Every caring mother can share her experience of worrying about children’s illnesses, especially if it concerns infants.
There is definitely no need to panic when identifying signs of disease; precious time is wasted. What to do if ulcers are detected on the tongue and which specialist to contact will be discussed in the article.
Possible causes of ulcers on a child’s tongue
Ulcers on the tongue are a symptomatic manifestation characteristic of several diseases. It makes no sense to treat a symptom without eliminating the provoking factor.
Therefore, the primary task is to determine the cause, which is achieved by analyzing a set of signs:
| Causes of ulcers on the tongue | ||
| Name | Description | Associated symptoms |
| Aphthous stomatitis | The disease is characterized by the formation of ulcers on the tongue with a diameter of 1 to 5 mm. The wounds hurt a lot, which is why the child becomes restless and irritable. When there is mechanical impact on the aphthae, they begin to bleed. | Initially, redness appears on the tongue; if left untreated, it turns into gray or white ulcers. Due to the burning and pain from aphthae, eating is difficult. There is also a spreading white coating on the surface of the tongue. |
| Herpes stomatitis | Herpes stomatitis is contagious, caused by the Herpes virus. Many ulcers appear in the child's mouth, which is similar to a rash. The formed bubbles quickly burst, leaving wounds in their place. The lesion is often transferred to the skin of the face, lips and nose. | Blisters on the tongue contain a clear or slightly yellowish liquid. After a breakthrough, painful gray-white ulcers with a narrow scarlet rim are formed. There is also an increased body temperature and an increase in the size of the lymph nodes. |
| Thrush (candidiasis) | The causative agent of the disease is Candida fungi, transmitted through toys, dishes and other household items. The disease can also develop under the influence of infections, hormonal fluctuations (adolescence), and also as a result of hypothermia. | In the absence of treatment, in addition to yellowish and white ulcers, the following are observed: swelling, dry mouth, tightness of the mucous membrane, increased body temperature, cracks in the corners of the mouth. The sores emit an unpleasant odor due to suppuration. |
| Allergy | Formations on the tongue are caused by the body's reaction to an allergen. | The disease manifests itself in the form of red spots and ulcers with blurred outlines. Over time they merge. Other symptoms are: swelling of the lip, face. |
| Gastrointestinal problems | The tongue reflects any problems in the body. If there are problems with the gastrointestinal tract, white ulcers form. | In addition to ulcers on the white tongue, there are: disturbances in the microflora of the oral cavity, discomfort when chewing food and swallowing. The outbreaks are located in small clusters. |
| Tongue injuries | Injury to the tongue or mucous membrane occurs frequently. Ulcers appear in the area of tissue damage. | The ulcers are usually painless and are recognized by their pink or reddish color. If the wounds become infected, yellowish pus may form. Apart from pain at the site of injury, no other symptoms are noted. |
Causes
Stomatitis is a disease that affects the mucous surfaces of the oral cavity. This is an acute inflammatory process of various etiologies, which is manifested by the appearance of yellowish or whitish pimples with liquid and ulcers. It can occur in children and adults, but children are much more likely to suffer from the disease.
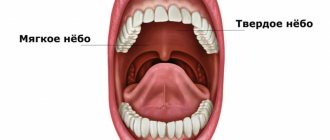
The rash affects the inside of the cheeks, gums, and tongue. Their appearance causes discomfort, since ulcerative wounds itch, hurt, and there is a constant burning sensation in the mouth.
Young children have extremely delicate oral mucous membranes. The body’s insufficiently developed defense system is not able to quickly cope with infectious agents, so the natural reaction of the immune system to their entry into the body is inflammation. Common causes of the disease are:
- insufficient oral hygiene;
- chronic gastrointestinal diseases;
- mucosal injuries;
- burn;
- ingestion of pathogenic bacteria from hands or toys.
Important! Treatment of stomatitis in children is possible at home. However, in order to choose the right treatment regimen, you cannot do without consulting a specialist.
Associated symptoms and what they indicate
Diagnosis of the disease is carried out taking into account the accompanying symptoms.
