Dental diseases include not only inflammatory processes occurring directly in the tooth, but also damage to the tissues surrounding the tooth - bone, periosteum or ligamentous apparatus. And basically all damage to surrounding tissues leads to tooth loss.
Inflammation of the periosteum
Periosteum is the lining or connective tissue between the bone tissue and the tooth. Periostitis is an inflammation of the periosteum; this disease is also commonly called “flux”. Periostitis is very easy to detect - a lump appears on the gum, usually filled with pus. Flux is a very serious disease that requires surgical intervention, but in no case self-medication.
The reasons for the appearance of flux can be various injuries that caused hematoma of internal tissues, as well as advanced caries or incomplete dental treatment. For example, the cause of gumboil can be pulpitis, the treatment of which the patient abandoned halfway through. If the doctor did not remove the nerve, but applied, for example, arsenic or a drug, you should definitely visit the dentist again to remove the temporary filling and install a permanent one, otherwise the nerve may begin to become inflamed and even rot, which will invariably lead to inflammation of the periosteum or bone tissue.
Don't suffer toothache! Come visit us today!
Complex treatment of caries - 6500 rub. for all! Flux treatment, full complex - 6500 RUR!
Periostitis: symptoms
- pain in the gum area
- the appearance of a lump on the gum
- increase in body temperature
- cheek tumor
Periostitis: treatment
- mandatory removal of carious cavity
- treatment or removal of an inflamed tooth nerve
- root canal treatment
- removal of a purulent source of inflammation (usually by a surgical method, which involves cutting the gums and releasing pus out)
- filling and prosthetics of damaged teeth
- drug therapy is used simultaneously with dental treatment
In case of flux, you should never treat yourself! The formation of pus indicates a serious inflammatory process. With self-medication, the purulent focus can increase and spread throughout the body. Traditional methods are used only to relieve pain and facilitate the treatment process, but nothing more.
Inflammation of bone tissue
Following the periosteum is bone tissue, in which the tooth root is securely fixed. Inflammation of bone tissue is always a very serious disease that leads to the destruction of hard bone and, accordingly, tooth loss. Periodontitis is an inflammation of the bone tissue surrounding the tooth. With periodontitis, the tooth is not alive, since the bacteria first attack the root and nerve of the tooth, and only then spread to the bone tissue.
The main causes of periodontitis include dental trauma, as well as acute caries or pulpitis, in which the nerve of the tooth dies.
Periodontitis: symptoms
- sharp pain
- the presence of carious cavities on the tooth
- bad breath
- tooth mobility
- fistulas on the gums (in the most severe stages)
What is osteitis of the jaw?
Osteitis of the jaw is an inflammatory process that occurs in the jaw bone tissue and spreads beyond the periodontium of one of the teeth to the spongy substance of the bones. This is a dental disease that develops along the neurovascular bundle, as well as through contact. It is often accompanied by periostitis (inflammation of the periosteum), less often osteomyelitis (inflammation of the bone marrow with the formation of fistulas, abscesses, and phlegmon).
Osteitis can be acute or chronic. Acute is characterized by destruction of dental bone tissue, and chronic develops in the presence of a chronic focus of infection in the periodontium of the tooth, followed by proliferation, when cells cannot perform a protective function, and the infection spreads deeply.
Diagnostics.
Treatment of inflammation of the periosteum of the tooth is carried out in several stages; first you need to undergo a comprehensive examination by a dentist. It includes:
- Initial examination. The doctor will assess the condition of your oral cavity, interview you and give you a referral for tests and x-rays.
- Having received all the necessary data, the specialist must determine what kind of disease the patient has. Because signs of periostitis are similar in symptoms to such pathologies as: acute periodontitis, phlegmon and osteomyelitis. Also, at this stage it is important to establish the exact form of the flux in order to draw up a suitable treatment plan.
Main symptoms of jaw inflammation
There are symptoms of osteitis that occur at the beginning of inflammation in bone tissue. This:
- sudden pain that occurs in the affected area of the jaw;
- swelling (hyperemia) of the sore spot;
- difficulty chewing food;
- spread of pain throughout the entire oral cavity.
