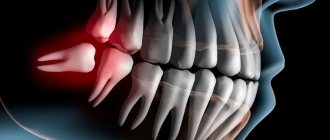
Our teeth do not forgive careless treatment. Advanced caries leads to pulpitis, and from there it is not far to tooth extraction. If you do not solve the problem of gaps in the dentition for a long time, then you will inevitably face an irreversible process of atrophy of the jaw bone.
What is this process and why does it happen? The human body operates according to a very simple principle: “he who does not work, does not eat.” If for any reason an organ stops functioning, the body stops supplying it with the necessary substances in full and the organ begins to atrophy (decrease in size).
The jawbone is no exception: while it is experiencing chewing load, the body diligently “feeds” it and maintains it in working condition. An extracted tooth deprives the jawbone of its normal work: immediately after the loss of a tooth, the bone begins to adapt to new circumstances.
The process of jaw bone atrophy can be divided into two stages. First, a thin strip of bone disappears, which was closest to the roots of the extracted tooth: such a restructuring takes one and a half to two months. It takes a few more months for the bone to heal. If after this stage you do not give the bone chewing load, the bone tissue begins to gradually dissolve further. The process of atrophy affects deeper and deeper layers. In a year of missing a tooth, the volume of the jawbone can decrease by up to 25%.
Tooth loss is the most common cause of bone loss, but it is far from the only one. Atrophy is also caused by:
- Inflammatory diseases of the mouth, such as periodontal disease, granulomas, and cysts;
- Deterioration of blood supply to the bone (this is affected by age-related changes, diseases of the cardiovascular system, endocrine pathologies);
- Various malocclusions and jaw injuries.
Prosthetics based only on gums (removable) or on living teeth (bridge) do not solve the problem: the jawbone under such dentures does not experience the necessary pressure and the process of bone tissue atrophy continues.
Classification of jaw atrophy and bone tissue phenotypes
Depending on the position of the jaw, there are two groups that characterize the atrophic state of the upper and lower jaws:
- According to Schroeder for the top row. There are three types of upper jaws with missing teeth, resulting in thinning bone tissue:
- The jaw tubercles are very noticeable. These gaps can be filled with prosthetic implants because the physical abnormalities are not noticeable. The palate is deep, and the bend of the mucosa is quite large.
- The alveolar processes are not clearly defined. The depth of the sky is average. Prosthetics are possible, but their fixation may deteriorate after muscle tissue overstrain.
- The bone at the base of the jaw is seriously destroyed. The ridges and tubercles of the alveoli are smooth, and the palate is transformed into a flat shape. The fold of the mucous membrane becomes at the level of the palate and does not hold its shape well. As a result of pathology, prosthetic structures cannot be secured.
- According to Keller for the bottom row:
- The alveolar elements are slightly smoothed, but are visible throughout the entire jaw. At the beginning of the alveolar ridge, muscle tissue and a fold of mucous membrane are attached. Installation of the prosthesis is not difficult.
- The ridge becomes noticeable and takes on a sharper shape. The muscles are attached to the crest. In most cases, the implant causes discomfort and pain.
- It is often observed in people who have undergone early removal of lateral teeth. The alveoli around the molars and premolars become thinner. In the central part, the bone tissue does not lose volume. Creating artificial teeth is possible, but there is a possibility of the implant slipping when chewing.
- In the area of the frontal incisors, a pronounced atrophic process is observed, while the lateral dentition remains preserved. Fixation of the prosthesis cannot be done, because the likelihood of its displacement increases.
Classic delayed load protocol
Classic surgery is performed when there is sufficient bone tissue (at least 10 mm) in two stages. The protocol involves delayed loading on the implants: they need time to fuse with the jaw.
An implant with dismountable elements (an abutment and an intraosseous part) is fixed using the method of detaching a gum flap - the gum is cut and sutured.
2-6 months after the operation, the implant is opened, a gum former is placed on it, and two weeks later - an abutment and an individual permanent prosthesis.