- Small sores on the tongue and lips may indicate a viral infection - herpes
Temperature indicates an inflammatory process. This is typical for candidiasis, herpes, allergies, and aphthous stomatitis.
- Ulcers located under the tongue appear due to injury, candidiasis, and somatic diseases.
- On the tip of the tongue, sores most often form due to mechanical damage to tissue.
- Accompanied by plaque ulcers due to candidiasis and problems with the gastrointestinal tract.
- Small sores on the tongue and lips may indicate a viral infection - herpes. Thrush ulcers often spread to the lips.
- On the tongue and throat, ulcers are formed as a result of mechanical trauma, malocclusion, dehydration, vitamin deficiency, and the use of medications with a high concentration of active substances.
- Ulcers in a baby indicate possible problems with the internal systems of the body. May indicate an allergic reaction, vitamin deficiency, mechanical damage to the tongue, fungal or viral infection.
Diagnostics
A qualified doctor is able to recognize the disease by carefully examining the surface of the tongue. The average person can get acquainted with the basics of diagnostics, but actually using them in everyday life is problematic, since the etiology of diseases can be different.
If you detect ulcers on a child’s tongue, you should not self-medicate using various rinses and lotions. You should make an appointment with your pediatrician or pediatric dentist as soon as possible, especially if the ulcers are spreading rapidly.
During diagnostic procedures, a number of tests are performed:
- cytological (the cellular composition of the mucous membrane and plaque on it is studied, Candida fungi are detected);
- biochemical (control of the level of glucose and important microelements in the blood, on which the condition of the epithelial layer depends);
- bacteriological (the bacterial composition of the oral cavity is studied in order to identify dysbiosis and inflammatory processes of bacterial origin);
- immunological (presence of disturbances in the protective function of the body).
The method of differential diagnosis is also used.
Medicines to treat pain
If wounds occur on the tongue, the following are prescribed:
- Antiseptic drugs that help fight microbes and also reduce the sensitivity of the mucous membrane due to analgesic components. Similar medications include: Hexoral, Ingalipt, Strepsils.
- Disinfecting medications (alcohol, brilliant green, iodine, hydrogen peroxide). The listed medications must be used very carefully in order to avoid burns to the mucous membrane. To treat the wound, you need to moisten a cotton swab in the healing composition and apply it pointwise to the affected area.
- Dental gels.
These products also disinfect and anesthetize wounds. These include: Kamistad, Metrogyl, Cholisal, Solcoseryl.
We recommend watching a video about treating sores in the mouth:
In addition, it is recommended to rinse the mouth with sea water. To make such a medicine, you need to combine water with salt, iodine and soda. This procedure can also be carried out using a solution of Furacilin, Chlorhexidine, Chlorophyllipt, and propolis tincture.
Treatment methods
The tactics for treating ulcers on a child’s tongue depends on the type of disease and its course.
Aphthous stomatitis
The most common disease is aphthous stomatitis.
The following reasons can provoke its development:
- Sometimes the aphthous form of stomatitis in a child is often confused with the herpes virus
stress;
- genetic factor;
- lack of vitamins;
- allergy;
- folic acid deficiency.
Sometimes the aphthous form of stomatitis in a child is often confused with the herpes virus.
Mistakes can be avoided by carefully monitoring the development of the disease.
With stomatitis, at the initial stage, red dots form, after which white and gray bubbles with a red rim form in their place. Ulcers appear after the blisters burst.
To treat aphthous stomatitis, an integrated approach is used, including:
- systematic procedures for rinsing the mouth with decoctions of medicinal plants (calendula, chamomile, tea tree, etc.) and solutions of potassium permanganate, lugol;
- local treatment of affected areas of the mucous membrane with pharmacological agents (for example, methyluracil ointment).
The duration of treatment depends on the severity of the disease and the regularity of the procedures.
Herpetic stomatitis
Drug treatment is prescribed by a doctor, taking into account the characteristics of the body and the degree of neglect of the disease.
Treatment of the disease in its advanced form is carried out in a pediatric hospital or infectious diseases department.