If the source of infection is a sore tooth, then difficulty occurs when opening the mouth. If the disease develops rapidly, an increase in body temperature is possible.
With further development of osteitis, the inflammatory process is accompanied by suppuration in the affected area. The general condition of the patient depends on the associated secondary damage surrounding the bone tissue (periostitis, abscess, phlegmon).
Anatomical structure of the tooth
We figured out the order of the teeth. Further - more interesting! After all, a tooth is a unique organ, designed by nature to perform very important functions, primarily chewing. To be firmly held in the jaw bone, you need a root. The longest root is at the canine. Teeth can be single-rooted or multi-rooted. The structure of the upper teeth (molars) is somewhat more complex than that of the lower ones, since they have 3 roots. There are especially many variations in the number and type of roots in “wisdom teeth.” But the visible part of the tooth protruding above the gum is called the crown. It has different shapes in the incisors, canines and molars to perform the functions of biting, crushing or chewing food. The boundary between the crown and the root is the neck of the tooth. It is usually not visible, but it can become exposed due to certain diseases (periodontal disease, etc.). An x-ray is a kind of photo of the structure of the tooth and will give you an idea of what the state of affairs is in the oral cavity.
Treatment methods for osteitis of the jaw
Patients who suffer from inflammation of the jaw require complex treatment for osteitis. It includes surgery, as well as taking antibacterial drugs and special immunostimulating agents. If the teeth located in the area of tissue inflammation are severely destroyed and are a constant source of infection and inflammatory processes, then they must be removed.
If there is a general infectious disease that has caused inflammation of the bone tissue (tuberculosis, syphilis), treatment begins with its elimination. In other cases, the doctor drains the inflammation of the jaw through the root canal of the teeth. Physiotherapeutic treatment of the oral cavity is also carried out. Sometimes they resort to laser irradiation on the area affected by osteitis.
If you have the slightest suspicion of inflammation of the bone tissue in the oral cavity, you should immediately contact your dentist. If you start treating osteitis at the initial stage, it will not lead to serious complications and will not cause severe pain. After successful treatment, you should strictly adhere to the doctor’s prescriptions, carefully care for your mouth and teeth in order to prevent relapses of the disease and the transition of osteitis to a chronic form.
What are the possible consequences of atrophy?
Losing a tooth is not only fraught with cosmetic consequences, i.e. aesthetic defects. Functional impairments also occur. After all, healthy teeth have to take on excess load while chewing food. This means they break down much faster. In addition, all the teeth in the row shift and become mobile - after all, some of them lack lateral support. In general, the bite and facial expressions are disturbed, and wrinkles appear. The lips sink inside the mouth, problems arise with the pronunciation of various sounds, because the tongue loses support in the form of teeth, a decrease in the lower part of the face is observed, and flabbiness of the masticatory and facial muscles develops2. In addition, the digestive organs suffer, since a person most often switches to softer foods, since it is too difficult to chew excessively hard foods.
Options for solving the problem of bone loss
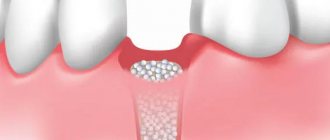
The main solution to the problem of bone loss is, of course, to prevent it, i.e. prevention. This means that after tooth extraction, you need to consider the option of surgical restoration or protecting the bone tissue from shrinkage. The first option will be discussed below, but the second involves the installation of protective barrier membranes. They are installed in the socket of the extracted tooth, and if necessary, a little artificial bone is added inside. In this way, it is possible to replenish the missing bone volume, making it possible to implant a tooth without using an extension procedure (but this is provided that it was not possible to install the implant immediately, i.e. at the time of tooth root removal).
So, when a patient is faced with a problem such as atrophy, bone tissue restoration can be performed using the following methods:
- sinus lift: performed exclusively on the upper jaw and allows you to lift or shift the maxillary sinus in order to make room for new bone. This operation is only applicable to change the height of the jaw bone,
- bone grafting with artificial materials: in this case, the jaw bone tissue is split and the freed space is filled with synthetic bone,
- bone block grafting method: for this procedure, the patient’s own bone material is used, usually extracted from the lower jaw (from the wisdom teeth area). The gum is cut, a bone block of the required size is cut out - it is transplanted to a new place and fixed with screws. Bone granules are placed around, and a membrane is attached to protect the tissue from being washed out.
