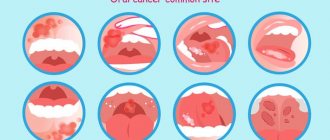
Stomatitis can be recognized by multiple ulcers on the gums, tongue, palate, inner cheeks and lips. It all starts with redness, which is accompanied by a burning sensation or a slight tingling sensation, and only after that, in places where pathogens are most concentrated, an ulcer forms. As a rule, it is shallow, and nevertheless, at the slightest irritation - while eating or brushing teeth - it makes itself felt with severe pain. But don’t despair; with proper treatment, stomatitis can be defeated in 4-5 days. Chlorhexidine for stomatitis is one of the mouth rinses recommended by all doctors.
Where do bacteria come from in the mouth and how to fight them?
Whatever the type of stomatitis (and there are quite a few varieties of it - aphthous, allergic, herpetic, ulcerative), it is always accompanied by the active proliferation of bacteria or viruses on the mucous membrane. Do you think they come from outside, from dirty hands and unwashed fruit? But it turns out that even an absolutely healthy person’s mouth is always full of spirochetes, fungi, staphylococci, streptococci and other “cocci.” These cultures constantly interact and restrain the excessive development of one of their friendly company. This balance is also maintained by saliva, which allows the microflora to exist more or less normally, but not to multiply too actively. This is the normal microflora of the oral cavity, the task of which is to destroy “foreign” bacteria that enter the mouth from the outside.
And then overnight the balance of microorganisms is disrupted. There are too many of some, too few of others. This is stomatitis. It is not difficult to destroy harmony. This can be caused by many factors and is not always due to dirty hands or unwashed food. Inflammation of the mucous membrane can occur due to:
- colds;
- stress;
- injuries;
- taking antibiotics;
- hormonal surge;
- dehydration of the body, and, consequently, a significant decrease in the amount of saliva.
The presence of hard-to-reach places in the mouth that are difficult to penetrate with a toothbrush also significantly increases the risk of developing stomatitis. Carious cavities, gum pockets, leaky crowns - all these are ideal conditions for bacteria. You can’t get them there, so they begin to multiply beyond measure. The more tartar and plaque in your mouth, the higher the likelihood that you will sooner or later face the need to treat painful ulcers.
Precisely because with stomatitis you have to “tame” overly active bacteria, one of the mandatory components of treatment is an antiseptic. It doesn't have to be chlorhexidine. But since it is the most accessible and cheap, most often patients prefer to rinse their mouths with it. The essence of its action is simple: it penetrates inside the bacterial cell and prevents it from consuming oxygen, which naturally causes it to die immediately.
Prevention of stomatitis in children
- Be sure to clean all cutlery, bottle and pacifier. Boil periodically.
- You need to brush your baby teeth 2 times a day. Cleaning should be carried out by parents up to 6 years of age, and then show all the movements to the child and teach him proper oral hygiene.
- After eating food, you need to rinse your mouth with boiled or filtered water that is well removed from bacteria.
- Wash your hands and all toys regularly. Children often put their fingers or toys in their mouths - wean them off this (many pathogenic bacteria get into the mucous membranes).
- Visit your dentist 2 times a year for a visual examination and disease prevention.
- Do not give your child too hot or cold food. Avoid hard, spicy, sour and very salty foods. This will lead to injury to the oral mucosa.
- Avoid foods that cause allergies.
- Provide a healthy diet rich in minerals and vitamins. It is advisable to walk outdoors more often. All this helps strengthen the immune system and protect against stomatitis.
Which chlorhexidine to buy and how to prepare the solution?
Chlorhexidine is an aqueous solution of chlorhexidine digluconate. When you go to the pharmacy, you can see containers with different numbers on the label - 0.05%, 0.1%, 1%, 5% and 20%. They indicate the concentration of the active substance in the solution. For mouth and throat rinses, 0.05% chlorhexidine is always used. If you buy just this one, then you won’t need to breed anything. But if you have a 20% solution on hand, that’s not a problem either. 2 milliliters of concentrated solution per liter of warm boiled water - that’s 0.05% chlorhexidine.
