Causes of facial allergies
Atypical reactions of the immune system to foods, chemicals and biological substances can cause rashes, pimples, redness, swelling and itching. The person experiences physical and moral discomfort. The manifestations of allergic reactions are varied and depend on the individual characteristics of the body. Most often, localization is observed on the forehead, temples, cheeks, behind the ears, in the décolleté area and on the neck. The most common prerequisites for allergies are:
- heredity;
- consequences of long-term use of medications;
- unfavorable environment;
- constant stress;
- reduced immunity;
- too high a concentration of certain substances;
- insect bites;
- cold or direct sunlight.
There may be other reasons; you need to approach the problem individually.
Allergies to foods and medications
There is often cross-reaction to the protein in this group, making it difficult to find the source. The speed of onset of symptoms can vary from immediate to a period of 2-3 hours. In the case of medications, the prerequisite is overdose, long-term use, too many drugs taken during the day.
Sun or cold
The body’s response is characteristic not only of winter. This could be water or food at a certain temperature. The appearance of photodermatitis is promoted by internal and external causes. Within a day or a little later after exposure to the sun, soreness and itching of the skin begin to bother. When an allergic rash appears on the face of an adult, treatment should begin immediately, otherwise the situation will worsen with each passing hour. As part of complex therapy, immunostimulating cosmetics such as Laennec are effective. Before use, you should consult with specialists.
Reaction due to eczema
Skin diseases significantly reduce the body's resistance, and any violation provokes their exacerbation. Most often, the reaction appears externally in the form of small bubbles with liquid. The acute form can become chronic, which subsequently leads to relapses.
Errors in diet
Various dietary restrictions do not go out of fashion. There are programs based on the consumption of one or just a few products for a long time, which leads to an oversaturation of the body with certain elements, since in this case there can be no talk of balance. You should not be surprised at the deterioration in well-being, since such restrictions become the causes of severe allergies on the face of an adult, the treatment of which is carried out comprehensively and will take a lot of time.
We recommend
GHC Placental 3D Mask withQ10
Serum concentrate
Repairing cream with a moisturizing effect
Placental antioxidant lotion concentrate
Contact with animals, insect bites
A swollen nose and watery eyes when trying to pet a pet are a true classic of the genre. Mosquitoes, bedbugs and other blood-sucking creatures can also cause itching and redness on the skin. The toxins they inject in large quantities cause a rash, often accompanied by fever. In this case, external agents and antihistamines are recommended; dosages should be confirmed with a doctor.
Allergies due to stress
In addition to nervous tics, there are other reactions to emotional overload. Unconsciously, a person may scratch or clench their hands tightly. If such situations happen regularly, then health problems may begin. Itching, swelling of certain areas, redness, and difficulty breathing appear. The main direction of stabilizing the condition is the prescription of sedatives, breathing exercises aimed at calming the nervous system, ointments and gels to relieve external manifestations on the skin.
Ringworm “as a keepsake”: the most common skin problems after COVID-19 are named
Source: "DoctorPeter" Date: 07/23/2021
Hair loss and skin rashes are common complaints among those who have recovered from COVID-19. As the City Committee for Internal Affairs said, doctors have not yet identified exclusively “Covid” skin problems - many of them also arise with other diseases.
Related to COVID-19, but not certain
According to Elena Moshkova, dermatologist of the City Clinical Infectious Diseases Department, no special skin rash characteristic only of coronavirus infection has yet been identified.
— Taking into account the still short period of observation of patients with COVID-19 and skin manifestations, it cannot be stated unequivocally that there are pathognomonic skin rashes (unambiguously describing a specific disease - editor's note), and they can be used to confirm infection with the new virus. Quite the contrary. The patient knows that he has a history of coronavirus infection, and the doctor can conclude that these skin manifestations are most likely associated with a viral disease, Elena Moshkova told Doctor Peter.
The doctor named the 5 most common skin complications after Covid with which patients come to the City Clinical Hospital.
Pink lichen of Zhiber
It appears as round, scaly spots usually up to 2 cm in diameter. Over time, the central part of the spot fades, but the edges remain quite bright. Patients may experience itching, but not always - this is individual. According to Elena Moshkova, Zhiber’s pityriasis rosea can occur not only after Covid, but also against the background of a common ARVI, and in other situations when immunity is reduced.