Mild cases of herpetic stomatitis are carried out on an outpatient basis, but the child is isolated from others due to the fact that he is a carrier of the virus.
Drug treatment is prescribed by a doctor, taking into account the characteristics of the body and the degree of neglect of the disease.
Among the recommended drugs:
- antiviral (Acyclovir, Zovirax, Oxolinic ointment, etc.);
- antihistamines (Cetirizine, Loratadine, Fenistil);
- anti-inflammatory (Ibuprofen, Paracetamol);
- wound healing (solutions of Trypsin or Chymotrypsin);
- antiseptic (Solutions of Chlorhexidine, Furacilin);
- immunostimulating (Imudon, echinacea extract, etc.).
In case of acute or recurrent stomatitis of the herpes form, physiotherapy or laser therapy procedures are also prescribed.
Thrush (candidiasis)
Starting at six months of age, doctors prescribe topical antifungals
Choosing a treatment method for babies is quite difficult, because babies cannot describe their symptomatic sensations.
The mother needs to closely monitor the child to understand the cause of thrush.
If this is regurgitation after eating, then it is worth reducing the diet or keeping the baby upright for 20 minutes every time after eating.
It is equally important to maintain hygiene and sanitary standards in your home.
The following methods are used to treat infants:
- treatment of the oral mucosa with a cotton swab dipped in soda solution (1 tsp per 200 ml of warm water);
- wiping the oral mucosa with gauze soaked in a weak solution of potassium permanganate.
It is advisable to carry out procedures at an early stage of the development of a fungal infection, then the chances of recovery double. Pediatricians rarely prescribe antifungal agents for infants.
Starting from six months of age, doctors prescribe topical antifungals. When the disease progresses to a severe form, an integrated approach is used, which combines internal and local drugs.
The following drugs are used to treat older children:
- Miramistin (ointment, solution);
- Nystatin (tablets);
- Diflucan (tablets);
- Clotrimazole (ointment, tablets), etc.
Allergy
Most often, the allergen is found in foods, hygiene products, and medications.
Red ulcers on a child’s tongue may appear as a result of the body’s reaction to an allergen (causative agent).
There is no point in treating the consequences; the main thing is to identify the product or substance that caused the formation of wounds on the tongue as quickly as possible.
Most often, the allergen is found in foods, hygiene products (you need to carefully study the composition), and medications.
Dental fillings, dentures, and braces can also provoke an allergic reaction.
Gastrointestinal problems
In infants, the digestive system is still at the stage of formation, so the gastrointestinal tract is very sensitive to many irritants.
Any failures provoke a violation of the absorption of nutrients into the blood, against which vitamin deficiency develops, spots and ulcers appear on the tongue.
Another reason for changes in microflora are antibiotics, so they are prescribed in combination with drugs containing beneficial bacteria.
The essence of treating ulcers comes down to eliminating problems in the gastrointestinal tract and treating the lesions with special local agents.
Tongue injuries
Scarlet ulcers can also appear on a child’s tongue as a result of injury:
- careless use of a toothbrush;
- biting the tongue with teeth;
- tissue injury from sharp edges of a damaged tooth or filling;
- due to the eruption of baby teeth;
- poor-quality installation of the prosthesis when correcting the bite, etc.
Treatment of wounds in such cases consists of eliminating the irritant and local treatment of the lesions with wound-healing agents.
Types of stomatitis common in children?
Treatment of stomatitis will directly depend on the correct diagnosis of the form of the disease and the severity of its manifestation. Below are the forms of stomatitis that are most common in children.
- Herpetic stomatitis in a child is expressed by multiple small or merging blisters, gradually turning into erosions with a white-gray coating.
- Aphthous stomatitis in children is one, two or three elements of a round-shaped rash (aphtha) with a diameter of 5-10 mm with a red rim around.
- Candidal stomatitis in infants is a whitish “curdled” coating on the tongue or cheeks, tightly fused to the mucous membrane.
- Angular stomatitis , seizures - erosions with crusts in the corners of the mouth.
