Effective treatment of stomatitis in adults
Treatment of stomatitis in adults largely depends on the type of this disease, as well as concomitant diseases that provoke the appearance of ulcers and inflammation in the mouth. The most interesting thing is that the diagnosis of stomatitis is still carried out visually: the patient undergoes tests only if other, more serious diseases are suspected. Effective therapy for stomatitis is possible, but only if the type of disease is correctly determined. Recovery usually occurs within one or several weeks, but there are also more severe forms when long-term rehabilitation is required for complete recovery. Let's look at the main types of disease and drugs for the treatment of stomatitis in adults.
Diagnostics
If a mucosal lesion occurs in the mouth, the patient is examined by a dentist, infectious disease specialist or pediatrician. To identify the cause of the disease, measures are taken to identify the causative agent of the disease.
The following diagnostic methods are used:
- linked immunosorbent assay;
- cytopolymerase reaction;
- tank sowing discharge from ulcers, pieces of mucous membrane and plaque;
- cytological, immunological research methods.
If candidal stomatitis is suspected, an endocrinologist is consulted and tests are performed to detect diabetes mellitus.
In chronic forms of the disease, the following is carried out:
- tests for worm eggs;
- Ultrasound of the abdominal area;
- immunogram;
- stool examination for dysbacteriosis.
Consultations with a gastroenterologist and immunologist are carried out.
Treatment of herpetic stomatitis
Treatment of stomatitis after detection can be carried out many times (once a year or more often), since once settled in our body, the herpes virus remains there for life. Herpes stomatitis is characterized by the accumulation of reddish transparent blisters on the lips and inside the mouth, so it is quite easy to detect. Especially often, herpetic stomatitis manifests itself against the background of decreased immunity, vitamin deficiency, hypothermia and stress. Remember that herpetic stomatitis in adults is contagious, so you should avoid tactile contact.
Types of drugs
- Antiviral agents.
- Immunostimulants (as a preventative measure).
- Ointments (including to eliminate visual manifestations of the disease).
Prevention
The occurrence of stomatitis is much easier to prevent. To do this, just follow simple rules.
Recommended:
- clean your mouth twice a day under parental supervision;
- regularly take your child to the dentist for preventive examinations;
- promptly treat dental caries;
- avoid injury to the oral mucosa;
- timely treat all somatic diseases in the baby;
- disinfect dishes and toys;
- prohibit the baby from putting dirty objects and hands in his mouth.
Stomatitis has different origins and is caused by different pathogens. Therefore, only a doctor should treat these diseases. Self-medication is unacceptable, since a thorough diagnosis is necessary before treatment. Identification of the causative agent of the disease is a condition for successful treatment.
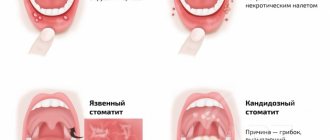
Treatment of candidal stomatitis
A type of stomatitis that is caused by a special type of fungus – Candida albicans. Very often, candidal stomatitis begins with glossitis, which is why its second name is stomatitis on the tongue. Treatment in this case requires fairly prompt treatment, since in adults it is quite painful and is accompanied by a burning sensation in the mucous membrane and sore throat. On the inner surface of the lips and cheeks, as well as on the tongue, characteristic foci of inflammation appear, covered with a white cheesy coating.
Treatment methods
- Treatment of common diseases (if detected).
- Antimicrobial therapy.
- Preventive rinses.
Treatment of aphthous stomatitis
A distinctive feature of this type of stomatitis is the appearance of so-called aphthae on the oral mucosa. These are small round ulcers with redness at the edges, the touch of which causes unpleasant painful sensations. Often occurs as a result of the activity of microorganisms (in particular, staphylococcus). Treating aphthous stomatitis at home is only recommended if it is not caused by a more severe illness. Often aphthous stomatitis occurs with problems with the immune system, liver and gastrointestinal tract.
Treatment methods
- Allergy therapy.
- Antiseptic therapy (treatment of aphthae with anti-inflammatory solutions, gels and ointments).
- Dental treatment and sanitation of the oral cavity (after dental treatment, stomatitis occurs less frequently than in the presence of carious lesions).
