Author: Brodsky Sergey Evgenievich Deputy Chief Physician, Candidate of Medical Sciences in the specialties: dentistry and medical microbiology In dentistry, almost all operations to build and restore the jaw bone contain the stage of installing membranes. Most patients who are planning to restore their eubs by installing implants and who learn more about all the stages of the operation are interested in why a membrane is used in bone grafting. Their use is required in case of acute deficiency of jaw bone tissue, if it is necessary to restore large volumes of it. The use of a membrane during implantation can successfully prevent the resorption of bone structures and eliminate bone atrophy, which creates favorable conditions for implantation of implants into it.
What is a dental membrane? Indications for installation
Dental (barrier) membranes are one of the achievements of modern dentistry, which is a thin film that is attached during the implantation procedure to the jaw, an area where bone tissue is actively destroyed. When asked frequently by patients about what bone membranes are made of, experts answer that they are most often made from collagen. The use of a collagen membrane in dentistry can effectively fix bone material, avoid further bone destruction and strengthen mobile teeth. The main indications for installing membranes are:
- a membrane is placed after tooth extraction to prevent bone tissue from shrinking;
- During bone grafting, a membrane is installed to form the missing volume of bone tissue;
- the membrane during sinus lift surgery, installed under the bottom of the maxillary sinus, reduces the risk of osteoplastic material getting into the maxillary sinus.
Types of membranes in dentistry
Today, the use of barrier membranes is the most environmentally friendly and most widely used method of strengthening deteriorating jaw bones. It is used much more often than complex bone grafting. There are several types of dental membranes:
Resorbable (resorbable). These membranes independently dissolve in the jaw tissue, so their further removal is not required. Dentists use 2 types of such membranes:
- synthetic polymers - their advantages are complete hypoallergenicity, no risk of infection transmission and long-lasting action for 5-6 months;
- xenocollagens of animal origin - have very high biocompatibility with jaw tissues.
Non-resorbable (non-absorbable). Dense dental films, which must be removed surgically, since they are not able to dissolve on their own during use. Installation of such membranes is necessary in case of significant destruction of bone tissue. There are also 2 types of them:
- frameless, used for average, up to 4 cm, lack of bone tissue;
- with a titanium frame are used for significant destruction of the jaw bones.
Membranes from the patient's blood plasma are also widely used . The plasma lifting procedure is carried out directly in the dental office and does not require special preparatory measures - the most important thing is to avoid alcohol, spicy and fatty foods on the eve of the procedure. The plasma lifting procedure itself is carried out as follows:
- Blood is taken from the patient’s vein;
- tubes with the resulting biomaterial are placed in a centrifuge for 10-40 minutes, depending on the platelet sedimentation rate of a particular patient;
- A thick clot of plasma is taken from the test tubes - it can be used in various manipulations - cut, sutured, etc.
Ready-made membranes can be stored for no more than 4 hours, so the procedure for their manufacture is carried out directly on the day of surgery.
Stages of membrane installation during implantation
Installation of dental membranes requires the surgeon not only to have operational skills, but also to have high qualifications and extensive experience. The technology of the operation consists of the following stages:
- administration of anesthesia;
- cutting and peeling of the mucous membrane;
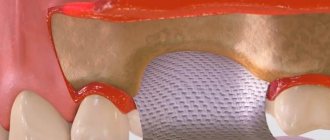
- filling the resulting hole with granules of bone material;
- installation of a barrier membrane for bone material granules.
In rare cases (during complex operations), the installed membrane is fixed with special small pins (buttons) and the gums are sutured. If a non-resorbable membrane is sewn in, surgery is repeated after some time to remove it.
Bone membrane: application in the Partner-Med clinic
It cannot be argued that the most important step before dental implantation is the choice of a clinic and a doctor. Today, a huge number of dentists offer this service, but not all of them will provide it with high quality. Dentistry Partner-Med is one of the few Moscow clinics where the patient will undergo this procedure with the highest quality. Our highly qualified specialists, many years of experience and regularly updated levels of professional training have thousands of successfully performed operations behind them.
Our dentists know in practice when to use a membrane when installing an implant, and will immediately determine which one is suitable for a particular patient. The level of professionalism of doctors is confirmed by numerous reviews from patients who are no longer ashamed of their smile.
Our additional advantages are:
- free initial consultation;
- individual selection of treatment;
- reasonable prices for services;
- permanent promotions.
Deputy Chief physician Sergey Evgenievich Brodsky
Sign up for a free consultation
+7
Just CALL US!
+7
We will answer any of your questions and will definitely help you!
In what cases are barrier and protective membranes applied?
Membrane linings perform several functions:
- Protective - protect the operated area from external factors.