1
Implantation
Implantation
2
Prosthetics
Installation of a butterfly prosthesis or temporary crown (if it is possible to remove the bite)
4-6 months
Installation of abutment and permanent crown
Osteoplasty in case of a lack of tissue is organized before the implantation of titanium roots or simultaneously. The operation is justified for single defects. If the patient has multiple defects or complete edentia, classical surgery is difficult due to acute bone loss and the need to build up a large volume of bone.
If there is not enough bone tissue for implantation, classical implants in some clinics are implanted without tissue augmentation. The doctor suggests:
- install titanium roots only in the frontal zone (signs of atrophy rarely appear here);
- fix the implant in the area of the posterior wall of the maxillary sinus at the end of the dentition, behind the maxillary sinus (the height of the bone here reaches 20 mm);
- implant short and thin implants - implantation is possible in case of atrophy of the bone tissue of the lower jaw, without touching the jaw nerve.
But the described methods are unreliable: the risk of weak primary stability of the implant and its loosening cannot be excluded. The most reliable method in case of severe atrophy of bone tissue in the upper jaw can be pterygoid implants
ROOTT. These implants are longer than classic ones and are implanted into the zygomatic bone, bypassing the maxillary sinuses. Pterygoid implantation differs from zygomatic zygomatic implantation in its safety and low trauma.
When performing an operation, it is important to use implants from the same manufacturer (with the same impurities - metals in a titanium alloy). When fixing implants, impurity metals of different brands in the acidic environment of the oral cavity may not combine and cause allergies, galvanic syndrome, and rejection of titanium roots. The ROOTT implant system is unique: a range of implants from one manufacturer is used in all clinical cases.
Implantation for jaw bone atrophy
Several techniques are used to quickly restore the dentition. For example, installation of bridges or removable dentures. However, these methods cannot restore the required load on the bone, since the gums or healthy teeth are loaded.
Implantation helps relieve pressure on the bone and prevent further thinning.
In advanced cases, when the atrophy of the jaw bone tissue is significant, restoration of the bone structure is used before implantation. Various techniques are used, for example, sinus lifting, separation of the alveolar process, and the introduction of artificial tissue. Six months after the operation, implants are inserted. As a result, bone density and volume are preserved.
Implantation with immediate loading is considered a new technique. Special materials are installed not in the alveolar process, but in the basal part of the jaw. Thanks to this, the bone is immediately loaded, and the metabolism is not disrupted. Suitable only if three or more teeth in a row are missing.
Osteoplasty
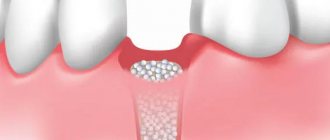
Classic dental implantation for bone tissue atrophy (height less than 10 mm) is preceded by bone augmentation surgery - osteoplasty. The procedure is carried out to ensure stable fixation of the implant and to avoid aesthetic complications during subsequent restoration of the element with prosthetics. For this purpose, the implantologist acts using one of the methods:
- Sinus lift.
The operation is performed on the upper jaw - the doctor lifts and displaces the maxillary sinus, making room for new bone. - Guided bone regeneration.
Bone material is added, covered with a membrane and sutured until it fuses with the jaw. - Replanting bone blocks.
The person's own bone material is used. It is removed from the lower jaw in the area of the wisdom teeth. The bone block is fixed with screws, bone granules are placed around it, and a membrane is attached. - Splitting of the alveolar ridge.
The dentist cuts the appendage and increases its thickness using a graft or artificial material.
It takes 3-6 months for the new bone to heal. It is possible to combine osteoplasty and implantation operations. The decision-making algorithm for performing osteoplasty simultaneously with implant fixation is as follows:
- Studying the possibility of positioning the artificial root in the correct position (using wax-up and surgical templates).
- Choice of osteoplasty technique. Depends on the degree of bone atrophy and its spread in height or width.
- If it is impossible to achieve stability of the artificial root with the existing bone volume, the extension is carried out in a separate stage.
Types and degrees of jaw bone atrophy
Deformation of the jaw bone develops with different intensity:
- I degree. At the beginning of the disease, it is eliminated by prosthetics. The implant performs its function, the blood supply is not disrupted.
- II degree. The clinical picture is intensifying. The mucous membrane of the jaw begins to shrink. Dental prosthetics are possible, but additional treatment is required before this can be done.