- Immunotherapy.
- Diet.
Causes of stomatitis
Many factors contribute to the development of stomatitis. One of the common causes of the disease is the action of an irritant . The mucous membrane can be affected by constant mechanical trauma (biting the cheeks and tongue, trauma from tartar, incorrectly made prosthesis or crown) [5]. Injury can be caused by exposure to a thermal or chemical agent, for example, when a mucous membrane is burned by hot food or when an allergy occurs to certain foods (for example, citrus fruits) or medications. The risk group includes smokers, since nicotine also acts as an irritant to the mucous membranes.
Oral hygiene plays a major role in the development of stomatitis. With improper oral care, plaque and tartar accumulate; the microorganisms present in them (staphylococci, streptococci) can cause irritation and inflammation of the oral mucosa. As a result, stomatitis occurs as a protective reaction of the body.
Sometimes inflammation of the mucous membrane occurs in various chronic diseases and pathologies with an unclear etiology (cause). Stomatitis can manifest itself in the oral cavity against the background of diseases of the gastrointestinal tract (with helminthic infection), cardiovascular system, blood diseases (anemia), endocrine disorders (diabetes mellitus). Very often, stomatitis develops during HIV infections and can be one of the diagnostic signs when identifying HIV.
Reason/Example
| Fungal infections | ⠀•⠀Candidiasis |
| Bacterial infections | ⠀•⠀Acute necrotic ulcerative gingivitis ⠀•⠀Syphilis ⠀•⠀Tuberculosis |
| Viral infections | ⠀•⠀Chicken pox ⠀•⠀Herpes simplex virus |
| Physical factors | ⠀•⠀Poorly fitting denture ⠀•⠀Improperly made crown ⠀•⠀Improper bite ⠀•⠀Biting cheeks and lips ⠀•⠀Tartar |
| Medicines | ⠀•⠀Antibiotics ⠀•⠀Barbiturates ⠀•⠀Chemotherapy drugs |
| Allergens | ⠀•⠀Occupational exposure to dyes, acid fumes, heavy metals ⠀•⠀Allergic reaction to food |
| Chronic diseases | ⠀•⠀Diabetes mellitus ⠀•⠀Anemia ⠀•⠀HIV infection |
If you notice similar symptoms, consult your doctor. Do not self-medicate - it is dangerous for your health!
Causes of acute stomatitis
Acute stomatitis occurs most often after damage to the mucous membrane or against the background of a viral disease. Injuries create favorable conditions for the proliferation of pathogenic microorganisms, including the herpes virus. Stomatitis in adults usually has a herpetic form.
Relapses of the inflammatory process usually occur in the cold season, when acute respiratory viral infections, in particular influenza, progress. This coincidence is not accidental. Viral diseases contribute to the appearance of stomatitis in adults and children.
Causes of chronic stomatitis
Chronic stomatitis in the oral cavity regularly worsens. In the summer, a temporary remission is observed. Chronic inflammation is caused by concomitant pathologies of the endocrine system, digestive tract, and diseases of an autoimmune nature. Dental diseases, including caries, periodontal disease, and gingivitis, also contribute to the protracted course of the inflammatory process.
Treatment of stomatitis with folk remedies
Treatment of diseases, especially in the early stages, is possible at home. How is stomatitis in the mouth treated in adults ? Anti-inflammatory and healing folk remedies:
- chamomile with honey;
- burdock root and chicory herb;
- grated raw potatoes (keep in mouth for 5-7 minutes);
- yarrow decoction;
- crushed burdock seeds;
- garlic mixed with curdled milk (or sour cream).
If your body lacks vitamins, you can prepare a vitamin salad.
Burdock leaves, horseradish roots, green onions, sour cream and salt are added to it. Effective treatment of stomatitis at home is possible. The patient must also:
- perform daily oral hygiene;
- follow a diet;
- limit alcohol consumption;
- give up sweets, chips, crackers.
There is a high probability of this disease appearing again. But if you carry out the right treatment, this will not happen.
How to treat stomatitis in children?