Bone augmentation is a procedure that, although not complicated for an experienced surgeon, is very specific (and for the patient as well). When transplanting a bone block, at least 2 incisions are made, which means the patient will have to monitor the condition of several wounds at once. Plus additional material expenses: building up a large area of bone tissue is especially expensive.
“The cost of bone grafting is from 19-20 thousand rubles. And this does not take into account the implantation itself. In addition, the operation significantly lengthens the treatment process - at least 3-4 months must pass before the grafted bone can be used to install implants. Therefore, in our practice we use implantation methods that eliminate bone grafting. For the patient, this saves both time and money.”
Zhilenko Evgeniy Aleksandrovich, Implant surgeon, periodontist, orthopedist Work experience over 18 years make an appointment
Causes
There are several causes of the disease:
- Traumatic. The disease occurs due to a bruise, sharp biting on a hard object, or a blow to one tooth. Another possible cause is injury during root canal treatment with dental instruments.
- Infectious. It develops due to the penetration of microorganisms into the tissues surrounding the tooth root. Typically, periodontitis occurs due to Staphylococcus aureus, Streptococcus.
- Medication. Occurs due to the effect of potent drugs on the peri-apical tissues of the tooth. Signs of the disease appear within a few hours after exposure to the drug.
The inflammatory process can occur slowly or very quickly. This does not depend on the cause of its occurrence.
Types of dental periodontitis
Based on localization, the disease is divided into the following types:
- Regional periodontitis. In this case, tissue damage occurs near the edge of the gums. Often occurs due to injury.
- Apical periodontitis. The tissues are affected near the apical part of the root or at the base. In some cases, it is misdiagnosed as pulpitis.
According to stage, the disease is divided into:
- acute form;
- chronic form.
Acute periodontitis
May be purulent or serous. The first type is especially dangerous, as it can lead to the destruction of periodontal tissue. As a result, the teeth become mobile.
Chronic periodontitis
The chronic form is divided into granulomatous, granulating and fibrous periodontitis. The first two types are the most dangerous, as they are accompanied by pronounced bone resorption.
Treatment of tooth root resorption
The doctor chooses a technique in each specific case, taking into account the complexity and characteristics of the patient’s body. The dentist may resort to cleaning the canals and sealing them. When the process is advanced, when irreversible resorption of tooth roots is observed, removal of the unit followed by prosthetics or implantation is indicated.
In the early stages of small lesions, the surgeon removes the infected areas by making an incision in the gum.
If the cause is a tumor or an improperly growing adjacent tooth, then the tumor is removed surgically; the interfering or pathological unit (the choice is made by the doctor depending on the indications) is in most cases removed.
Prevention
To reduce the risk of developing the disease, you should follow simple recommendations:
- Brush your teeth at least 2 times a day. It is advisable not to use hard brushes to avoid injury to the gums.
- After eating, rinse your mouth with warm, clean water or a special mouthwash.
- Use toothpicks less often.
- Visit your dentist regularly.
- Remove tartar twice a year and undergo professional cleaning.
- Get rid of bad habits. Alcohol and smoking greatly impair dental health.
Periodontitis is one of the most common dental diseases. If you take good care of your teeth and maintain oral hygiene, you can significantly reduce the likelihood of its occurrence.
Back
Reparative bone regeneration is the restoration after injury. This process is of great importance for practical medicine. Bone tissue is unique because bone is capable of completely restoring even significant defects, unlike all other tissues in which regeneration ends with the formation of a connective tissue scar or organ hypertrophy.
There is no single definition of the term “reparative regeneration”. Some authors argue that this is a type of physiological regeneration that occurs under conditions of extreme influences on the body, but is more intense. Others characterize it as a complex process that is caused by the destruction of bone structures, quantitatively exceeding the permissible limits of physiological regeneration and aimed at restoring integrity and function.