- III degree. The contour of the bone tissue is smoothed both on the inside of the mouth and on the side of the chin.
When selecting a treatment method, this characteristic of the development of pathology should be taken into account. Bone tissue decreases not only in height, but also in width. The bone becomes short and thin.
Tooth extraction is always accompanied by subsequent atrophy of both soft tissue and bone structures of the alveolar crest [4]. Clinically, this manifests itself as “recession of the gums” in the vertical and horizontal directions, mainly from the vestibular side; partial atrophy of the gingival papillae is often observed. This leads to a deterioration in the aesthetic result when carrying out further orthopedic or implantological treatment in the so-called aesthetically significant zone (zone of incisors, canines, premolars) [2].
There are risk factors that help predict possible aesthetic defects after tooth extraction: high smile line; thin gingival phenotype; pronounced pattern of the gingival margin with relatively high gingival papillae [3]. There is a group of patients with high aesthetic requirements, for whom the cosmetic result of treatment is more important than the functional one. Due to the increasing demands of patients for the cosmetic results of dental treatment in general and, in particular, for the restoration of lost teeth, the dental surgeon faces the difficult task of replenishing the lost volume of the gums and gingival papillae.
Correct prediction and planning of treatment after tooth extraction, assessment of risk factors from an aesthetic point of view, and the patient’s periodontal status can significantly improve the quality of subsequent orthopedic or implantological treatment.
Our proposed method for preventing atrophy of the gingival margin after tooth extraction allows us to avoid many of the indicated negative consequences of tooth extraction in an aesthetically significant area and improve the quality of treatment in general.
The indication for the use of the technique is the removal of teeth in an aesthetically significant area (the area of incisors, canines, premolars) as preparation for the upcoming fixed prosthetics or implant treatment.
Contraindications for using the technique: severe general somatic pathology that does not allow surgical treatment on an outpatient basis; allergic reactions to medications used; acute purulent inflammatory process in the area of the tooth being removed; general somatic pathology that reduces the general resistance of the body and the local regenerative properties of the soft tissues of the oral cavity (diabetes mellitus, condition after radiation or chemotherapy, blood diseases).
Relative contraindication: smoking; If the patient smokes about a pack of cigarettes a day or more, plastic periodontal surgery is not recommended due to a sharp deterioration in the healing processes in the oral cavity.
Logistics and technical support of the technique: surgical instruments: scalpel (No. 15 or microscalpel), raspatory, needle holder, surgical forceps, scissors, buccal retractor (micro instruments are preferred); binoculars with light; graduated periodontal probe; suture material "Vicryl" 6.0-7.0; hemostatic drugs (hydrogen peroxide, Katalugem); collagen hemostatic sponge.
Description of the technique
The essence of the technique is to transplant a free gum graft from the palate to the area of the mucosal defect above the socket of the extracted tooth in the area of the incisors, canines, and premolars. It is necessary to remove teeth in an atraumatic way without detachment of the mucoperiosteal flap, but only with separation of the circular ligament of the tooth. The main goal of surgery is to minimize trauma to the marginal gum of the tooth being removed in order to preserve its blood supply as much as possible. The traumatic nature of tooth extraction is directly related to the subsequent survival rate of the transplanted graft. After tooth extraction, it is necessary to examine the marginal gum. If granulation tissue is present, it is excised with a scalpel or periodontal scissors. If necessary, de-epithelialization of the gingival margin is carried out from the inside.
A free gingival graft is taken from the tissues of the hard palate, 5 mm away from the gum edge. Anesthesia of the palate is achieved by administering a local anesthetic with adrenaline 1:100,000. Adrenaline provides not only good local anesthesia, but also facilitates hemostasis during surgery. The site of choice is the gingival area distal to the anterior fold in the lateral palate. The donor area is limited to the distal surface of the crown of the first molar and the mesial surface of the first premolar (if necessary, the donor area can be expanded and enlarged in the anterior direction) [1, 5]. To increase the size of the ridge, it is recommended to use flaps of medium thickness (at least 1.5-2 mm). It should be noted that when cutting out a flap, the scalpel blade must be held perpendicular to the surface of the mucosa so that the base of the graft is the same diameter as its upper part. When taking a graft, a portion of the periosteum should be left in the donor area to avoid exposing areas of bone tissue. This reduces postoperative pain, accelerates healing time, which makes the postoperative period easier for the patient.
