Aphthous stomatitis is an acute inflammation of the oral mucosa with the formation of painful erosions (aphthous). Small round ulcers form on the inside of the lips, cheeks, tongue, tonsils, cause constant pain and affect overall well-being. Stomatitis is caused by a viral or bacterial infection, microtrauma of the mouth. But most often the disease develops against the background of stress or a decrease in the body’s defenses.
Causes of aphthous stomatitis
The exact cause of this disease remains unclear. It is assumed that HRAS is of an allergic nature; allergens can include: food, medicine, toothpastes, dust, worms.6,7 It is also assumed that the cause of the disease is an autoimmune reaction.8 A hereditary predisposition to this disease can be traced.
Predisposing factors:
- diseases of the digestive system (gastritis, gastric ulcer, cholecystitis, Crohn's disease)
- dysbacteriosis
- stress
- deficiency of iron, vitamins B1, B2, B6, B12, C
- chronic tonsillitis, otitis and rhinitis
Symptoms of the disease
Signs of aphthous stomatitis depend on the form and stage of the disease.
The following stages of aphthous stomatitis are distinguished:
- Initial.
- External manifestations.
- The appearance of pathological foci.
- Healing.
The initial stage is characterized by general malaise and enlarged lymph nodes in the neck, back of the head and jaws. The patient's body temperature rises and his appetite worsens, he feels weak.
At the stage of external manifestations, local symptoms (changes in the oral mucosa) join the above-described signs. These include:
- Edema.
- Pain, aggravated by eating and hygiene procedures.
- Redness and congestion with blood (hyperemia).
- Palpable itching.
The patient may also experience sleep disorders.
During the stage of appearance of pathological foci, single or multiple aphthae occur. They can develop on any part of the oral mucosa, but are most often observed on the cheeks, lips, palate and tongue. Ulcers are usually quite painful.
During the healing stage, the aphthae is gradually covered with epithelial tissue. In most cases, no scars are left.
Forms of aphthous stomatitis:
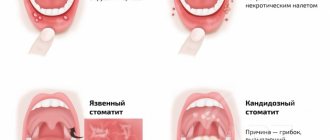
Fibrinous aphthous stomatitis is the mildest form, resulting from impaired circulation in the superficial layer of the mucous membrane. Single painful ulcers covered with a white coating appear in the mouth. Healing of aphthae occurs within 1–2 weeks.
The granular form develops due to a lack of saliva. With this type of disease, the minor salivary glands are affected, causing them to produce less secretion. Due to the dryness of the mucous membrane, painful and long-lasting ulcers occur near the excretory ducts of the glands. In patients prone to frequent colds, granular stomatitis can develop into a chronic form. The treatment is quite long - it takes from 1 to 3 weeks.
Necrotizing aphthous stomatitis is characterized not only by the presence of ulcers, but by the slow destruction of the outer layer of the oral mucosa, resulting in tissue death. Unlike other forms of the disease, this one is not accompanied by pain and discomfort. This type of pathology is rare. Necrotizing aphthous stomatitis is usually observed in adults suffering from any severe systemic diseases.
The scarring form occurs when the minor salivary glands and connective tissue are damaged, caused by genetic failures. The ulcers are small at first, but get larger over time. They are very painful. Aphthae in this type of disease are located in the projection of the salivary glands, mucous membrane of the pharynx and anterior palatine arches.
Deforming is the most complex form. It causes a lot of inconvenience to the patient, as it is accompanied by general malaise and significant pain. The ulcers are quite deep and do not go away for a long time. They lead to deformation of the lips, anterior palatal arches and the soft part of the palate. Microstoma (narrowing of the mouth) may also develop when the corners of the mouth are affected.
Reference! A complication of aphthous stomatitis is the spread of infection through the tissues, as well as the progression of the acute form to the chronic form.