“It is important that this dermatosis is not contagious and for most it can go away within a few weeks even without treatment. Such patients rarely require the use of glucocorticosteroid creams and systemic therapy, the dermatologist said.
Skin vasculitis
Another common problem.
Skin vasculitis is characterized by hemorrhagic spots, which fade over time like small bruises. Some people, most often older people, may develop areas of necrosis - dead cells - on the skin. — The coronavirus that causes COVID-19 is tropen (prefers - editor's note) to vascular receptors. Therefore, it is not surprising that skin vessels can also be affected, often on the hands and feet. However, the diagnosis of “vasculitis” existed in dermatology even before Covid, the doctor adds.
Rashes
Toxic-allergic rashes also occur in those who have recovered from the disease . However, according to Elena Moshkova, in most patients with such problems, doctors cannot determine for sure whether this is a consequence of COVID-19 or a reaction to taking medications in the treatment of a viral disease.
In addition, those with a high fever may suffer from common heat rash - this often goes away on its own, but in some cases special medications may be required to reduce the itching. After a coronavirus infection, doctors also observe urticaria-type , usually on the skin of the palms. According to Elena Moshkova, if you have urticaria, you still need to go to the doctor - he will conduct a differential diagnosis, because it can be confused with a variant of skin vasculitis.
Rare, but without bald spots
Those who have recovered from Covid go to the City Clinical Internal Affairs Department not only with rashes and spots on the skin. Both men and women are often worried about another post-Covid problem - hair loss, as “Doctor Peter” has written about more than once. Hair does not begin to fall out immediately, but only several months after the illness. As doctors specify, the hairline thins, but bald spots do not form.
— The main reason is impaired blood circulation in the scalp due to damage to the vascular walls. Plus, stress, concomitant intoxication, and drug therapy for the disease contribute to this. And under unfavorable conditions, the alternation of phases of activity and rest of the hair follicles is disrupted. This happens regardless of the severity of Covid - everything is individual,” explains Elena Moshkova.
According to the doctor, usually over time, blood supply to the scalp is restored and hair density returns to normal. Good nutrition also helps speed up the solution. However, consulting a trichologist in this situation may not be superfluous, especially if the problem is too noticeable.
* Nadezhda Krylova
Types of allergies on the face
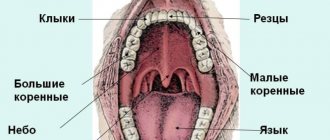
If in children the most vulnerable area is the buttocks, where signs appear that indicate certain foods or unfavorable conditions, then in adults this is the nasolabial triangle, eyelids, lips, tongue, neck and hands.
Atopic dermatitis
Chronic inflammatory skin disease. Most often begins in early childhood. The priority prerequisite is genetic predisposition. It can be a concomitant disorder with bronchial asthma and conjunctivitis. There are infant, child and adult forms of the disease.
Hives
Allergies and rashes in the form of pimples on the face, the photo of which most often appears on advertising posters of the newest antihistamines, occurs with a seasonal variant. It is characterized by lacrimation, swelling of the eyelids, obsessive itching, and redness of certain areas of the body.
Food reactions can occur instantly when certain foods enter the mouth and esophagus. Most often they are milk, eggs, red or yellow fruits, and nuts. Peanuts are the most dangerous in this regard.
Contact dermatitis
Recognizable by clear zones of irritation. The causes are hygiene and cosmetic products, chemicals that come into contact with unprotected skin, jewelry, piercings, latex products, extracts and juices of certain plants. It manifests itself in the form of weeping erosions, in place of which dry scales then appear. To understand how to remove facial allergies, you need to find and eliminate the substance that causes your health to worsen. Often a good result comes from moving to another region. This way, it is possible to cut off some of the options; for the rest, you will have to take special tests in the laboratory.
Toxicoderma
A distinctive point is inflammation not due to external factors, but due to the penetration of a provoking substance into the body. In some cases, it can cause secondary damage to internal organs and anaphylactic shock, since it develops rapidly from the ingestion of an allergen from the inside. One way to prevent inflammation is to take antibiotics, especially penicillin. At the same time, timely treatment gives good results.
The alimentary variety is included in a special group; the deterioration of the condition is provoked not by products, but by food additives in their composition. It is quite dangerous due to the fact that it can occur suddenly, since manufacturers do not indicate all the ingredients in the composition.