Parents who discover ulcers in their child’s mouth are required to contact a pediatric dentist. The following will help prevent the spread of infection:
- limiting contact with other children;
- allocation of separate dishes;
- own personal hygiene items.
The course of therapy consists of taking medications:
- painkillers;
- antiseptic;
- antiviral;
- healing.
How to treat stomatitis in children ? Allowed to process places:
- Oxolinic ointment. Apply 2-3 times daily.
- Acyclovir. The interval between applications is 8 hours.
- Tebrofen gel. No more than 4 times a day.
Pain-relieving ointments can be used. For example, Lidochlor and Kamistad (allowed for 3 months).
Ointments and gels
1. Acyclovir An antiviral drug that has a highly selective effect on herpes viruses. In case of herpes, it prevents the formation of new rash elements, reduces the likelihood of complications, accelerates the formation of crusts, and reduces pain in the acute phase of herpes zoster. The ointment is applied to the affected areas of the skin 4-6 times a day (as early as possible after the onset of infection). Cost: up to 220 rub.
2. Metrogyl denta
A combined antimicrobial drug, the effectiveness of which is due to the presence of two antibacterial components in its composition.
For aphthous stomatitis, the gel is applied to the affected area of the oral mucosa 2 times a day for 7-10 days. The drug is contraindicated in people under 18 years of age. Cost: up to 300 rub.
3. Oxolinic ointment Demonstrates antiviral activity against herpes simplex viruses, herpes zoster, and influenza viruses (mainly type A2). For external use. Non-toxic, non-irritating if the required amount and concentration have been applied and the skin at the application site has not been damaged. Cost: up to 100 rub.
4. Vinilin is a drug that has an antimicrobial, anti-inflammatory, enveloping effect, promotes the cleansing and healing of wounds and ulcers. The antimicrobial effect of the drug inhibits the growth and development of microorganisms. Envelops and regenerates. Vinilin acts as a local anesthetic. Vinylin is usually prescribed by dentists for the treatment of stomatitis, because it has not only antimicrobial, antiviral and antifungal effects, but also healing. A protective film is formed, which protects the wound from irritation upon contact with products, thereby reducing pain. Vinilin does an excellent job of treating stomatitis, but it should be used as prescribed by a dentist. Suitable for any type of stomatitis. Cost: up to 200 rub.
1. Anaferon Lozenges. Immunomodulatory agent. When used prophylactically and therapeutically, it has an antiviral effect. It is used for complex treatment of infections caused by herpes viruses, as well as acute and chronic viral infections. Allergic reactions and increased individual sensitivity to the components of the drug are possible. Contraindications include individual sensitivity to the components of the drug. It is not recommended for use by people with congenital lactose deficiency syndrome. Cost: up to 240 rub.
2. Immunal The drug is in the form of drops for oral administration. Used in cases of decreased immunity, stimulates the immune system in uncomplicated acute infectious diseases. Contraindicated during breastfeeding without prior consultation with a doctor. Cost: up to 340 rub.
3. Givalex Antibacterial and antifungal agent. It has a bacteriostatic and weak bactericidal effect. The drug is in the form of a spray and solution in bottles. It is used as a means for the local treatment of infectious and inflammatory lesions of the oral cavity and pharynx, which are caused by microflora that are sensitive to the action of the drug. It is used to prevent the development of infectious and inflammatory lesions after dental surgery. During pregnancy, use according to strict medical indications. If breastfeeding, use of Givalex should be discontinued. Cost: up to 150 rub.
4. Clotrimazole
Clotrimazole is an antifungal medicine.
Has a wide range of antifungal effects. The active ingredient of the drug is an imidazole antimycotic agent. . This medicine is effective against dermatophytes and yeast fungi. In addition, the drug has an antimicrobial effect. Clotrimazole should not be used if you are hypersensitive (allergic) to clotrimazole, its auxiliary ingredients, or in the first trimester of pregnancy. Cost: up to 360 rub.
