After tooth extraction, especially if the procedure was complex, there is inflammation, swelling, suppuration in the mouth, you want to speed up the healing process of the wound and avoid complications from the appearance of pathogenic bacteria in it. To achieve this, surgeons often recommend mouth rinsing after surgery. But this does not always happen - sometimes the doctor will advise you not to do this.
Why is that? What is the correct way – when and with what to rinse your mouth after tooth extraction, and whether to rinse? We're talking to the doctors at the Family Smile dental clinic.
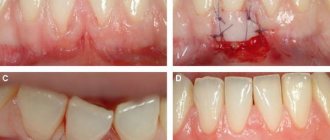
How gums heal after tooth extraction
It is worth knowing the specifics of the process in order to understand what is considered normal and what is not, and whether it is worth contacting the dentist again.
The average tissue recovery time is 10-15 days. During this period, the pain goes away, and new mucous gum tissue appears in place of the hole.
It all happens like this:
In the first two to three hours after the manipulation, the gums may bleed, and a thrombus will form in the socket - a blood clot that closes the wound from the penetration of bacteria. You shouldn’t injure him or try to spit him out.
Up to three days after the operation, the blood clot gradually thickens, decreases, and connective tissue begins to form inside the wound.
Three to seven days after the operation, the clot becomes lighter, and the hole is covered with young connective tissue. Pain and swelling go away.
After one to two weeks, bone tissue begins to form under the gum, in place of the extracted tooth.
After a couple of weeks, superficial healing is complete.
The timing may vary depending on the specific case and the patient’s health condition.
Do not ignore:
swelling, pain, bloody or other discharge from the socket that does not go away for more than 4 days.A “dry” socket is a deep cavity in the gum without a blood clot, but with a yellowish-gray, greenish, white coating and the smell of rotting.
Difficulty opening the mouth, clicking, pain in the temporomandibular joint that appeared after removal and did not go away within 2-3 days.
Numbness in parts of the gums and cheeks that did not go away after the anesthesia ended.
Runny nose, nasal congestion, and fever that appeared after removal.
In these cases, be sure to consult your doctor again.
Contraindications and some features of the use of Miramistin
The drug is not used in case of hypersensitivity to benzyldimethyl ammonium chloride. Patients diagnosed with a catarrhal form of gastritis, which is provoked by an imbalance of the positive microflora of the gastrointestinal tract, should use the solution carefully. Miramistin enhances the effect of antibiotics. When using drugs together, it is necessary to adjust their dosages. The likelihood of adverse reactions occurring when taking the solution is very low.
The use of Miramistin for more than a week is not recommended, since it has an aggressive effect on the microflora of the oral cavity. Otherwise, the number of beneficial bacteria on the mucous membrane will decrease significantly. She will become vulnerable to various diseases. For example, stomatitis may develop.
With rinsing, the pain subsides on the second or third day. Bleeding should be minimal. The saliva may be slightly pink in the first two days. If you feel worse when rinsing, or local symptoms increase rather than go away, you should visit your doctor.
How to rinse your mouth after surgery
Ready-made pharmacy antiseptics and solutions made independently at home are applicable. Let's consider how to rinse your mouth after gum surgery or tooth extraction.
Your doctor may recommend not rinsing the wound on the day of surgery. Every other day, you can make oral baths with decoctions of chamomile, sage, or solutions of furatsilin, 0.05% chlorhexidine.
There are quite a few such drugs, and your doctor will give specific recommendations on what to rinse your mouth after gum or tooth removal. The choice of a suitable drug depends on the condition of the hole, the complexity of removal, the age of the patient, whether he has allergies or sensitivity to some components of the products.
Carefully! It is not recommended to use ethyl alcohol, hydrogen peroxide solution, brilliant green or iodine for rinsing. They can cause pain, burn the mucous membrane and lead to the detachment of a fresh clot.
What do doctors recommend?
For several days, it is necessary to rinse the oral cavity with an antiseptic solution, which will prevent the entry of microbes from the external environment through the wound surfaces of the gums. The number and duration of rinses is determined by the attending physician. Rinse solutions should be no cooler than room temperature and no hotter than 37 degrees. The simplest and most inexpensive option is a solution of baking soda (1 teaspoon per glass of water). In addition, rinsing can be done using pharmaceutical products.
Rinses from the pharmacy
| Iodine-containing products | Iodinol, yox (spray) |
| Chlorine-containing | Chlorhexidine, miramistin, eludril, |
| Nitrofuran | Furacillin |
| Based on hexetidine | Stomatidin, hexoral |
| Vegetable | Chlorophyllipt, calendula tincture, |
| Antiseptic lozenges | Faringosept, septolete, grammidin |
| Means to accelerate the healing of mucous membranes | Rotocan, dental paste solcoseryl, stomatophyte, propolis spray, sea buckthorn oil. |
| Infection Control Products | Antibiotics, bacteriophages (staphylococcal bacteriophage, pyobacteriophage) |
How to rinse your mouth after tooth extraction
The main rule is not to rinse your mouth too vigorously. Immediately after tooth extraction, you should do oral baths rather than vigorous rinsing. Rinsing vigorously may cause the fresh clot to fall out of the socket. Bleeding will occur and healing will be delayed.
How to rinse your mouth with Chlorhexidine after tooth extraction? Let's use the example of this popular tool. First, rinse the mouth with warm boiled water to remove any remaining food. Then we put 15-20 ml of the drug into the mouth and hold it for 15-30 seconds. On the second or third day after removal, gentle rinsing movements are allowed. Spit and repeat 2-3 more times. The number of rinses during the day is 3-6.
How much to rinse your mouth after tooth extraction depends on how the healing is progressing. You can stop rinsing when young gum tissue has formed at the site of the hole.
Why is processing important?