Quincke's edema
It poses a direct threat to life. In the question of what an allergy on the face and neck looks like in this case, what to do and how to treat it, time is of the essence. Choking occurs quickly, and the slightest delay can have fatal consequences. An acute inflammatory reaction of the body, which occurs locally in the skin and subcutaneous tissue, affects deep layers, including the muscles of the respiratory system, and in a third of cases is localized in the larynx. It is impossible to prevent the development of Quincke's edema. Women suffer from this disorder more often. The diagnosis is made based on the clinical picture and requires medical attention. Signs may persist for several days and disappear gradually. Treatment includes the administration of potent antiallergic drugs. In severe cases, the patient requires urgent hospitalization in an intensive care unit or intensive care unit.
Causes of seborrheic dermatitis on the face
The main cause of seborrheic dermatitis is the increased functioning of the sebaceous glands and a change in the composition of the fat they produce. A similar situation develops when the Malassezia fungus multiplies excessively (normally it is part of the skin microflora). In this case, it penetrates the sebaceous glands and produces a special secretion that forces subcutaneous fat to break down, forming fatty acids that irritate the skin and contribute to the occurrence of rashes.
Dermatitis affects men more often than women, which is explained by the action of androgen, a male hormone. This hormone stimulates the synthesis of subcutaneous sebum. In women, the disease usually manifests itself when estrogen levels decrease and androgen concentrations increase.
Seborrheic dermatitis on the forehead is especially often diagnosed in people whose close relatives have a similar problem, which is associated with a hereditary predisposition.
Other factors can also provoke the development of the disease:
- hormonal imbalances;
- disruption of the endocrine system (especially the thyroid gland);
- weakened immunity;
- hypovitaminosis;
- unfavorable environmental situation;
- improper facial skin care;
- excessive sweating;
- poor nutrition;
- lack of sleep;
- uncontrolled use of medications, especially hormonal ones;
- exacerbation of chronic diseases;
- presence of infection in the body;
- dysfunction of the nervous system, manifested in the form of epilepsy or schizophrenia;
- diabetes;
- pathologies of the gastrointestinal tract;
- frequent stressful situations;
- overwork;
- malignant tumors in the adrenal glands or genitals.
What does an allergy look like on the face?
There are many manifestations of allergies, and they depend on the form, location and intensity. The main indicator of the disorder is sudden swelling of the eyes and lips, one or both. Changes also affect the structure of the skin. It becomes lumpy, swollen, with a small scattering of small dots. Red, uneven spots of varying sizes often appear. Cracks and a scaly structure may be observed. If you give in to temptation and start scratching the itchy areas, the condition will quickly worsen.
Depending on the type of disorder and the affected area, allergic rashes on the face are likely, the treatment of which requires an integrated approach. Along with pharmaceutical drugs, cosmetics have a fairly good effect. Plasma therapy with the Japanese drug CURACEN perfectly restores appearance, but only after the acute period ends and the condition stabilizes.
How to diagnose allergies
The main difficulty is to distinguish it from a skin disease. Rashes should not be a reason for panic, but a prerequisite for examination. To prevent exacerbation and speed up the process of identifying causes, it is necessary:
- try to independently identify the allergen by eliminating cosmetics or products from everyday use, doing this gradually in order to replace the changes in time;
- take an antihistamine that has already been used as prescribed by a doctor;
- Remove all alcohol-based external care products from use.
After such measures, it will be much easier to determine how to relieve an allergic reaction on the face and alleviate the general condition.
We recommend
GHC Placental 3D Mask withQ10
Serum concentrate
Repairing cream with a moisturizing effect
Placental antioxidant lotion concentrate
Treatment of seborrheic dermatitis in adults and children
Seborrheic dermatitis may resolve without treatment. But it often occurs in waves, with remissions and exacerbations.
Several repeated courses of therapy or ongoing maintenance therapy may be required until the symptoms go away completely. After some time, exacerbation may occur again.
You should consult a doctor if repeating the usual regimens of care and relieving acute symptoms does not help, as well as if there are signs of a secondary infection.
The basis of therapy is the use of medicinal shampoos, creams and lotions.
For children, it is recommended to use special children's shampoos; before washing, you can apply oil or cream to help soften the crusts.
