transient decrease in blood pressure is possible (possibly pharmacologically caused, and not accompanied by other manifestations of anaphylactic/anaphylactoid reactions).
Rarely: a sharp pronounced decrease in blood pressure.
With fever, a dose-dependent sharp decrease in blood pressure without other signs of a hypersensitivity reaction is also possible.
Skin and subcutaneous tissue disorders
Uncommon: fixed drug dermatitis.
Rarely: skin rash.
Frequency unknown: Stevens-Johnson syndrome, toxic epidermal necrolysis (Lyell's syndrome).
From the kidneys and urinary tract
Very rare: renal dysfunction.
Frequency unknown: interstitial nephritis.
In very rare cases, patients with impaired renal function may experience an acute deterioration in renal function (acute renal failure), in some cases with oliguria, anuria, proteinuria.
General disorders
Uncommon: urine may turn red due to the presence of a metabolite in the urine - rubazonic acid.
Overdose
Symptoms: nausea, vomiting, abdominal pain, decreased renal function/acute renal failure with oliguria (for example, due to the development of interstitial nephritis), less common central nervous system symptoms (dizziness, drowsiness, tinnitus, delirium, impaired consciousness, convulsions, coma) and a sharp decrease in blood pressure (sometimes progressing to shock), as well as heart rhythm disturbances (tachycardia), hypothermia, shortness of breath, acute agranulocytosis, hemorrhagic syndrome, paralysis of the respiratory muscles. After high doses, renal excretion of a non-toxic metabolite (rubazonic acid) may cause urine to turn red.
Treatment: There is no specific antidote. In case of overdose, forced diuresis is indicated. The main metabolite (4N-methylaminoantipyrine) can be eliminated by hemodialysis, hemofiltration, hemoperfusion or plasma filtration. With the development of convulsive syndrome, intravenous administration of diazepam and fast-acting barbiturates is indicated.
Overdose
Symptoms: hypothermia, marked decrease in blood pressure, palpitations, shortness of breath, tinnitus, nausea, vomiting, gastralgia, weakness, oliguria, anuria, drowsiness, delirium, impaired consciousness, tachycardia, convulsive syndrome; the development of acute agranulocytosis, hemorrhagic syndrome, acute renal and liver failure, paralysis of the respiratory muscles is possible.
Treatment: induction of vomiting, gastric lavage, administration of saline laxatives, activated carbon. Carrying out forced diuresis, hemodialysis, blood alkalization, symptomatic therapy aimed at maintaining vital functions. When a convulsive syndrome develops, diazepam and fast-acting barbiturates are administered intravenously.
Interaction with other drugs
With cyclosporine: with simultaneous use, a decrease in the concentration of cyclosporine in the blood may be observed, therefore, when they are used together, monitoring of its concentration in the blood is required.
With other non-narcotic analgesics: simultaneous use of metamizole sodium can lead to mutual enhancement of toxic effects.
With tricyclic antidepressants, oral contraceptives, allopurinol: the drugs disrupt the metabolism of metamizole sodium in the liver and increase its toxicity.
With barbiturates, phenylbutazone and other inducers of microsomal liver enzymes: drugs weaken the effect of metamizole sodium.
With sedatives and tranquilizers: drugs enhance the analgesic effect of metamizole sodium. Concomitant use with chlorpromazine or other phenothiazine derivatives can lead to the development of severe hypothermia.
With drugs that are highly bound to plasma proteins (oral hypoglycemic drugs, indirect anticoagulants, glucocorticosteroids (GCS) and indomethacin): metamizole sodium, displacing oral hypoglycemic drugs, indirect anticoagulants, GCS and indomethacin from its connection with plasma proteins, increases their activity .
With myelotoxic drugs: drugs increase the manifestations of hematotoxicity of metamizole sodium.
With methotrexate: simultaneous use of metamizole sodium with methotrexate may enhance the hematotoxic effect of methotrexate, especially in elderly patients. It is recommended to avoid simultaneous use.
With thiamazole and sarcolysine: the risk of developing leukopenia increases.
With radiocontrast agents, colloidal blood substitutes and penicillin: due to the increased risk of anaphylactic/anaphylactoid reactions, they should not be used in conjunction with metamizole sodium.
With codeine, propranolol, H2-histamine receptor blockers: drugs enhance the effect of metamizole sodium.
With acetylsalicylic acid: with simultaneous use, metamizole sodium can reduce the effect of acetylsalicylic acid on platelet aggregation. This combination should be used with caution in patients taking low doses of acetylsalicylic acid as an antiplatelet agent.
With bupropion: Metamizole sodium may reduce the concentration of bupropion in the blood, which should be taken into account when using them simultaneously.
Due to the high probability of pharmaceutical incompatibility, metamizole sodium should not be mixed with other drugs in the same syringe.