The processes of bone tissue regeneration in the maxillofacial region are a complex interweaving of a number of general effects at the systemic level and local changes in tissue metabolism, including changes at the molecular level. Reparative regeneration is based on cell differentiation, their proliferation, resorption of damaged tissue and new bone formation during remodeling, as well as the formation of an organic extracellular matrix with its subsequent mineralization.
Stages of healing of bone tissue of the maxillofacial area
When healing fractures, the following four stages are distinguished: reparative reaction, formation of fusions of bone fragments, fusion of bone fragments, functional restructuring of callus and fragments with the formation of an organ structure.
Currently, researchers distinguish several stages of reparative regeneration:
- Tissue catabolism, differentiation and proliferation of cellular elements.
- Formation and differentiation of new tissue structures.
- Formation of vascular formations to nourish new tissue.
- Restructuring of the primary regenerate.
In the first stage, the reparative reaction of bone, there are such phases as acute post-traumatic disruption of tissue blood supply, cell necrosis with disorganization of cellular structures, proliferation of non-viable mesenchymal stem cells and differentiation of proliferating cells towards the formation of bone differential (mesenchymal stem cell - preosteoblast - osteoblast - osteocyte ).
Acute post-traumatic disturbances of tissue blood supply in the fracture area are accompanied by rupture of the periosteum, endosteum, osteon canals, as well as bone marrow, vessels and nerves, muscle and connective tissue surrounding the bone. These processes are accompanied by hemorrhages, edema, macrophage infiltration and the development of diffuse ischemic degenerative-necrotic changes in tissues. This phase lasts about 6-18 hours from the moment of injury.
The second phase, lasting 10-24 hours after injury, is accompanied by disorganization of bone tissue structures, signs of necrosis and macrophage cell infiltration.
In the third phase, which occurs within 24-72 hours from the moment of fracture, against the background of restored blood supply, proliferation of mesenchymal stem cells, pericytes of the microvasculature, periosteum, endosteum with the formation of osteogenic tissue is observed. Depending on the location of the proliferating cells, periosteal (periosteal cells), endosteal (bone marrow cells) and intermediate (cells of the bone marrow and vessels of the central canals) bone formations are distinguished.
The fourth phase of the reparative reaction is accompanied by proliferation and differentiation of osteogenic cells into preosteoblasts and osteoblasts. They synthesize osteoid, which after mineralization turns into coarse fibrous bone tissue. Activation of osteoclasts is observed, which resorb necrotic bone tissue.
At the stage of formation of fusions of bone fragments, which occurs 3-5 days after the injury, bone regenerate, or callus, is formed, which spreads in the proximal and distal directions. After 2-6 weeks, this process leads to the fusion and consolidation of bone fragments.
The last stage of fracture healing is characterized by the formation of bone adhesions, which can be of several types. Primary bone fusion is accompanied by direct fusion of fragments at the level of the cortical layer with the formation of new osteons. Fibrous-cartilaginous fusion is characterized by the development of necrosis of bone and soft tissue in the fracture zone, a sluggish reparative reaction that develops at a considerable distance from the fracture site, and the predominant development of fibrous and, less commonly, cartilaginous tissue.
The existing fibrocartilaginous bone fusion as a result of prolonged ossification can be replaced by bone tissue, forming a secondary fusion of bone fragments. In the fourth stage, a functional restructuring of the callus and fused fragments occurs with the formation of the organ structure of the bone.
Cells and substances involved in reparative regeneration
of bone tissue
The process of regeneration of bone tissue in the maxillofacial area occurs with the participation of cells such as osteoblasts, osteoclasts or osteocytes . Below is a brief description of these cellular elements, indicating the features of their structure and functions.
Osteoblasts
are bone-forming cells that originate from mesenchymal stem cells. They are round in shape, 20-30 microns in size, with an eccentrically located core. These cells are located in the osteogenic layer of the periosteum and in the perivascular spaces of osteons.