In children, it is important to stop itching, since scratching can cause secondary infection of the scabs.
Features of the treatment method
When selecting external skin care products, choose products containing the following ingredients that reduce skin inflammation:
- Keratolytics: salicylic, lactic acid, urea, propylene glycol.
- Topical antifungal agents: shampoos and creams containing ketoconazole (ciclopirox).
- Products with selenium disulfide or zinc pyrithione.
- Local low-strength corticosteroids can only be used as prescribed by a doctor to relieve the acute phase of the disease, except for the facial skin.
- In case of resistant forms, patients may be offered oral antifungal drugs.
- In severe cases, isotretinoin or phototherapy may be considered.
How is seborrheic dermatitis treated at the Rassvet clinic?
We evaluate the patient's skin type, severity and location of the rash.
The diagnosis of seborrheic dermatitis is based on the clinical picture. The detection of Malacesia has no diagnostic value, since this is a normal microflora of human skin.
A dermatologist evaluates the condition and makes a differential diagnosis with psoriasis, rosacea (on the face), pityriasis versicolor (on the body), and atopic eczema in children. At first, we usually recommend shampoo and only if the selection of permanent skin care products fails, do we move on to active drug therapy.
Treatment
It is not recommended to use drugs other than antihistamines on your own. In most cases, they are enough to eliminate the main symptoms and relieve swelling. It is necessary to take into account that the action must be comprehensive and must include creams, ointments and gels to relieve external signs of the disease.
Preparations for internal use
Medicines prescribed by a doctor are divided into corticosteroid and non-hormonal. The first are produced on a hormonal basis, have a powerful effect, but have a number of serious contraindications for long-term use. The second, milder ones, are prescribed to relieve mild forms of irritation. Several generations of antihistamines are available in pharmacies. If the former, such as Suprastin, influenced the level of attention, causing drowsiness and inhibition of reactions, then Cetrin, Telfast, Claritin, with high efficiency, do not give side effects that could become a limitation for work in areas where concentration is required.
Cosmeceuticals and their help in the fight against allergies
When the body reacts violently to a stimulus, skin lesions are sure to appear, and sometimes quite unpleasant ones. These are not only rashes and pimples, but also increased dryness and microcracks. Their danger lies in the possible entry of bacteria and the development of local inflammation. The main task, along with eliminating illness, is strengthening the immune system. Cosmetic products from the medical corporation "RHANA" are used in professional problem solving, provide a quick and lasting positive effect, allowing you to maintain beauty, health and prevent premature aging. And the skin is susceptible to it if an allergic reaction often appears on the face, a photo of which clearly demonstrates the degree of damage to the integument.
In order to give a fresh look and ensure cellular renewal, it is recommended to use placental preparations:
- Modeling mask with placenta hydrolyzate GHC Placental 3D Mask withQ10. It will prevent the risk of developing inflammation and give a healthy tone.
- Concentrate serum for intensive revitalization GHC Essence will instantly restore inner radiance, and also improve microcirculation and cell nutrition.
- LNC Repairing Cream with a moisturizing effect will preserve the beauty and freshness of the skin, and also protect it from moisture loss and eliminate the regeneration of ceramides (epidermal cells).
- Placental antioxidant lotion concentrate LNC Toning Lotion will protect cells, normalize melanin production and provide optimal hydration.
The dangers of self-medication
According to preliminary forecasts, the number of people reacting to certain stimuli will reach almost 90% by the end of the century. Allergists-immunologists mention the fault of allergy sufferers themselves, who, by self-medicating, expand the range of allergens and provoke the development of other diseases. In this case, the part is fixed and passed on by inheritance. By identifying the cause and drawing up an optimal treatment regimen, you can almost completely eliminate the likelihood of regular exacerbation of allergies.
Fast wound healing
CONDITIONS
- The wound must be clean, free of foreign matter, dirt, particles, and non-viable tissue;
- The wound should not be infected;
- The wound should not remain open and in contact with the environment;
- Healing should occur in moderately
moist environment.
And now, in order: Condition of the wound.
It should not contain foreign particles, dirt, or non-viable tissue.