If excess glandular or adipose tissue is obtained during autograft harvesting, this may slow down the engraftment of the graft. The free autograft is placed on a napkin moistened with saline solution. The thickness of the graft is checked to ensure that the flap has a smooth and uniform surface. If necessary, while the graft is still on a damp cloth, a No. 15 scalpel can be used to remove fatty or glandular tissue. These manipulations must be carried out with extreme caution so as not to lead to excessive thinning or perforation of the graft. The wound on the palate can be left open; it heals by secondary intention. To ensure better hemostasis, a collagen hemostatic sponge is most often used, which is sutured to the edges of the wound with suture material (chrome-plated catgut, silk, vicryl, etc.).
After this, the graft is transferred into the oral cavity and its correct size and shape are checked. Giving it its final shape and the necessary correction is usually done using scissors outside the mouth and on a damp cloth. The finally formed autograft has the appearance of a “plug” for the socket of the extracted tooth; it must have a size and shape corresponding to the marginal gum of the socket. One of the signs of a correctly formed autograft is its independent retention in the socket after insertion. In this case, the edges of the graft should not turn under and it should not fall out of the socket. Fixation of the flap to the gum is carried out using regular interrupted sutures (5 sutures or more in a circle). Suturing is carried out without excessive tension; excessive compression of the marginal gum, accompanied by whitening of the tissue, should be avoided. This can lead to tissue necrosis and worsen the engraftment of the autograft. The thinnest possible suture material (6.0 or more) should be used. Suturing using magnifying optics is preferable to better align the gingival margins with the flap.
In the postoperative period, the patient is prescribed a gentle diet, antiseptic rinses (chlorhexidine 0.05% or Miramistin) 3 times a day after meals. The sutures are removed on the 7-10th day.
Studies [2] have shown that revascularization of a transplanted autograft occurs on average after 14 days. During this period, it is necessary to install an orthopedic structure (in the case of planning a bridge) to form gingival papillae. We operated on 24 patients using this method.
Here is a clinical example.
Patient N
., 32 years old, it is planned to remove the 14th tooth due to multiple root perforations
(Fig. 1, see color insert)
.
Figure 1. Figure 1.
14th tooth to be removed. An atraumatic removal of the 14th tooth, a thorough inspection and curettage of the socket, and an inspection of the marginal gum for the presence of pathological tissues were performed. Using a graduated periodontal probe, the length and width of the socket were measured (Fig. 2, see color plate)
.
Rice.
2. Measuring the size of the mucosal defect using a graduated periodontal probe. On the donor area of the hard palate, the required dimensions of the proposed flap were noted and a free gum graft of the same length, width and shape as the socket of the extracted tooth was cut out. Next, the necessary correction of the autograft was made, and excess adipose and glandular tissue was removed. The graft was transferred into the oral cavity, placed in the socket, and its edges were compared with the gingival edge of the socket. Using binoculars, sutures were applied (suture material “Vicryl” 6.0) without tension (Fig. 3, see color plate)
.
Rice.
3. View of the socket after fixation of the autograft; the wound on the roof of the mouth is left open. In this case, the donor area of the palate is left open in the postoperative period. Hemostasis was stable. The wound healed by secondary intention.
On the 7th day, epithelization of the wound occurred, the sutures were removed (Fig. 4, see color insert)
.
Rice.
4. View of the socket on the 7th day after surgery; the wound is epithelized. The proposed technique is quite simple, effective, and can significantly improve the aesthetic performance of subsequent orthopedic or implant treatment. Recommended for use during outpatient surgery.
Jaw bone atrophy with age
One of the factors influencing the defect is age-related changes. As a rule, in patients over 60 years of age, atrophy is a common process. This is explained by the fact that the lack of minerals and cell nutrition affects metabolism and teeth fall out. The blood supply to bone tissue is disrupted and the required amount of oxygen is not supplied. This causes a change in pressure on the bone.