5. Ketotifen Ketotifen is produced in tablets and syrup. The main ingredient of the product is ketotifena fumarate. The drug is intended for long-term use. The maximum effect can be achieved only after several weeks of treatment. The average course of therapy can last from 2 to 3 months. Discontinuation of the drug is carried out gradually - from 2 to 4 weeks. Ketotifen is not prescribed to those whose profession involves driving vehicles or potentially dangerous machinery. Cost: up to 100 rub.
6. Tavegil Tavegil in solution for injection is used in the prevention and treatment of pseudoallergic and allergic reactions. Tavegil is not prescribed to patients undergoing treatment with monoamine oxidase inhibitors. In addition, the drug is not prescribed to patients with damage to the lower respiratory system. Cost: up to 200 rub.
Drugs that accelerate the healing of the mucous membrane
1. Vitamin A Has a general strengthening effect, normalizes tissue metabolism, and participates in redox processes. Increases the body's resistance to infection. The drug is taken orally early in the morning or late in the evening, 10-15 minutes after meals, 1 capsule 1 time per day. Long-term daily use can cause intoxication, hypervitaminosis A (headache, nausea, vomiting). Contraindicated during pregnancy and breastfeeding. Cost: up to 100 rub.
2. Sea buckthorn oil Oil preparations always act more gently than aqueous or alcoholic medicinal solutions. This oil can be used if there is no allergy to natural oils. Treatment is carried out by lubricating the areas of erosion a maximum of three times a day. A cotton swab or disk should be dipped in oil and then applied to the mucous membrane. Cost: up to 150 rub.
Anti-inflammatory drugs, antiseptics
Anesthetic (painkiller) drugs dull pain in the mouth for a short time. 1. Hexoral Antiseptic for topical use in ENT practice and dentistry. The drug has a wide spectrum of antibacterial and antifungal effects, in particular against gram-positive bacteria and fungi of the genus Candida. It is prescribed as a symptomatic remedy. The drug is sprayed into the mouth or pharynx, and the affected areas are treated while holding your breath. One injection for 1-2 seconds 2 times a day. The duration of treatment is determined by the doctor. Cost: up to 310 rub.
2. Lidocaine Asept Available in aerosol form. The drug can be used for local anesthesia in dentistry. Apply topically, externally. The dosage varies depending on the doctor's indications. You can also apply it using a cotton swab soaked in it. Contraindications include hypersensitivity to lidocaine. Cost: up to 280 rub.
3. Decathylene Has antibacterial and antifungal effects. Affects microorganisms that cause mixed infections of the mouth and throat. Decathylene does not contain sugar, so it is suitable for people with diabetes. Recommended for aphthous stomatitis. Contraindications – hypersensitivity to any of the substances that are part of the drug. Cost: up to 1300 rub.
Prevention
Prevention helps avoid relapses of stomatitis. First of all, it is worth protecting the mucous membrane from the action of aggressive factors: poor-quality hygiene products, cold or, conversely, scalding food, traumatic dentures and uneven edges of teeth, cigarette smoke, and alcoholic beverages.
Strengthening local immunity plays an important role in preventive measures. The oral mucosa is a protective barrier. If the normal microflora is disrupted, the number of potentially dangerous infectious pathogens increases, they actively multiply and cause a response - an inflammatory process.
To strengthen the immune system, you can use natural factors (hardening with water, sun, air) or natural and artificial immunostimulants.
It is recommended to consume honey in courses, which has antimicrobial activity and functions as a biostimulator. Among medications to strengthen local immunity, it is useful to chew Echinacea tablets and use the drug Imudon.
The presence of bad habits, especially frequent smoking, disrupts the local microflora, irritates the mucous membrane and causes inflammation. Try to gradually reduce the number of cigarettes to give up them painlessly.
Several times a year it is necessary to take courses of multivitamin preparations. Prophylactic treatment usually takes 1-2 months. Pay attention to the quality of your diet. Your daily diet must include vegetables and fruits. Avoid foods that irritate or damage the mucous membrane. Be sure to promptly treat tooth decay and remove tartar at the dentist's office. Carefully choose a specialist who selects the prosthesis and installs it. During the period of adaptation to prosthetics, use the dental gel Cholisal with antimicrobial activity or Metrogyl denta.