HRAS classification:
| CAUSES | A COMMENT | ||
| causes: | Clinically, several forms of HRAS are distinguished: | a comment: | 1) fibrinous form: the size of aphthae is 2-3 mm, heal in 6-8 days 2) small canker sores (Mikulich’s aphthae): the size of aphthae is up to 1 cm, heal in 10-14 days 3) large Setton’s aphthae: the size of aphthae is from 1 to 3 cm, heal for a very long time, up to several months, leaving scars 4) herpetiform type: the smallest aphthae that merge |
| causes: | HRAS as a symptom of the disease: | a comment: | 1) Behcet's disease 2) Reiter's disease |
| causes: | According to severity, HRAS is divided into: | a comment: | 1) mild form: 1-2 aphthae, once every 2 years 2) moderate form: 3-6 aphthae, relapse 2 times a year 3) severe form: more than 6 aphthae, relapse several times a year |
Diagnostic features
At the initial appointment, the dentist examines the oral cavity and analyzes complaints. To make an accurate diagnosis, you need to distinguish this form of the disease from others, as well as differentiate it from other pathologies that have similar symptoms. For extensive lesions, different diagnostic methods may be used:
- clinical blood tests;
- microflora smear;
- blood for PCR to determine the causative agent of the disease;
- biopsy (if indicated).
They are also necessary for recurrent forms of the disease. In simple cases, laboratory diagnostics are not required; aphthae are determined visually by an experienced specialist.
With the help of a comprehensive examination, the doctor will determine which microorganism caused inflammation with subsequent ulceration of the mucous membrane. He also differentiates the disease from herpetic stomatitis and oncological pathology.
HRAS as a symptom of the disease
Behçet's disease is a disease of unknown etiology, characterized by vascular damage, the appearance of aphthae in the oral cavity and genitals, damage to the eyes, joints, gastrointestinal tract, central nervous system and other organs. It has a chronic course and, if left untreated, can lead to disability.9
Symptoms:
HRAS
HRAS is the earliest symptom of the disease; aphthae can be of any size, recur at least 3 times a year, and are often located on the mucous membrane of the cheeks, lips, gums, tongue
Eye damage
Uveitis (inflammation of the membrane of the eye), blurred vision, “fog” before the eyes, redness of the eyes (rarely), lacrimation
Genital ulcers
Similar to mouth ulcers, but deeper and more painful
Skin redness
The skin exhibits erythema nodosum (red, painful subcutaneous nodules), rash
Other
- vessels in the form of thrombosis, aneurysms
- Nervous system damage: coma, meningitis, confusion
- joints may also be affected in the form of arthritis
Reiter's disease is a systemic infectious disease characterized by damage to the oral mucosa, genitourinary system, eyes and joints.10 The triggering factor for infection is often chlamydia and gonococci, and there is also a genetic predisposition. The disease has a severe course, and in case of complications it leads to disability (blindness, deforming arthritis) and even death.
It is important to remember that HRAS may indicate the presence of a serious systemic disease.
Diagnosis of the disease and its differences from other pathologies
The doctor receives the first data after examining the patient’s mouth. Next, the doctor collects an anamnesis of the disease and the patient must answer when the first symptoms appeared, how quickly the disease developed, whether there were injuries (including burns) to the oral cavity, allergies to foods and medications, whether close relatives suffered from stomatitis.
To identify the causative agent of the disease, you will need to take a smear on the flora and exclude manifestations of herpes and candidiasis. For this purpose, laboratory tests are used - bacterial culture and PCR smear.
For persistent stomatitis, you should check your blood glucose level.
Prevention of HRAS
Prevention should be aimed at monitoring the state of health in general, treating chronic diseases, and it is necessary to undergo regular examinations regarding the existing disease. Hardening and strengthening the immune system have a good effect. You need to visit the dentist to monitor your oral health once every 3-4 months to ensure timely detection of relapses. You should avoid using toothpastes, hygiene products with dyes or identified allergens. Taking antibiotics should only be done under the supervision of a doctor. It is recommended to avoid strong psycho-emotional stress and regularly carry out wet cleaning of the premises.
It is worth paying attention to Tantum® Propolis .
Tantum® Propolis
Propolis has an immunostimulating effect, promotes healing, vitamin C, which is part of it, is responsible for regeneration, participating in the synthesis of collagen.
Propolis also has antiviral and antifungal effects. Therefore, vitamin therapy Tantum® Propolis is an effective means of preventing stomatitis12 Find out more
Features of treatment
The main goal of treating aphthous stomatitis is to completely get rid of the disease or at least reduce the frequency of relapses to a minimum. Therapy is aimed at relieving inflammation, relieving unpleasant symptoms, and accelerating the recovery processes of the mucous membrane.