Any dirt, clotted blood and pus must be removed, that is, the wound must be treated and washed. Hydrogen peroxide, saline solution, or, in extreme cases, just clean water will do. If the wound is chronic, poorly healing with a dry, poorly detachable bottom (eschar), it is necessary to use a special gel ( Fibrogel Ag
or
Intrasite gel
) in combination with a secondary absorbent dressing (Allevyn Adhesive, Non Adhesive), or in combination with a breathable film dressing (Opsite FlexiFix , Opsite Flexigrid). However, if you have a deep chronic wound, we recommend that you first seek help from specialists.
Presence of infection.
The presence of an infectious process in the wound negatively affects the healing process.
If measures are not taken, the wound may become chronic, as a result of which the healing process may take a long period. It has long been proven that silver has a pronounced antibacterial effect, due to which the use of silver-containing dressings significantly helps to block the growth of bacteria and the development of infection in the wound. If there is an infectious process, it is necessary to use a bandage with silver nanocrystals (Acticoat or Acticoat 7); Neofix Fibrotul Ag
. Matching headbands are here.
Closing the wound.
The wound must be protected from environmental influences and infection. If the wound is small, an abrasion or a scratch, it is enough to treat it with a special film spray (Opsite Spray) or cover it with a breathable film bandage (Opsite FlexiFix, Opsite Flexigrid). The dressing for wounds of medium size and depth should be sterile, impervious to moisture and microorganisms from the outside, and also facilitate the absorption of exudate and removal of excess moisture (Neofix Post, Opsite Post Op, Opsite Post Op Visible).
Humid environment.
It was previously believed that for a wound to heal quickly, it should be as dry as possible, but modern experience shows that for successful and rapid wound healing, a moderately moist environment must be maintained in it. In a humid environment, enzymes and growth factors are most active and cell growth and reproduction are more active, but excess moisture must be removed. Optimal moisture in the wound is maintained with breathable patches (Neofix Post, Opsite Post Op, Opsite Post Op Visible) when there is little exudate, or sponge dressings when there is a lot of discharge (Allevyn Adhesive, Non Adhesive).
WHAT TO DO?
- Assess the wound. Large, deep, bitten, scalped, lacerated wounds and wounds with heavy bleeding require qualified medical care; self-medication in this case is dangerous.
- Clean the wound - rinse with hydrogen peroxide, it will help remove small foreign objects, particles of dirt, non-viable tissue, and blood clots from the wound. If there is no hydrogen peroxide, then you can simply wash the wound with water or saline;
- Treat the edges of the wound. In this case, iodine or a solution of brilliant green (brilliant green) is suitable. To prevent wound infection, you can use a silver-containing dressing, Neofix Fibrotul Ag, fixing it on the wound with a patch or film type bandage (Opsite FlexiFix, Opsite Flexigrid);
- You can also simply cover the wound after treatment with a non-stick, breathable, moist dressing. Or a patch with the same properties. In this case, any adhesive bandage on a non-woven or film base (Neofix Post, Opsite Post Op) is suitable.
If the wound is small, then you need to do the following:
CONCLUSION OF WOUND EDGES
For additional fastening of the edges of a sutured wound, as well as for bringing together the edges of an incised wound after treatment, you can use LEUKOSTRIP adhesive strips. They reliably fix the edges of the wound, allow air to pass through, and remove excess moisture.
SUPERFICIAL WOUNDS, EXTENSIVE Abrasions
To ensure healing of a superficial wound, non-adhesive mesh dressings containing paraffin (Jelonet) are used as the primary wound covering. If there is a risk of wound infection, as well as to prevent infectious complications, a mesh dressing containing soft paraffin and an antiseptic (Bactigras) can be used as a primary wound covering. To remove excess fluid (exudate), an absorbent secondary layer is applied over the mesh bandage - a sponge bandage (Allevyn Adhesive, Allevyn Non Adhesive). Fixation can be achieved using a breathable film bandage (Opsite Flexifix, Opsite Flexigrid).
WOUNDS ON THE FACE
Wounds on the face require a special approach, since wound healing should lead to minimal cosmetic defects. For additional reduction of the edges of the wound, if the wound is sutured, or as a primary dressing, you can use special adhesive strips - strips (Leukostrip). The range of leading manufacturers of plasters includes a large number of simulated bandages (cut to size), with which you can carefully close the wound. If a scar has formed after healing, you can use a special silicone bandage that is designed to reduce and eliminate scars (Cica-Care). You can buy Cica-Care silicone patch here.