Sources:
- https://ProBolezny.ru/stomatit/
- https://stom-info.ru/stomatit/
- https://stomatita.ru/
- https://atvmedia.ru/materials/stomatit-vo-rtu-u-vzroslyh
Treatment of ulcerative stomatitis
Ulcerative stomatitis very often occurs due to poor oral hygiene and bad habits (especially smoking). Often this type of stomatitis at its onset is confused with periodontitis and gingivitis, since it is characterized by inflammation of the gums, a grayish coating around the teeth and death of soft tissues. Often accompanied by fever and fever. One of the few forms of stomatitis, which often requires treatment by a doctor, and in the most advanced cases, surgical intervention.
Treatment methods
- Antibiotic therapy.
- Antibacterial treatment of affected areas.
- Surgical intervention (in severe cases, removal of areas of dead tissue and gum grafting).
Treatment of bacterial stomatitis
This type of stomatitis is also called prosthetic stomatitis, since it occurs due to unsatisfactory care of the orthopedic structure, when many pathogenic microorganisms accumulate in the area of contact between the prosthesis and soft tissues. After treating foci of inflammation, it is necessary to carry out complete cleaning and antibacterial treatment of the prosthesis or replace it. This type of stomatitis should not be confused with allergic stomatitis, which develops against the background of an allergy to the prosthetic material. In this case, the prosthesis must be changed to a hypoallergenic one.
Treatment methods
- Anti-infective therapy.
- Mouth rinse.
Treatment of allergic stomatitis
This type of stomatitis is caused by the body's immunological response to contact with an allergen. The role of the latter can be played by anything: food products, new oral hygiene products, dentures, animal hair and much more. At risk are patients who are predisposed to allergies or suffer from various autoimmune diseases. A distinctive feature of allergic stomatitis is the acute onset of the disease, accompanied by an increase in temperature, severe pain and putrid odor from the mouth, which does not disappear even after thorough brushing of the teeth.
Treatment methods
- Identifying the allergen and eliminating it (or minimizing contact).
- Antihistamine therapy.
- Relief of inflammation with corticosteroids.
- Taking analgesics to relieve pain.
- Local antiseptic drugs
- Diet.
Kinds
Varieties are distinguished according to the depth of damage to the mucous membrane and the reasons that caused the development of the pathology.
According to the depth of the lesion there are:
- aphthous;
- catarrhal;
- necrotic;
- ulcerative
Treatment varies depending on the stage. For the catarrhal variety, local treatment at home is predominantly prescribed. With the most severe necrotic, the child is hospitalized in a hospital.
Clinical manifestations of different types of disease
Signs of stomatitis in children vary significantly. This depends on the nature of the agent causing the disease.
Signs of this pathology:
- Viral - this type of pathology is characterized by the appearance of bubbles with a clear liquid that quickly open. Then erosive areas of round shape and small size are formed. They are covered with a grayish coating. In severe cases, the lesion has a draining character. The mucous membrane of the oral cavity and nasopharynx is bright red. There is pronounced pain. Similar skin rashes are also noted. The child shows signs of general intoxication and elevated body temperature. Signs of enlarged lymph nodes and conjunctivitis are detected. Possible loose stools and vomiting. Mucosal defects are epithelialized without scarring.
- Fungal - most of this species is candidal. It often develops in infants. It can also appear in children wearing braces. In other cases, its occurrence indicates immunodeficiency or other severe somatic pathologies. On the surface of the mucous membrane, areas covered with white plaque appear, then its area increases. A dense white layer covers the entire oral cavity; it has a curd-like consistency. In severe forms, it becomes gray and sometimes separates, exposing the bleeding surface. With the atrophic variety of the disease, only redness and dryness of the mucous membrane are detected. Plaque appears rarely, only in folds.
- Bacterial - the most common type of infection is the impetiginous type. It is characterized by confluent superficial erosive lesions and a purple color of the mucous membranes. Yellowish crusts form that stick the lips together. Salivation increased. There is an unpleasant odor from the mouth. Body temperature rises.