- The role of the reinforcing material is to fix the osteoplastic material in a suitable position.
Applicable:
- when strengthening mobile units;
- to protect bone from atrophy after tooth extraction;
- when it is necessary to fix granules of osteoplastic material during osteoplasty before or during implantation;
- when building up the jaw bone with blocks.
The decision to use barrier membranes is made by the dentist after a preliminary examination.
To increase bone
An osteoplastic material is fixed under the gum, on top of which a protective pad is placed. It protects the bed and its contents from growing soft tissues. Eliminates washing out of the bone graft from the wound through the suture line. More reliable treatment results are provided by the use of a bone substitute along with two types of membranes. One of them covers the defect and osteoplastic material, and a collagen plate is placed on top of it.
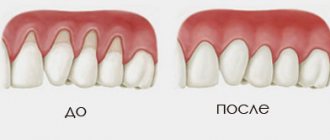
Gum extension (augmentation) during gum recession
Deficiency of soft tissues as a result of atrophy is characteristic of patients with long-term absence of teeth. Significant bone loss in such cases is accompanied by a proportional decrease in gum volume, which causes significant discomfort. Augmentation is more expensive and more difficult to install an implant. Gum augmentation can be performed with non-resorbable membranes, usually based on a non-porous material and resorbable, with a high rate of tissue compatibility. The method promotes rapid healing, reduces the risk of relapse and soft tissue swelling.
What is platelet fibrin
Human blood contains formed elements, one of which is transparent, anucleate cells - platelets. They take part in the process of blood clotting and stopping bleeding. During the destruction of the walls of a blood vessel, platelets, disintegrating, release components that form blood clots. In the 80s, an effective function was discovered: to increase the rate of healing and tissue restoration. This process occurs due to the release of growth factors (hormonal components) that enhance the regeneration of old cells, as well as the growth and increase in the number of new cells.
Platelet autoplasma is not only formed elements, but also saturated platelet fibrin. This is a yellowish liquid released when blood is processed in a special centrifuge.
It contains:
- platelets;
- fibrin;
- fats;
- hormones;
- nucleic acids;
- mineral components.
After the autoplasma is introduced into the jaw bone, growth factors are activated within a week. The tissues are intensively saturated with oxygen, and a dense capillary network is formed. The rate of restoration of jaw bone cells and their growth, as well as tissue nutrition, increases.
Human autoplasma is saturated with nutrients and is biocompatible with the body, because it is its own product. Consequently, engraftment is successful and side effects never develop. The restoration is proceeding as planned.
Types of biomaterials used
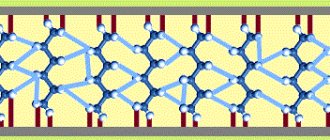
The method of directed tissue regeneration in surgical dentistry is based on the use of two main groups of membranes: resorbable (collagen, vicryl, polylactic acid, etc.) and non-resorbable (Gore-tex or titanium mesh, with titanium reinforcement, Teflon and others).
Resorbable
Installation of absorbable membranes prevents their removal after the osteoplastic material has engrafted. Such linings do not always remain stable over a long period. To enhance the prolonged action, their composition is supplemented with slowly resorbing substances. One of the main advantages of membrane linings is the possibility of enriching their structure with drugs that enhance osteogenesis, anti-inflammatory, antimicrobial agents, etc.
Types of resorbable membranes:
- Synthetic polymers (polyactides, polyglycolides) and their chemical modifications (for example, Guidor, EpiGuide, Vicryl) - decomposition into microscopic fragments that undergo phagocytosis occurs under the influence of hydrolysis. Among the disadvantages of the products, weak tissue integration and a high likelihood of developing swelling during resorption due to changes in pH in the tissues are noted. Advantages of polymer plates:
- no risk of transmitting an infectious disease;
- hypoallergenic;
- long-term effect (5-6 months).
Non-resorbable
They contribute to the effective restoration of bone in a given volume and trajectory, there are:
- Frameless - for restoration of bone tissue less than 4 mm.
- With a titanium frame - for bone restoration in large volumes, in all directions.
Main advantages:
- high mechanical strength;
- pronounced barrier properties.
These types of pads should be removed after 6-9 months . Consisting of titanium, they are effective in situations where there is a large load on the bone and it is necessary to protect implants or osteoplastic material. The most common indication for use is vertical ridge augmentation. They are removed after restoration of soft and bone tissues damaged during the operation.
Main disadvantages:
- risk of exposure - during suturing of the flap, the insert must be completely closed;
- absence of the process of periosteum formation under the overlay;
- the patient needs to visit the dentist frequently (every 2 weeks).