For each specific case, the doctor will develop a set of measures. The main ones include local and systemic drug treatment.
Rinsing with antiseptics can be done using medications or mouth rinses that contain antibacterial components. An alternative to rinsing is to use a spray. Typically, the treatment regimen includes 2-3 sessions of 1-minute rinsing immediately after brushing your teeth.
Local treatment methods include the application of gels with anti-inflammatory and analgesic effects.
Occlusive agents can reduce pain and speed up the healing of mucous membranes. They form an insoluble film on the ulcer, protecting the affected area from exposure to adverse factors.
Local glucocorticoid therapy is used against the background of immune diseases, as well as when standard measures are ineffective. They eliminate pain and quickly relieve inflammation, shortening the healing period. Such products are used only according to indications and are available with a prescription. In some cases, it is advisable to inject the drug under the base of the ulcer; this is done by a doctor.
Epithelialization drugs are used after acute inflammation has resolved. The specialist will prescribe a gel with an analgesic and healing effect, usually this occurs 5–6 days after the start of complex therapy.
Local laser therapy can relieve pain, speed up the healing process, and minimize the risk of relapse.
Systemic treatment of aphthous stomatitis in adults involves taking the following drugs:
- antihistamines (anti-allergic, anti-edematous effect);
- glucocorticoids (anti-inflammatory, analgesic effect);
- immunomodulators (to stimulate defenses and accelerate recovery).
And if antiallergic drugs can be recommended to any patient even in the absence of information about the exact causes of stomatitis, then other drugs are prescribed only according to indications: in case of acute severe course of the disease, frequent relapses, and the presence of severe systemic pathologies. An additional method of treatment is vitamin therapy - taking vitamins C, group B.
In addition to the main course of treatment, all patients without exception are recommended to adhere to a hypoallergenic diet, avoid taking too hot drinks and dishes, and spicy, irritating foods. It is better to give preference to toothpaste without sodium lauryl sulfate, this component can provoke the disease.
It is important to continue your oral hygiene, even if it is difficult. To make brushing your teeth easier, choose a soft toothbrush. If the disease recurs frequently, it is necessary to pay attention to the general state of health, promptly treat teeth and gums, replace fillings and dental structures.
What systemic diseases can manifest as aphthae?
- Reiter's syndrome
- Behçet's disease
- AIDS
- cyclic neutropenia
- PFAPA syndrome
The gastroenterologist is especially interested in the connection between recurrent ulcers and specialized systemic diseases.
Celiac disease is found in 5% , and for a long time canker sores may be the only manifestation of a reaction to gluten.
Let me remind you that the estimated prevalence of celiac disease in the general population is about 1%.
Enamel defects and aphthous stomatitis in celiac and healthy subjects: Systematic review and meta-analysis of controlled studies
Other important conditions that manifest as canker sores are inflammatory bowel diseases: Crohn's disease and ulcerative colitis.
Extraintestinal Manifestations of Pediatric Inflammatory Bowel Disease: Prevalence, Presentation, and Anti-TNF Treatment
Conclusions:
Aphthae in the mouth recur at some point in life in almost 20% of all people, most often in the second decade of life.
It is difficult to establish a clear and unambiguous reason.
If recurrent aphthae occurs, the pediatrician, physician, or dentist should consider the possibility that rare aphthae are a manifestation of a serious systemic disease.
In such situations, the gastroenterologist must exclude celiac disease, Crohn's disease and ulcerative colitis.
5, total, today
Symptoms
The disease has rather sparse symptoms. Visually, it is easy to identify by the presence of characteristic ulcers on the inside of the lips, cheeks, soft palate and tongue (rarely). Keratinized (fixed) gums are not affected by aphthous stomatitis, which is another difference between aphthous stomatitis and herpetic stomatitis. At the initial stage of aphthae, the patient usually feels discomfort and burning, and the temperature may rise slightly. Diagnosis involves a visual examination, as well as taking blood tests and mucosal smears if the doctor suspects the presence of concomitant diseases.
Acute and chronic
According to the nature of the disease, aphthous stomatitis is divided into acute and chronic.