Typically, a tooth is removed if it is so damaged that it cannot be restored. That is, both its visible part and the root are damaged, and at the same time it is not possible to install a reinforcing pin for subsequent prosthetic restoration with a crown. This procedure is possible only when the thickness of the root walls is at least 2 millimeters. If it has been severely damaged by caries, then the tooth has to be removed completely.
What is caries? This is rot, consisting of a mixture of bacteria. If even a small part of them gets into the wound left after tooth extraction, a purulent sac will certainly appear there. Moreover, all this can happen even without a pain symptom, because the dental nerve usually dies before this moment.
If the pus subsequently breaks out, it may result in blood poisoning. There are also cases where, due to bacterial infection of the wound after tooth extraction, the rotting process transferred to the jaw bone. As a result, part of it had to be removed.
And in order to prevent the above complications, the wound is treated with antiseptics and anti-inflammatory drugs. Miramistin solution (0.01%) is ideal for this, since it is active against bacteria, fungi, viruses, and at the same time strengthens local immunity and prevents the activation of the inflammatory process.
How to eat after tooth extraction
There is an opinion that it is better to fast for the first day after surgery and drink through a straw so that liquid does not get into the wound.
In fact, everything is not so: You can already eat 2-3 hours after the manipulation - the body needs strength to recover. For several days, you should include slightly warm, soft foods in your diet and avoid hard, spicy, too cold or hot foods. Optimal choice: puree soups, milk porridge, stew.
You can drink immediately after removing the cotton swab from your mouth. Contrary to popular recommendations, you should not drink through a straw - when you retract your cheeks, a vacuum effect is created, which can tear the clot from the wound.
The dentist will talk about the main points in oral care after surgery and answer questions after the procedure. Follow the recommendations so that you don’t encounter complications and healing goes quickly!
Types of stomatitis in adults
Effective treatment of stomatitis in adults begins with the diagnosis of pathology. Identifying the provoking factor is one of the main tasks of the dentist. The situation is aggravated by the fact that many reasons are similar - they overlap each other, distorting the clinical picture. For this reason, only experienced doctors treat stomatitis in adult patients.
There are a variety of classifications of stomatitis:
- according to the course - acute periodic, chronic, recurrent;
- by external manifestation - redness, aphthae, erosion;
- by localization - on the lip, on the tongue, on the palate, in the throat.
When diagnosing and selecting a treatment plan, dentists try to take into account the versatility of the disease - the form, causes, degree of damage to the mucous membranes, stage of the disease, and other classification parameters. Based on these factors, it is customary to identify the most popular types of stomatitis in adults:
- aphthous;
- ulcerative;
- herpetic;
- candida;
- prosthetic;
- allergic;
- ray.
Aphthous stomatitis
Aphthous stomatitis is characterized by the appearance of round ulcerative formations covered with necrotic plaque. This is the most common variant of the disease - it occurs in 65-70% of dental patients.
The causes of aphthae formation are viral and bacterial diseases. Localization of ulcers is on almost any mucous tissue of the oral cavity.
Initially, the patient is faced with the fibrinous form, when local blood circulation is disrupted. If left untreated, the disease turns into a necrotic form, accompanied by tissue death, or into a scarring form - the mucosal tissue changes structure.
Ulcerative stomatitis
Ulcerative stomatitis is characterized by the formation of deep, painful ulcers in the mouth. They usually arise due to:
- poor hygiene - a large amount of plaque on the teeth, tartar;
- problems with the gastrointestinal tract - metabolic disorders;
- chemical burns - abuse of especially spicy foods.
Lesions affect the deep layers of tissue, so treatment of ulcerative viral or bacterial stomatitis in adults is carried out only by a dentist according to a carefully developed plan.
A separate type of ulcerative stomatitis is ulcerative-necrotizing gingivitis, Vincent's stomatitis. The cause of the disease is the active proliferation of pathogenic microflora, the influence of spindle bacillus and Vincent's spirochete. The disease is observed against the background of a sharp decrease in immunity and is characterized by reactive development. Patients complain of swelling of the gums, suppuration, pain, putrid breath, and loss of appetite. Without treatment, tissue necrosis progresses and tooth roots are exposed.
Herpes (herpetic) stomatitis
Viral herpetic stomatitis is a contagious variant of the disease provoked by the herpes virus. Transmitted through hygiene items, through negligence, by airborne droplets.
Externally it differs from other types, since the lesions look like fluid-filled blisters before turning into ulcers.
During treatment, the doctor conducts complex therapy, including taking medications.
Candidal stomatitis
The cause of candidal stomatitis is a fungus that causes the appearance of a cheesy coating on the oral mucosa. Underneath the plaque is a swollen, inflamed area. When the formations are removed, the tissue surfaces begin to bleed.
The causes of the disease are decreased immunity and poor hygiene. Treatment requires careful selection of drugs so as not to aggravate the situation.
Prosthetic stomatitis
The pathology is typical only for adult patients, as it is a consequence of improper prosthetics, individual intolerance to the crown material, and poor quality of care for the orthopedic product.
The disease manifests itself as inflammation of the soft tissues around the prosthetic structure, turning into ulcers and erosion.
Allergic stomatitis
A distinctive feature of the disease is dryness and itching in the mouth. This is how increased sensitivity to allergens manifests itself. At the site of the inflamed areas, aphthae and ulcers quickly form. In severe cases, an ulcerative-necrotic form may develop.
Pathology happens:
- acute - single manifestation;
- chronic - with constant relapses and complications.
Treatment requires an integrated approach.
Radiation stomatitis
The reason for the appearance is the patient undergoing radiation therapy or chemotherapy and, as a result, a decrease in immunity. It occurs acutely - with inflammation and ulcers. Requires careful attention from the doctor during treatment to avoid worsening the situation.