- Autozny - this variety is more common in children under 7 years of age. It is assumed that it is of an infectious-allergic or autoimmune nature. With it, aphthae appear on the mucous membrane - these are painful ulcers of a necrotic nature. They are round in shape, covered with fibrin, surrounded by a reddish granulation rim. The child's temperature rises, he is bothered by pain in his mouth, and refuses to eat. This option has a chronic course. Typically, exacerbations occur once or twice a year. Outside of exacerbation, aphthae heal.
Symptoms in children are quite varied. They depend on the form of the disease and the pathogen that caused it.
Treatment of stomatitis in children
Treatment of childhood and adult stomatitis follows the same methods. At the same time, some drugs used for adults are replaced with those that are better suited for the child’s body. First of all, we are talking about antibiotics, antiseptics and drugs to enhance immunity. Children are often prescribed more gentle methods, which include the use of herbs and natural tinctures for rinsing. At an early age, dentists recommend preventing stomatitis using traditional medicine.
| Age | Type of disease |
| From 0 to 3 years | Candidal stomatitis, or childhood oral thrush. This type of stomatitis is especially common in infants. |
| 1 – 4 years | Aphthous and herpetic stomatitis caused by external infections and mechanical trauma to the oral cavity. |
| Children of primary and secondary school age | Allergic and aphthous stomatitis. |
Treatment of stomatitis at home
I would like to immediately note that treating stomatitis with folk remedies at home is possible, but you need to understand that in many cases it is impossible to do without a visit to a specialist and the use of antibiotics. Ignoring these points can lead to worsening of the disease and longer rehabilitation. In addition, on the Internet you can find a whole lot of “revolutionary” recipes for stomatitis, so you need to be able to separate the wheat from the chaff and understand which remedies can really help, and which are the fruit of the inflamed imagination of “couch healers”. Below we publish the most common methods of preventing and treating stomatitis with folk remedies, but please note that only an experienced specialist can draw up an optimal treatment plan.
In the case of children, treatment of stomatitis with folk remedies at home is used quite often. This is especially justified as a preventive measure, since the child’s body is more susceptible to the influence of the external environment. The most popular remedies are considered to be all kinds of decoctions, for the production of which chamomile, calendula, burdock, propolis and blackberry leaves are used. A homemade ointment is also used to treat stomatitis, which is made from novocaine, egg white and honey. Be that as it may, if your child shows signs of stomatitis, it is best to immediately take him to a specialist who can make the correct diagnosis and plan treatment.
Additional recommendations –
As soon as you notice the appearance of ulcers due to aphthous stomatitis, immediately start taking an antihistamine (anti-allergy) drug, plus eliminate from your diet all the foods and drinks that we described above. Immediately begin local therapy, which includes antiseptic rinses, anti-inflammatory gel + bismuth-based product to protect the surface of the ulcers from irritants. See if your toothpaste contains sodium lauryl sulfate or parabens, and if so, it is worth purchasing a toothpaste without these ingredients.
If brushing your teeth causes pain, then buy a soft toothbrush (they are usually used for inflammation and bleeding gums). For adults and children with constantly recurring outbreaks of aphthous stomatitis, there is an excellent preventive remedy - toothpastes with licorice extract and a whole complex of lactic enzymes. These components increase the protective factors of the oral mucosa, preventing the development of new cases of aphthous stomatitis.
Additional laboratory tests - with frequent, recurring outbreaks, a complete blood count should be performed to rule out hematological diseases. It is important to check blood plasma immunoglobulins and the number of lymphocytes, and take a test for HIV infection. To exclude autoimmune diseases, the patient is usually referred for the following tests:
- erythrocyte sedimentation rate,
- antinuclear antibodies and antineutrophil cytoplasmic antibodies,
- IgA-antiendomysial antibodies,
- antibodies to tissue transglutaminase.
If ulcerative lesions heal very poorly, take a long time and practically do not respond to local treatment, it is necessary to refer the patient for a biopsy to exclude granulomatous conditions such as orofacial granulomatosis, tuberculosis or malignant tumors.