- Acute aphthous stomatitis. It occurs suddenly, most often due to viral infections and increased concentrations of staphylococci in the blood. Almost immediately, pain occurs and round-shaped aphthae are formed, covered with a grayish coating and having a characteristic red border. The pain makes it more difficult to eat and, in some cases, talk. With timely treatment, the causative agent of aphthous stomatitis is destroyed within 10-12 days, and the epithelial layer at the site of aphthous stomatitis returns to its normal state.
- Chronic (recurrent) aphthous stomatitis. It has been getting worse regularly for many years. This form of the disease occurs in the presence of chronic diseases, as well as under the influence of genetic factors. Recurrent aphthous stomatitis is often accompanied by fever and enlarged lymph nodes. Swelling is observed in the area where afts occur. If left untreated, ulcers begin to grow into the deeper layers of the mucosa: this process is accompanied by slight bleeding and severe pain.
Literature:
- Aphthous stomatitis. Nurse, No. 5, 2015, p. 21.
- Mikhalchenko V.F., Firsova I.V., Fedotova Yu.M. and others. A new approach to the treatment of chronic recurrent aphthous stomatitis (Setton's aphthosis) using the method of photoactivated disinfection and the immunomodulator Galavit. Modern problems of science and education. No. 6, 2015, pp. 1-6.
- Salomão Israel Monteiro Lourenço Queiroz, Marcus Vinícius Amarante da Silva. Ana Miryam Costa de Medeiros. Recurrent aphthous ulceration: an epidemiological study of etiological factors, treatment and differential diagnosis. (Recurrent aphthous ulcers: epidemiological study of etiological factors, treatment and differential diagnosis). An Bras Dermatol. 2018;93(3):341-6.
- Maksimenko P.T., Skripnikova T.P., Khmil T.A. Nomenclature, clinical classification of diseases, changes in the mucous membrane of the oral cavity, lips and tongue. Ukrainian Dental Almanac, 2008, No. 4, pp. 28-36.
- Sunday O. Akintoye, BDS, DDS, MS* and Martin S. Greenberg, DDS, FDSRCS. Recurrent Aphthous Stomatitis. Dent Clin North Am. April 2014; 58(2): 281–297. doi:10.1016/j.cden.2013.12.002
- Galizina O.A. Main aspects of the occurrence, clinical manifestations, treatment and prevention of chronic recurrent aphthous stomatitis. Russian Dental Journal, 2014, No. 6, pp. 39-42.
- Mahesh Chavan1, Hansa Jain2, Nikhil Diwan1, Shivaji Khedkar3, Anagha Shete1, Sachin Durkar. Recurrent aphthous stomatitis: a review. J Oral Pathol Med (2012).
- Volkov E.A., Butova V.G. Clinical recommendations (treatment protocol) for chronic recurrent aphthous stomatitis. Russian Dental Journal, No. 5, 2014, pp. 35-50.
- Instructions for medical use of the drug Metrogyl-Denta®.
- Strakhova S.Yu., Drobotko L.N. Chronic recurrent aphthous stomatitis (lecture). RMZh, No. 29 dated December 27, 2006, p. 2096.
- Dental gel for gums Metrogyl-Denta® in the treatment of periodontal diseases and oral mucosa. Practical medicine, No. 1(33), March, 2009, pp. 105-106.
- Glukhmanyuk D.S., Malinovsky V.A. Aphthous stomatitis. Proceedings of the scientific and practical conference “Modern problems of pharmacology, cosmetology and aromology.” International Humanitarian University, Odessa Medical Institute, 2015. – 48 p.
Dentists' recommendations
Prevention of aphthous stomatitis is the surest way to prevent the disease in children. Parents of children with a hereditary predisposition, chronic diseases or weakened immunity should pay the greatest attention to preventive measures.
To reduce the risk of developing aphthous stomatitis, dentists recommend:
- monitoring the child's nutrition;
- exclusion of allergenic products (if indicated);
- periodic intake of vitamin complexes;
- maintaining oral hygiene at home;
- professional teeth cleaning every 6 months;
- timely treatment of dental diseases;
- treatment of any provoking diseases;
- contact your dentist at the first symptoms of aphthae.
Aphthous stomatitis is a complex dental disease caused by infection. Treatment of infectious pathology at home often only helps to eliminate symptoms and transition of the disease to a chronic form. Contacting a qualified dentist will allow you to individually select treatment tactics for complete recovery or achieve long-term remission with subsequent “attenuation” of the infection.