There are four types of osteoblasts involved in the healing of bone tissue: preosteoblasts, proliferating functionally active osteoblasts, maturing osteoblasts with a hypertrophied endoplasmic reticulum, and differentiated low-active osteoblasts. The main part of osteoblasts synthesize bone tissue until their function stops, followed by their transformation into inactive cells.
These cells line the surface of the newly created bone tissue and connect to osteocytes through a system of tubules. A certain part of osteoblasts are encapsulated in the osteoid matrix and differentiate into osteocytes.
Osteoblasts have a developed Golgi apparatus and mitochondria, due to which they synthesize a huge amount of intercellular substance, in particular proteins and collagen fibers, which form the organic bone matrix - osteoid. Osteoblasts synthesize type I collagen from procollagen, which consists of one α2- and two α1-polypeptide chains forming a helical structure.
The procollagen molecule contains two terminal peptides: amino- and carboxy-terminal propeptides. After the secretion of procollagen by osteoblasts into the extracellular space, these two propeptides, under the influence of enzymes, are cleaved from procollagen, which is transformed into tropocollagen.
Free final propeptides of bone tissue enter the circulating blood, where their concentration can be determined by the enzyme immunoassay method. This analysis very accurately indicates the amount of type I collagen synthesized, with the level of amino-terminal propeptide most accurately characterizing its metabolism.
Osteoblasts also synthesize the non-collagenous fraction of bone matrix proteins, which play a leading role in its mineralization. These are osteocalcin, osteopontin, osteonectin, and bone sialoprotein.
Osteocalcin is the main non-collagenous bone protein that is involved in the binding of calcium and hydroxyapatite. It has a chemotactic effect on osteoclasts and is involved in bone resorption.
Osteonectin binds type I collagen and hydroxyapatite and takes part in the formation of the initial crystal (nucleation) during bone mineralization. Osteopontin also binds bone cells to hydroxyapatite in the extracellular space, but recent studies indicate the involvement of this protein in tumor metastasis by facilitating the adhesion of tumor cells during invasion.
Bone sialoprotein contains sialic acids. It is a calcium-binding glycoprotein that provides mineralization and stabilization of the collagen structure.
Osteocytes
, or “stellate cells,” have a large number of long and thin processes. They are divided into three types, the characteristics of which are briefly listed below:
- Type I osteocyte-producing cells synthesize bone matrix components.
- Type II osteocytes, mature or resorbing cells, are involved in the process of osteolysis.
- Type III osteocytes, degenerating cells, are located at the periphery of the osteon. As a result of their destruction, a significant amount of lysosomal enzymes is released and osteolysis of bone tissue occurs.
Osteocytes have receptors for parathyroid hormone, synthesize osteocalcin, matrix proteins and sclerotin, which is an inhibitor of the Wnt signal in osteoblasts. Their main function is the transmission of mechanical and chemical signaling to osteoblasts, integumentary cells and, through them, to osteoclasts. This circuit plays an important role in triggering bone remodeling processes under physiological and pathological conditions.
Osteoclasts
are multinucleated giant cells that provide resorption of bone matrix components. They are located on the surface of the bone in small depressions (erosive lacunae or Howship's lacunae). In places of contact with areas of bone resorption, the cytoplasm of osteoblasts forms outgrowths in the form of a corrugated border, which increases the area of contact with the bone and facilitates the entry of biologically active cellular products into the resorption zone.
Osteoclasts also secrete protons and proteolytic enzymes (cathepsin K, cysteine protease, matrix metalloproteinases) into the resorption zone and remove decay products into the surrounding space through the basolateral membrane. For such transport to occur, the presence of tartrate-resistant acid phosphatase (TRAP) is necessary. There are 5 types of acid phosphatases, which are produced by bone tissue, spleen, red blood cells, platelets and macrophages. All types of acid phosphatases are inhibited by tartrate, except for the fifth isoform, which is called TRKP-5.
Osteoclastogenesis,
osteoblastogenesis and bone remodeling
The following functional types of osteoclasts are distinguished: young, mature, functionally active and inactive, as well as dying. The source of origin of all osteoclasts is macrophage-monocyte cells of the bone marrow.