Calling a doctor to your home –
If your child has stomatitis, it is very important to correctly determine its shape. Usually this is either an aphthous or herpetic form of stomatitis, and the most important thing is that they are treated completely differently. If your child develops stomatitis, you should not call the pediatrician. These specialists usually do not even know that there are several forms of stomatitis, and many of them still recommend treating them with brown, blue or Metrogil-dent gel. Or they prescribe a whole bunch of drugs with opposite effects - as if “at once for everything.”
It makes sense to contact a pediatrician only if the child’s general condition is severe, i.e. symptoms of intoxication (high temperature, dehydration...), but such symptoms are characteristic not of aphthous stomatitis, but of primary acute herpetic stomatitis. Therefore, it is optimal to contact a pediatric dentist, and you can always arrange a house call at the reception of a pediatric dental clinic. We hope that our review “Aphthous stomatitis: treatment in adults and children” was useful to you!
Sources:
1. Dental education of the author of the article, 2. National Library of Medicine (USA), 3. Textbook “Pediatric Dentistry” (Kolesov A.A.).4. “Pediatric therapeutic dentistry. National leadership" (Leontyev V.K.). 5. “Clinical recommendations (treatment protocol) for chronic recurrent aphthous stomatitis” (Volkov E.A., Butova V.G.).
Treating stomatitis with home remedies
| Facilities | Description |
| Hydrogen peroxide | Rinsing with a solution of hydrogen peroxide helps reduce discomfort and has an antiseptic effect. |
| Baking soda | Treatment of stomatitis in adults with soda is recommended when the disease is detected in the initial stages. A solution of the substance (a spoon in a glass of water) is recommended for rinsing. |
| Decoctions of chamomile, rose hips and calendula | They have disinfecting properties and contain vitamins and nutrients to maintain oral health. |
Table of children's medications against stomatitis by age
| Drug/Age | 1 month | 3 months | 4 months | 5 months | 7 months | 1 year | 2 years | 3 years | 5 years | 6 years | 10 years |
| Paracetamol | + | + | + | + | + | + | + | + | + | + | + |
| Soda | + | + | + | + | + | + | + | + | + | + | + |
| Candide | + | + | + | + | + | + | + | + | + | + | + |
| Viferon | + | + | + | + | + | + | + | + | + | + | + |
| Suprastin | + | + | + | + | + | + | + | + | + | + | + |
| Ibuprofen | — | + | + | + | + | + | + | + | + | + | + |
| Holisal | — | — | + | + | + | + | + | + | + | + | + |
| Kamistad | — | — | + | + | + | + | + | + | + | + | + |
| Parlazin | — | — | + | + | + | + | + | + | + | + | + |
| Kalgel | — | — | — | + | + | + | + | + | + | + | + |
| Chlorhexidine | — | — | — | — | + | + | + | + | + | + | + |
| Furacilin | — | — | — | — | + | + | + | + | + | + | + |
| Iodinol | — | — | — | — | — | + | + | + | + | + | + |
| Vinylin | — | — | — | — | — | + | + | + | + | + | + |
| Malavit | — | — | — | — | — | + | + | + | + | + | + |
| Fduconazole (Futsis) | — | — | — | — | — | + | + | + | + | + | + |
| Ingalipt | — | — | — | — | — | — | + | + | + | + | + |
| Honey | — | — | — | — | — | — | + | + | + | + | + |
| Propolis | — | — | — | — | — | — | + | + | + | + | + |
| Nystatin | — | — | — | — | — | — | + | + | + | + | + |
| Oxolinic ointment | — | — | — | — | — | — | + | + | + | + | + |
| Hexoral | — | — | — | — | — | — | — | + | + | + | + |
| Miramistin | — | — | — | — | — | — | — | + | + | + | + |
| Lugol | — | — | — | — | — | — | — | — | + | + | + |
| Stomatidin | — | — | — | — | — | — | — | — | + | + | + |
| Stomatophyte | — | — | — | — | — | — | — | — | — | + | + |
| Metrogil Denta | — | — | — | — | — | — | — | — | — | + | + |
| Hydrogen peroxide | — | — | — | — | — | — | — | — | — | — | + |
| Chlorophyllite | — | — | — | — | — | — | — | — | — | — | + |
| Aekol | — | — | — | — | — | — | — | — | — | — | + |