Schroeder classification
According to the Schroeder classification, there are 3 types or types of atrophy of the alveolar ridge of the upper jaw:
- good appearance and shape of the alveolar ridge of the jaw, the hard palate is high dome-shaped, the frenulum of the lips is located high,
- moderate type: the shape of the alveolar ridge is somewhat smoothed out and it becomes smaller, the hard palate becomes flatter, the frenulum of the lips moves lower in comparison with the norm,
- sharp: the alveolar ridge is very much smoothed out, the hard palate loses its dome-shaped appearance, the frenulum of the lips drops even lower - almost level with the ridge. When installing a conventional removable denture, the frenulum will tighten and displace the denture.
Jaw bone atrophy after tooth extraction
The most common cause of the disease is the loss of a tooth or dentition. A few months after extraction, if prosthetics are untimely, the process of reducing the jawbone begins due to pressure on the alveolar process. Within a year, the deformation can reach its maximum.
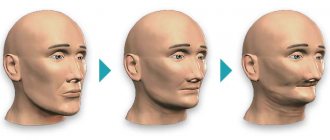
The consequences of bone tissue deficiency are expressed in the deterioration of speech, changes in the proportions of the face and its shape, and the appearance of severe wrinkles in the mouth area. At an advanced stage, patients experience displacement of the dentition, loss of opposite and/or adjacent teeth. Because of this, the likelihood of implantation failure increases.
Common causes and pathogenesis
Let's start with the fact that every organ of our body is constantly under load. When we do strength training, muscle performance increases. If we actively read books, study languages and gain new information, then our brain activity works and improves. It's the same with teeth. If they are present, the bone tissue and connective ligaments function naturally. When we chew, pressure is distributed onto the bone and triggers metabolic processes.
Now let's look at the pathogenesis, i.e. mechanism of occurrence of atrophy of the jaw bone tissue. It lies in the fact that after the tooth is removed (with the root), the chewing pressure that previously applied to this area disappears. The body ceases to consider this zone necessary and gradually “turns off” it from work. Blood vessels (capillaries) gradually atrophy, and nutrients and building substances cease to flow to the tissues. The bone decreases, shrinks and decreases in size, that is, it completely stops “working”. As a rule, this concerns the upper part of the alveolar process or the ridge of the jaw. They consist of a spongy bone layer that has a porous structure. It is in it that the alveoli (sockets) are located and the dental roots are fixed. Simultaneously with bone atrophy, the level of the gum decreases.
In general, the causes of bone tissue atrophy look like this:
- absence of teeth due to extraction or loss: physiological reason, which was described above,
- jaw trauma and serious bite pathologies,
- periodontitis – inflammation of the periodontium (periodontal tissues): atrophy of bone tissue during periodontitis occurs against the background of a large amount of tartar above and below the gums. It is inhabited by microbes that cause inflammation,
- diseases of the jaws – osteomyelitis (inflammation and necrosis of the bone), cysts (replace part of the bone tissue under the root of the tooth),
- wearing uncomfortable dentures that put a lot of pressure on the gums,
- metabolic disturbances, hormonal changes, systemic pathologies (including periodontal disease, osteoporosis, diabetes mellitus, HIV infection),
- aging of the body: characterized by a slowdown in metabolism,
- genetic predisposition,
- around the implant, bone tissue atrophy occurs due to improper implantation, jaw injuries, and poor oral hygiene (plaque forms, inflammation begins - peri-implantitis).
Consequences of a negative process
Adentia (lack of teeth) provokes a lot of problems, and atrophy of the jaw bone is not the only one of them. Destructive processes lead to the fact that with the loss of natural tissue volume, a person develops external changes in the contour of the face. This becomes especially noticeable if all teeth are missing: the number of facial wrinkles increases, lips and cheeks recede, asymmetry appears, visually a person looks older than his age, and sagging skin is noticeable.
A person experiences external changes in the facial contour
Health problems begin, the gastrointestinal tract suffers, and the clarity of pronunciation of sounds is impaired.
The most unpleasant thing is that even timely installed removable dentures and bridges do not save you from the problem. As the atrophic processes progress, they begin to cause more and more trouble: they no longer fit tightly to the gums and become displaced. Between the dentures and the mucous membrane, as a result of thinning of the bone tissue, a gap or gap is formed, into which food particles and bacteria penetrate, provoking the development of the inflammatory process. To get rid of these defects, patients often have to go to the correction of prostheses, buy adhesives and fixing creams.