The RANK/RANKL/OPG system, which was discovered in 1997, plays an important role in osteoclastogenesis. RANKL, expressed on the surface of osteoblasts, binds to the RANK receptor, which is located on the membranes of osteoclast precursor cells. This triggers differentiation and activation of osteoclasts. The interaction of RANKL and RANK occurs in the presence of macrophage colony-stimulating factor (M-CSF), which, using high-affinity transmembrane receptors (c-fms), activates intracellular tyrosine kinase and stimulates the proliferation and differentiation of osteoclast precursors, mononuclear cells.
M-CSF activity has been shown to be significantly increased by exposure of osteoblasts to parathyroid hormone, vitamin D3, and tumor necrosis factor (TNF), but decreased by exposure to OPG and estrogens.
Osteoprotegerin is synthesized by osteoblasts, vascular endothelial stromal cells and B-lymphocytes. It is a soluble decoy receptor for RANKL that interferes with the interaction of RANKL and RANK, which impairs osteoclastogenesis and inhibits bone resorption. At the same time, interleukins (IL) -1,3,6,11, tumor necrosis factor-α (TNF-α), granulocyte-macrophage colony-stimulating factor (GM-CSF) and prostaglandins E2 (PG2) through the EP4 receptor are able to enhance the production RANKL by stromal cells of the bone environment, in particular osteoblasts, which stimulates osteoclastogenesis.
It was found that the production of osteoclasts is stimulated by parathyroid hormone. It is synthesized by the parathyroid glands. The hormone maintains calcium homeostasis by leaching from bone into the extracellular fluid and enhancing reabsorption in the renal tubules. This hormone activates the synthesis of acid phosphatase, lactate and citrate, and inhibits the synthesis of collagen and alkaline phosphatase.
With a sharp increase in the level of parathyroid hormone in the blood, activation of mature osteocytes and bone resorption (osteocytic osteolysis) are observed. With prolonged hypersecretion of parathyroid hormone, osteoclastogenesis increases and the activity of osteoblasts decreases, which also suppresses collagen synthesis. It has been proven that long-term administration of small doses of parathyroid hormone causes an anabolic effect, and this, on the contrary, promotes the maturation of cartilage tissue. It promotes the synthesis of 1,25-(OH)-2D3 in the kidneys under the influence of cyclic AMP from 25-(OH)-2D3.
Unlike parathyroid hormone, calcitonin, which is secreted in the interfollicular cells of the thyroid gland, reduces the number and activity of osteoclasts in bone tissue, suppresses osteocytic osteolysis and reduces the level of calcium in the blood. Calcitonin stimulates the maturation of chondrocytes in epiphyseal cartilage.
According to foreign studies in recent years, the leading role in the regulation of osteoblastogenesis belongs to bone morphogenetic proteins (BMP, bone morphogenetic protein). This is a group of signaling growth factors (cytokines) that actively stimulate the formation of enchondral bone tissue and regulate various cellular processes (proliferation, differentiation, apoptosis, chemotaxis, angiogenesis or production of extracellular matrix in tissues).
BMPs trigger the process of bone tissue formation through the expression of genes that regulate the processes of differentiation of mesenchymal stem cells with the subsequent formation of osteoblast cells. Dysregulation of the BMP signaling system is very often found in cancer.
Currently, 47 BMP subfamily proteins that interact with specific BMP receptors (BMPs) have been described. In the process of intercellular interactions in the bone tissue of the maxillofacial region, the following are especially important:
- BMP2: stimulate osteoblast differentiation.
- BMP3: promotes the formation of new bone tissue.
- BMP7: activate osteoblast differentiation and SMAD1 production.
- BMP8a: are directly involved in the development of bone and cartilage.
In practical medicine, BMP is used to stimulate bone healing processes. They are injected into a bone implant, from where they are delivered to fracture sites to improve osteogenesis.
Bone cells intensively secrete transforming growth factor β1 (TGFβ1) into the interosseous matrix, which activates the differentiation of mesenchymal stem cells according to the osteoblastic and chondral type, stimulates the processes of reparative bone regeneration, and enhances proliferation and collagen synthesis.