Note! There is also an alcohol solution of chlorhexidine on sale, but under no circumstances should you rinse your mouth with it. This is a technical antiseptic that is most often used to disinfect medical instruments and hospital premises.
Interestingly, chlorhexidine bigluconate can be sold under different names. For example, dentists often prescribe Corsodil to their patients. This is the same solution, only produced and packaged abroad. Because of this, its price is exactly 10 times higher than its domestic analogue! Does this mean that with its help it will be possible to deal with bacteria faster and more effectively? Not at all.
Properties used
Chlorhexidine is a drug that is not endowed with a specific taste and smell, does not leave marks on the skin, does not cause pain when it comes into contact with the surface of wounds, does not provoke the formation of scars and promotes tissue regeneration, extremely rarely, it can cause irritation and allergic reactions. These properties of the 0.05% solution, combined with a wide spectrum of action, distinguish it favorably from the most common means used for disinfection:
- iodine;
- brilliant green;
- hydrogen peroxide;
- alcohol and acid solutions,
as well as other common antiseptic agents.
How to rinse your mouth with chlorhexidine for stomatitis?
Chlorhexidine for stomatitis is used in a course, the maximum duration of which is 10 days. All this time, rinsing should be given for two minutes in the morning and evening. It is better to do the treatment after breakfast and dinner, since the antiseptic needs time to act, and for this you will have to give up eating for at least 2 hours.
The scheme is not complicated: we had breakfast, brushed our teeth properly, rinsed our mouth with water again to get rid of any remaining toothpaste - some of its components can reduce the effectiveness of the drug, and started treating the mouth with an antiseptic. To do this, you need to take a small amount of 0.05% chlorhexidine solution into your mouth and rinse for at least a minute. This is an important condition, because only with prolonged rinsing does chlorhexidine bigluconate form a thin film on the surface of the mucous membrane, which will fight bacteria for several more hours. In the evening, the procedure must be repeated.
Note! Accidental ingestion of even a weak solution is fraught with serious consequences. If this happens, you should immediately rinse your stomach and consult a doctor.
It is for this reason that chlorhexidine is rarely prescribed for rinsing for childhood stomatitis - the risk of accidental ingestion is too high. However, for these purposes the drug is released in the form of a spray. It can be sprayed onto any areas of the mucous membrane where there are aphthae and inflammation, but you should avoid contact directly with the throat or tonsils.
As for pregnant and lactating women, the drug poses no danger to them. Chlorhexidine is not absorbed into the blood and is concentrated exclusively on the surface of the mucosa, which means it can be used by this group of patients without restrictions.
Nevertheless, the duration of the standard course of treatment - 10 days - of course, cannot be exceeded by anyone. There is a temporary limitation in the use of antiseptics for a reason. By suppressing the proliferation of some bacteria for too long and intensively, we thereby promote the growth of others, in particular the Candida fungus. Many women are familiar with it firsthand - the same fungus provokes thrush. Getting rid of it is not easy, and if the same infection settles in the mouth, a lot of unpleasant sensations are guaranteed.
It happens that the need for antiseptics does not disappear even after 10 days from the date of start of treatment, in which case you can choose a mouthwash based on extracts of medicinal plants that has a mild anti-inflammatory effect.
Treatment of stomatitis in a child
The main rule is to immediately contact a specialist and not use any gels or ointments based on recommendations from the Internet. Each type of pathology is treated differently, so the dentist conducts a comprehensive examination. Additional consultation with an otolaryngologist or dermatologist is often required.
In complex therapy, proper oral care is prescribed and professional toothpaste is selected. Solutions and gels are required. If the form is viral, then antibiotics are used, and if it is allergic, then antihistamines are used. If necessary, medications are used to reduce the temperature (if there is fever and chills).