There is another problem that atrophy leads to. If you have lost one or more units, and after a few years you decide to restore them with implantation, then difficulties will arise. Which? If there is insufficient bone volume, the implant cannot be securely fixed in it. He just won't hang in there. In addition, during the installation process, the doctor can injure nerves, touch the maxillary sinuses and adjacent areas. To avoid this, bone augmentation will have to be done before implantation. And this is a very costly and unpleasant manipulation that takes a lot of time. After it, you need to wait until the tissues heal, which usually takes 4-6 months.
Degree of development of pathology
Doctors distinguish four stages. In the first, the bone has a satisfactory volume, and if the patient wishes, the tooth can be restored without resorting to the procedure of increasing bone tissue during implantation. At the second stage, gum loss is noticeable, the first destructive processes are just beginning, but the bone tissue is still suitable for implantation.
There are four stages of atrophy development
At the third stage, the loss is uneven, but it is quite pronounced, so if you want to do implantation, you can’t do without procedures to increase the volume. At the fourth stage1, strong destructive processes are noticeable in the central section (there is practically no spongy substance left here), and when restoring a tooth using traditional implantation methods, increasing the volume is mandatory.
Symptoms of atrophic processes in the bones
It is difficult to recognize the initial degree of pathology on your own. Later stages are already visible - the gum becomes lower and / or narrow (after all, the bone under it has atrophied). Other signs include exposure of the necks of adjacent teeth, implants, and food getting stuck under dentures. There may be a large amount of tartar, mobility of teeth, implants or prostheses (crowns, bridges), teeth visually become longer. All this is explained by the loss of bone tissue. And in the case of tooth mobility, there is also inflammation of the periodontium and dental ligaments. By the way, the gums may be inflamed and reddened, or they may become more whitish.
The mechanism of atrophy
The jaw bone is heterogeneous; it consists of several layers:
- central: this is the top layer where a large number of capillaries and vessels are located. This layer is quite loose or, as it is also called, spongy,
- cortical shell: consists of bony septa,
- basal: very dense section, not subject to atrophy and inflammatory processes. This is, in fact, the basis of the jaw bone, its base.
The jaw bone consists of several layers.
If the oral cavity is healthy and a person’s natural teeth are completely intact, then all layers of bone tissue receive adequate nutrition and blood supply. They function under the influence of chewing pressure. However, if the load for some reason disappears or changes (destruction, tooth loss and removal, periodontal inflammation), then negative consequences occur. The central spongy area is most affected.
If a person removes a tooth, then an empty space appears in the central part of the bone, there is no chewing load, and accordingly, food ceases to flow into this area, that is, it is, as it were, de-energized. Gradually, the spongy layer becomes thinner, it literally “melts” - this is called jaw atrophy. At the same time, the cortical and basal sections retain their volume.
The main causes of the pathological process
Jaw atrophy develops due to many factors:
- tooth extraction and untimely restoration: this is the main reason. All other circumstances listed below sooner or later again lead to loss of teeth,
- periodontal inflammation: periodontitis is the #1 cause of early tooth loss. The disease in its advanced stage leads to the destruction of the ligaments that hold the teeth in the sockets, causing them to become loose, shift and fall out,
- periodontal disease: not to be confused with periodontitis! This is a much less common systemic pathology,
- chronic diseases: diabetes, osteoporosis, cardiovascular pathologies, thyroid problems,
- bad habits: for example, smoking,
- metabolic disease,
- elderly age,
- injuries.
Keller classification
In accordance with the Keller classification, there are 4 types of atrophy of the alveolar process of the mandible:
- the alveolar process has retained its shape well, the frenulum is located normally (low),
- sharp and uniform shrinkage of bone tissue throughout the entire dentition, frenulums are attached above normal,
- severe loss in the lateral zones of the row, very slight atrophy of the alveolar process in the anterior area,
- stronger shrinkage in the anterior part of the jaw, in the lateral areas the atrophic process is weakly expressed.
%akc67%