Processes associated with cell morphogenesis are also regulated by Wnt signaling. This process involves proteins discovered in the early 1980s as markers for certain types of cancer. They are also key regulators of the processes of remodeling and regeneration of bone tissue, differentiation of mesenchymal stem cells.
The canonical pathway of Wnt signaling in bone tissue is based on the stabilization of the cytoplasmic protein β-catenin. In the absence of a signal, it is inactive and quickly destroyed. When β-catenin is activated through Wnt, Wnt itself binds to cell surface receptors, which are the Friesland transmembrane protein. As a result, the destruction of β-catenin is inhibited, it accumulates in the cytoplasm and then penetrates into the nucleus. There it interacts with TCF/LEF proteins, which selectively bind to specific activator proteins and DNA sequences.
In this way, certain genes responsible for bone tissue regeneration are activated. Another, or non-canonical (β-catenin-independent) Wnt signaling pathway regulates cell polarity, stimulates calcium metabolism and cytoskeletal reorganization. Wnt signaling stimulates OPG production. It has been proven that at least 22 Wnt ligands are involved in the activation of Wnt signaling in humans.
An antagonist of the Wnt/β-catenin signaling pathway is sclerotin glycoprotein, which is produced by osteocytes of intact bone. It prevents MSC differentiation. When damage occurs to the bone tissue of the maxillofacial region, osteocytes transmit a signal to the integumentary cells that line the surface of the trabecula. Under the influence of prostaglandins and growth factors, which are released, the integumentary cells peel off from the surface of the bone, forming a specific canopy. The canopy cells combine with osteocytes and the capillary to form a bone remodeling compartment.
Recently, regulators of intercellular interactions between osteoblasts and osteoclasts, such as semaphorins and their receptors plexins, have been discovered. Semaphorins form a family of molecules consisting of 8 main classes of secretory and transmembrane proteins that are responsible for transmitting signals along axons. They regulate the growth, development and functioning of cells of the nervous, cardiovascular, immune, respiratory, and musculoskeletal systems.
In particular, Semaphorin 4D (Sema4D), which is a derivative of osteoclasts, acts on the membrane receptor Plexin-B1 on the surface of osteoblasts, suppressing the function of the latter. As a result, activation of bone tissue resorption is observed. Semaphorin 3B promotes the activation of osteoclasts, and semaphorin 3A, on the contrary, stimulates osteogenesis. Based on this, inhibition of semaphorins 4D and 3B is important for the treatment of osteopenia.
An important secretory derivative of osteoclasts is the SLIT3 protein. It stimulates the proliferation of osteoblast cells through activation of the β-catenin pathway. SLIT3 autocrine signaling inhibits bone resorption by suppressing preosteoclast differentiation. Experimental studies have shown that modified animals lacking SLIT3 or its receptor Robo 1 have low rates of bone formation and a high rate of bone resorption.
Practical assessment of bone tissue regeneration processes
The processes of bone tissue remodeling can be clearly assessed based on a comparative analysis of two groups of bone metabolism indicators - markers of bone resorption (hydroxyproline, hydroxyproline, calcium, breakdown products of type I collagen, pyridinoline and deoxypyridinoline, bone sialoprotein (BSP), tartrate-resistant acid phosphatase) and synthesis markers bones (osteocalcin, bone alkaline phosphatase, amino and carboxy-terminal fragments of type I procollagen, ACP, CCP).
Markers of bone tissue synthesis indirectly characterize the activity of osteoblasts. These cells take an active part in the formation of bone tissue, produce type I collagen plus other osteoid components, and participate in the mineralization of osteoid with hydroxyapatite.
The first biochemical marker of bone remodeling is the enzyme alkaline phosphatase, which was introduced into clinical practice in 1929 and is used today. There are 4 isoforms of this enzyme: bone, liver, intestinal and placental.
A laboratory indicator of osteoblast activity is bone alkaline phosphatase. This is a glycoprotein that takes part in the mineralization of the bone matrix. A simultaneous increase in ALP and parathyroid hormone may indicate the development of osteodystrophy with a high level of bone remodeling, and a decrease in these indicators may indicate an adynamic state of the bone tissue of the maxillofacial region.