Advantages and disadvantages of the drug
Due to its high antimicrobial activity, chlorhexidine is often used in dentistry. It is cheap and effective - these are its main advantages. But the coin also has a downside. In addition to the fact that rinsing is unlikely to give the patient a pleasant sensation (the solution has a pronounced bitter taste), they can also stain the teeth and tongue brown.
The fact is that blackening is a reaction of microbes to the active substance. Where the accumulation of microorganisms is most abundant, dark spots appear. However, you can easily get rid of them by making an appointment with your dentist for tartar cleaning. But even if this is not done, after a few days after completing the course of rinsing, the darkening will go away on its own.
It must be said that not all dentists prescribe chlorhexidine for stomatitis. Some doctors generally believe that the effectiveness of this drug in the treatment of ulcerative inflammation of the mucous membrane is zero. They argue their position by the fact that 9 out of 10 stomatitis are caused not by bacteria, but by viruses, in particular herpes viruses. And if chlorhexidine fights microbes with a bang, then it is practically powerless against viruses.
Of course, there is also an aphthous form of the disease, but it is usually the result of a local allergic reaction, vitamin deficiency or injury (burn, scratch, cut), and therefore it is not treated with antiseptics. They can be used for only one purpose - to prevent bacterial infection from joining the foci of erosions and ulcers. If we are talking about the herpetic form of stomatitis, then it is appropriate to use another antiseptic - Miramistin, which can affect not only bacteria, but also viruses.
So you shouldn’t place too much hope on recovery by doing just rinsing. Chlorhexidine is effective only as part of complex therapy and only after deposits of stones and plaque have been removed from the oral cavity. Treatment of stomatitis is often impossible without taking antihistamines and antifungals, and in some cases without antibiotics.
Dentists warn
By trying to suppress inflammation with an antiseptic, patients are doing themselves a disservice. Until the cause of the inflammation is determined and eliminated, it will develop one way or another, only with less pronounced symptoms. The result of such amateur efforts can be sad: when the patient does get to the doctor (and this is inevitable), the only way out of this situation may be the removal of loose teeth.
Note! Like any medical product, chlorhexidine has an expiration date. You cannot rinse your mouth with a solution that has been stored in your medicine cabinet for more than 2 years. Moreover, even if you are sure of the date, make sure that all this time the packaging was stored correctly (at a temperature not exceeding 25 degrees) and was not exposed to direct sunlight.
Symptoms of stomatitis
Signs of stomatitis in a child have a number of features characteristic of a particular type of disease.
Herpetic stomatitis in children is considered very common and usually manifests itself as follows:
- in the initial stage, the disease is confused with a cold due to increased body temperature, often runny nose and cough;
- the inflammatory process begins abruptly, manifested by headaches and pain in the mouth and muscles due to intoxication of the body;
- submandibular lymph nodes are enlarged and painful;
- feature - the formation of small bubbles filled with liquid.
Upon visual examination, redness of the gum tissue around the teeth, swelling of the mucous membrane and numerous vesicular rashes covered with a yellowish or whitish coating are noted. Candidal stomatitis in children can be clinically acute or mild. In this case, signs of stomatitis in a child appear as follows:
- very rarely an increase in temperature is recorded;
- in the oral cavity there are affected areas covered with a coating of cottage cheese;
- children behave restlessly, are capricious, refuse to eat;
- Locally similar stomatitis in children (or thrush, as it is often called) occurs on the tongue, cheeks, gums and inner lips).
Aphthous stomatitis in children is the most common form of the disease, but also difficult to treat due to the difficulty of identifying the specific pathogen. Similar stomatitis in children, the symptoms of which are more common in schoolchildren than in the younger age group, is characterized by the following symptoms:
- rash of single ulcers (feed) on the mucous membrane (on the cheeks, in the area of the tongue and the inside of the lips);
- Initially, such stomatitis in children in the mouth is manifested by characteristic redness, itching, burning, and an increase in temperature is also noted.