POST-OPERATIVE WOUNDS
We recommend covering postoperative wounds with specialized dressings. The structure of the dressing provides a favorable environment for healing and its painless change when dressing. Thanks to the inner layer, the bandage is securely fixed to the skin, but later it can be easily and painlessly removed. The middle, absorbent layer, consisting of viscose or polyurethane foam, ensures quick and reliable removal of exudate. The outer film or non-woven layer ensures rapid and constant evaporation of excess moisture. Among non-woven based dressings, we recommend using Neofix Post and Primapore. Among film-based dressings, Opsite Post Op and Opsite Post Op Visible have proven themselves to be excellent.
PURPUS WOUNDS
The presence of pus in the wound indicates that an infectious process has begun. Treatment of purulent wounds, especially large and deep ones, requires qualified medical care and an integrated approach. For such a case, we can recommend the following dressings: - For cleaning a wound with a dry, poorly detachable bottom (scab), or in the presence of a dense fibrin film at the bottom of the wound, hydrogel (Intrasite Gel) has proven itself very well. It must be applied to the surface of the wound, and then covered with a secondary film or sponge bandage. After 48 hours, the wound needs to be washed and cleaned. — For the treatment of purulent wounds, dressings with silver nanocrystals (Acticoat and Acticoat 7) have proven themselves to be excellent. Silver, acting as an antiseptic, is released gradually, providing a long-lasting and permanent effect. Acticoat dressing can be left on the wound for up to 3 days, Acticoat 7 for up to seven days. These dressings are primary; after application to the wound, they must be covered with a secondary absorbent dressing. Before use, silver-containing dressings must be moistened with distilled water or water for injection. Go to CATALOG OF BANDAGES
Preventive measures
In order not to look with disappointment at your reflection in the mirror and not to wonder how to get rid of allergies on your face once again, you should listen to the simple but effective advice of specialists.
- Adjust the daily menu by removing from the diet foods that provoke the appearance of characteristic symptoms of an immune disorder.
- Do not use cosmetics based on alcohol and other aggressive substances, giving preference to soft and neutral ones.
- Do not stay in the sun for a long time, and in winter, protect your skin from the cold as much as possible.
- During seasonal exacerbations of hay fever, use inhaled isotonic saline solutions to reduce the concentration of pollen in the nasopharynx.
- Always keep in your medicine cabinet an antihistamine recommended by an allergist-immunologist.
It is worth remembering that angioedema alone cannot be prevented. Other types of allergies are completely preventable, and this is much more effective than constantly treating exacerbations. Immunity support should take the leading place in the list of mandatory activities.
Why are allergies on the face dangerous?
A scattering of small specks or red spots not only look unsightly, but also pose a hidden threat. Acute inflammation, accompanied by swelling, can spread to the neck and make breathing difficult.
Violation of the structure of the skin, accompanied by a feeling of tightness, reduces the natural resistance to external influences. Weeping areas, as well as cracks in the upper layer of the epidermis, create a favorable environment for the proliferation of pathogenic bacteria, which leads to the appearance of pimples and ulcers. When such a condition occurs and is not treated, there is a high probability of it becoming chronic. In addition, an unpresentable appearance can cause a sensitive blow to pride and cause problems in communication.
If an allergic rash appears on the face, a specialist from a clinic or health center will tell you how to treat it. It is better to contact him at the first signs in order to make a timely diagnosis and receive an effective treatment regimen to avoid complications.
Symptoms of seborrheic dermatitis on the face
With seborrheic dermatitis on the face, symptoms appear:
- the appearance of pink, red or burgundy spots on the skin;
- the formation of white or yellowish scales and hemorrhagic crusts;
- peeling of the skin;
- irritation and increased sensitivity of the skin;
- itching and burning of varying intensity.
The course of the disease worsens in the autumn. In summer, unpleasant symptoms usually disappear.
If the ducts of the sebaceous glands become clogged, acne appears.
The disease is especially severe in men who grow beards and mustaches. Large plaques form under the hairline, which eventually transform into papules. If an infection occurs, then erythroderma is also detected. When papules coalesce, swollen areas colored red form.
The symptoms of seborrheic dermatitis are similar to those of other dermatological diseases. Therefore, only a doctor can make a correct diagnosis after a thorough examination of the patient.