Statistics show that the most effective membranes are polytetrafluoroethylene (PTFE) GoreTex and aliphatic polyetherurethane (Bone-up). Less commonly used are mesh forms made of calcium sulfate (Capset) or titanium (Frios, BoneShield, Tiomesh).
Benefits of using blood plasma
The introduction of a platelet membrane naturally activates cellular growth factors of the jaw bone and periodontal tissues, increasing the rate of recovery. Regeneration and acceptance of implants or bone material by the body is much faster, and the likelihood of inflammation is significantly minimized.
Blood plasma membranes have a positive effect on:
- increase in the rate of cellular growth factor in the bone after implantation;
- absence of allergies that could occur when interacting with foreign materials;
- accelerated gum recovery after implantation or plastic surgery;
- prevention of inflammation around the implant;
- reduction of swelling and pain after surgical procedures;
- optimal tightening of the socket after tooth extraction;
- minimizing inflammation during gingival curettage and cleaning periodontal pockets.
Fixing elements of different types
The membrane is adjusted to the size of the defect, or the required dimensions are transferred to it using sterile templates in the package. The edges should overlap the boundaries of the bone defect by at least 2-3 mm . Fixation can occur in one of several ways:
- Before installation, the resorbable pad is pierced and placed on the implant using the rubber dam principle. The edges are secured with screws or pins into the bone, in which holes are previously created with burs. Additionally secured with sutures to the periosteum. When used on the upper jaw, titanium pins with a wide head are used for fastening.
- The self-curing mixture or film with an adhesive composition is fixed directly to the alveolar process.
- Non-resorbable plates are fixed with titanium pins or microscrews. The edges of the barrier must be tightly adjacent to the bone to prevent soft tissue ingrowth. When suturing the mucosa, small diameter suture material is used. The thread should pass along the edge of the membrane in contact with the neck of the implant. The stitching is done in the middle of the overlay between the edge stitches.
Opinion of a dentist-implantologist : “The success of implantation depends on how accurately patients follow medical recommendations. The operated area should be protected from hard, hot foods. Hygiene must be regular. Medications are taken only in consultation with a doctor.”
- Complete restoration of the dentition in just 4 days!
more detailsRoott Pterygoid Implants Sinus lift is no longer needed!
more details
Once and for life! Express implantation in 4 days with a permanent ReSmile prosthesis
more details
All-on-4, All-on-6, ReSmile, Zygomatic implantation We use all modern methods of dentition restoration
more details
How membranes take root during dental implantation
Collagen membrane overlays reduce the risk of complications due to loss of soft tissue. Non-stitched - due to the healing of soft tissues by secondary intention, the wounds are protected from the general inflammatory process. Both types integrate well into the jaw tissue. The bone under the surface of the barrier plate is regenerated in a manner similar to fetal bone growth.
When using absorbable overlays, the postoperative wound heals without the use of additional medications. Often the healing process of non-resorbable membranes is accompanied by complications, in particular, exposure of the structure. This can lead to infection and inflammation, which means it will have to be removed prematurely.
Often, under the barriers a favorable background is created for the development of microbes, so it is not always possible to achieve the desired result.
Membrane exposure after bone grafting - consequences and treatment
The non-resorbable membrane pad is exposed in 1% of cases , causing the following consequences:
- wound infection with the development of purulent inflammation;
- rejection of osteoplastic material during vascularization of the mucous membrane (in 40-50% of cases).
In such situations, it is recommended to remove the implanted materials, carry out treatment, and then repeat bone grafting. Typically, a second layer of soft tissue is formed under the incision using a mucoperiosteal flap. To do this, it is peeled off, split, modeled, and then sutured in layers.
The exposed resorbable pad should be treated with 3% hydrogen peroxide and 0.12% chlorhexidine. Sometimes this allows you to postpone the removal procedure by 8 weeks.
Opinion of a dental surgeon : “Most of my patients are smokers. Many people do not immediately realize the complexity of the situation caused by their bad habit. Smoking causes a sharp narrowing of the blood vessels in the mouth. This weakens the flow of blood filled with oxygen and nutrients. Due to their lack, the healing process is delayed. Therefore, you need to completely stop smoking at least a couple of weeks before implantation and for several months after it.”
Recommendations after plasma lifting
Plasmolifting is carried out in combination with other medical procedures. The duration of the rehabilitation period is determined depending on the disease and the medical procedures performed.
Recommendations for the patient to follow after treatment:
- limit physical activity during the recovery period;
- avoid exposure to high and low temperatures - baths, saunas, solariums;
- do not disturb the intervention site with your tongue and brush;
- maintain proper oral hygiene;
- temporarily eliminate hard and irritating foods and alcohol consumption.