The most informative marker of bone formation is osteocalcin. This non-collagenous bone matrix protein containing hydroxyapatite can be considered specific for bone tissue and dentin. It is synthesized primarily by osteoblasts and forms the extracellular matrix of bone.
A fraction of newly synthesized osteoclasts is released into the bloodstream, so this marker indicates the rate of bone tissue remodeling. An increased level of parathyroid hormone in the blood suppresses the activity of osteoblasts that produce osteoclasts and reduces the concentration of osteoclasts in the blood and bone tissue.
During the synthesis of type I collagen by osteoblasts, amino- and carboxy-terminal fragments are separated from type I procollagen as a result of the action of specific enzymes. The ratio between the amount of mature collagen deposited in the bone matrix and the number of terminal molecules that enter the bloodstream must be equal to one. Thanks to this, based on the indicators of ACF and CCP in the blood serum, one can judge the synthetic activity of osteoblasts in the synthesis of type I collagen.
The next group of bone remodeling indicators are markers of bone resorption. It should be noted that they change their level during the day, so they must be determined at the same time of day, preferably in the morning. Markers of bone tissue resorption include enzymes involved in the destruction of the bone matrix under the influence of osteoblasts and products of the destruction of type I collagen.
This is, for example, tartrate-resistant acid phosphatase (TRAP) - a metal-containing enzyme, one of 6 isoenzymes of acid phosphatase. It is secreted by osteoblasts into the extracellular environment during resorption. There are forms of TRAP-5a and 5b, but TRAP-5b is synthesized by osteoblasts, and TRAP-5a is of macrophage origin. TRAP-5b activity in blood plasma is an indicator of bone resorption processes.
Hydroxyproline is the main amino acid in collagen. It is not considered an autospecific marker of bone tissue, because only 50% of this amino acid is found in bones, and the remaining 50% is a component of other proteins, in particular elastin, acetylcholinesterase and complement factor C1q.
Most of it, after the destruction of collagen, is oxidized in the liver and only 15% is excreted in the urine. The content of hydroxyproline depends on the nature of the diet, the age of the person, the presence of a tumor with decay and demonstrates a circadian rhythm with a peak between 0.00 and 8.00 am.
14% of the amino acid composition of collagen is hydroxyproline. It is synthesized by osteoblasts and is also a marker of bone resorption. Nowadays, more specific markers of bone resorption are used, such as type I collagen breakdown products. These include pyridinoline (PID) and deoxypyridinoline (DPID). They are found in tissues containing type I, II, III collagen. PID is an important chemical compound, but DPID is found only in collagen, so it is evaluated as a selective bone marker.
Also widely used in medical practice is the determination of type I collagen peptides, NTX and CTX. The uniqueness of these indicators lies in the rapid increase in their level in diseases accompanied by high bone tissue resorption (for example, osteoporosis, bone metastases), as well as their rapid decrease (within several weeks) against the background of antiresorptive therapy.
The next marker of bone resorption is bone sialoprotein (BSP). During the process of osteolysis (physiological or pathological), the bone matrix is destroyed by osteoblast enzymes with the release of sialoprotein into the blood with a corresponding increase in laboratory BSP parameters. Bone sialoprotein is present only in mature osteoblasts and is not found in their precursors, so BSP may serve as a marker of late differentiation of bone cells.
Conclusion
Reparative regeneration of bone tissue in the maxillofacial region is associated with the activity of osteogenic cells. The local regulation of reparative regeneration is based on several signaling pathways, such as the RANK / RANKL / OPG molecular system, bone morphogenetic proteins, Wnt signaling and others.
Osteoblastogenesis and osteoclastogenesis characterize biochemical markers of bone remodeling, the determination of which allows one to determine the rate of metabolic processes in bone tissue, identify patients at increased risk and conduct an early assessment of the effectiveness of prescribed treatment, predict the risk of complications, diagnose the appearance of bone metastases in the early stages, etc.