In this case, the ulcers do not look like blisters, but are whitish ulcers with a bright red outline around them. Then the ulcers are usually covered with a cloudy film, which can break through and cause a secondary infection, after which the baby’s condition will only worsen. Parents should know that stomatitis in a child is not a single type of infection with specific symptoms.
Each form of this inflammatory process has its own specific symptoms and causes. That is why, despite a number of individual similar points (temperature during stomatitis in a child, signs of inflammation of the mucous membrane, enlarged lymph nodes), the problem of treating stomatitis in a child is solved differently, taking into account the form of the disease.
When else is chlorhexidine used for teeth?
After tooth extraction
Stomatitis is not the only reason to resort to the help of an antiseptic. Its antimicrobial properties can be very useful after a complex tooth extraction. Especially if the surgical intervention took place against the background of inflammation or not all deposits of tartar and caries have been removed from the oral cavity. To prevent the infection from seeping into the hole formed at the site of the removed molar and causing the blood clot there to suppurate, the surgeon may recommend an antiseptic.
How to rinse your mouth with chlorhexidine after tooth extraction? Not too active and not too long. Simply hold the solution in your mouth for 20-30 seconds. The main thing is to prevent a blood clot from falling out of the hole. Then repeated bleeding may begin and the risk of inflammation will be too high.
In this case, we may be talking about another diagnosis - alveolitis. It also involves rinsing with an antiseptic, but only after the inflamed contents of the hole have been thoroughly cleaned of necrotic residues, washed and treated with a medicinal solution. All these manipulations are carried out by a surgeon and only he can give recommendations on further rinsing with chlorhexidine.
During teething
Chlorhexidine digluconate solution is often indispensable in dental practice. Thus, it helps relieve inflammation that occurs when wisdom teeth erupt. Until it is completely above the surface of the gum, some part of the molar is covered by the so-called “hood” - part of the mucous membrane that lies on the chewing surface. The space between the tooth and the hood is a favorite place for bacteria. It's warm, humid, and full of food debris that you can't reach with a toothbrush. It is not surprising that the mucous membrane becomes inflamed, swollen, and in some cases even purulent discharge is observed. Regular thorough rinsing with an antiseptic, as a rule, copes with this problem once or twice, and yet this is not a reason to self-medicate. A consultation with a doctor is necessary at least to make sure that the inflamed hood does not require any other intervention.
With flux
You cannot do without rinsing your mouth with chlorcesidine even after installing a drainage, which often happens if you use a flux. An opened purulent abscess is a huge threat to the entire oral cavity. This is a real source of microbes and bacteria that can spread a purulent infection not only throughout the entire mucous membrane, but also reach the tonsils. In this case, rinsing with chlorhexidine should be done very carefully so that the drainage does not fall out. It is enough to put the solution in your mouth and hold it there for half a minute.
For bleeding gums
An antiseptic can also help in the treatment of inflammatory processes in the gums caused by accumulations of soft plaque and tartar. It will quickly deal with the bacteria remaining after professional teeth cleaning (without this, alas, nowhere, otherwise the effect of chlorhexidine will be short-lived and inflammation will soon begin with even greater force). In addition, various forms of gingivitis and periodontitis are perfectly treatable with the help of special chlorhexidine toothpastes.
As you can see, chlorhexidine solution in dentistry in general and for stomatitis in particular is an irreplaceable remedy. But it, like any potent medical drug, can cause serious harm to health if you do not adhere to strict rules for its use. By self-medicating, the balance of the microflora of the oral cavity can easily be disrupted, but it will definitely not be possible to restore it without the help of a dentist.
Sources used:
- Hygienic care for inflamed periodontal disease / S.B. Ulitovsky. - M.: MEDpress-inform, 2008.
- Etiology and pathogenesis of inflammatory periodontal diseases / E.V. Fomenko. — M.: Medical Information Agency (MIA), 2010
- Chlorhexidine. State register of medicines (May 26, 2016).