Children may also encounter toxic-allergic, bacterial, erosive, and many types of specific (arising against the background of a specific infection) stomatitis, but the most common are acute herpetic, chronic recurrent herpetic, chronic recurrent aphthous and angular stomatitis.
What is stomatitis?
Stomatitis is the general name for a large group of diseases of the oral mucosa, which are characterized by a general picture of inflammation, as well as the appearance of specific rash elements on the mucosa (depending on the type of stomatitis).
This disease can occur in both adults and children, with the only difference being that some types of “adult” stomatitis do not occur in children (prosthetic stomatitis or stomatitis associated with smoking).
What are the causes of stomatitis in children and infants?
In children and infants, in most cases, the cause of stomatitis is infection. Stomatitis is often associated with ARVI, although the virus is not directly involved in stomatitis.
Stomatitis occurs against the background of a decrease in general immunity, against the background of local immunity in the oral cavity, and can also occur due to injury and subsequent infection of the mucous membrane. With general diseases (acute respiratory infections, acute respiratory viral infections, severe systemic diseases), the body’s overall resistance decreases, which contributes to the development of stomatitis. With viral infections accompanied by a runny nose and cough, the oral mucosa dries out, resulting in a decrease in local resistance - this also contributes to the development of stomatitis.
How to treat ulcers at home - traditional methods
As an additional treatment for ulcers on the tongue, you can use traditional medicine recipes:
- It is effective to use mouth rinses with home-prepared decoctions of plants that have antiseptic properties (calendula, sage, St. John's wort, viburnum berries, rose hips, chamomile, linden flowers). The brewing technology is simple - a tablespoon of dry plant is poured with 250 ml of boiling water. The container with the lid closed is left for 30-40 minutes. After filtering, you can carry out procedures. The oral cavity should be treated at least 5 times throughout the day. Keep the liquid in your mouth for about a minute each time you rinse.
- Ulcers will heal faster if they are treated with wound healing agents. These are mainly essential oils: sea buckthorn, calendula, rose hips, as well as aloe and Kalanchoe juices. They need to be applied pointwise, capturing only the affected tissue.
- Among the effective recipes, a solution based on soda , salt, iodine stands out (3 drops of iodine and a teaspoon of bulk ingredients per 200 ml of water). Applications and rinsing should be carried out at least 3-4 times a day for a week.
It is difficult to carry out medical procedures for babies less than a year old, and not all traditional methods can be used.
Therefore, the following treatment options for tongue ulcers have long been used for them:
- treatment of lesions with hydrogen peroxide;
- wiping the oral cavity, including the tongue, with a mixture of milk (100 ml), one yolk and honey (1 tsp);
- taking yarrow juice with honey (1 spoon 3 times a day for 3 weeks);
- processing with a mixture of egg white and water.
In what cases is it necessary to consult a doctor?
If you use folk recipes when identifying ulcers, you can get rid of them without the help of a doctor. But at the same time, the child’s condition must be stable.
If after a week’s treatment the lesions do not dry out or, in addition to them, other alarming symptoms appear (temperature, fever), then you should not hesitate to visit the clinic.
Herpetic stomatitis in children
Causes
This is an infectious stomatitis that occurs under the influence of the herpes virus. There are acute and chronic recurrent herpetic stomatitis. Acute herpetic stomatitis occurs when a child is first infected and occurs most often between the ages of 6 months and 3 years. In 100% of cases, the child gets the infection from parents and other close people (when they lick the child’s spoon and continue to feed him further, lick the pacifier or drink from the same cup). At this age, the child no longer has the antibodies that he gets from his mother’s milk, and has not yet developed his own. Therefore, when a virus enters the body, a disease inevitably begins. In its acute form, such an infection manifests itself in only 10% of children, and all the rest tolerate the primary infection quite easily.
Chronic recurrent stomatitis is due to the fact that the herpes virus, once entering the body, settles there forever and under favorable conditions (the above-mentioned decrease in immunity) can provoke repeated rashes.
The symptoms of acute and chronic herpetic stomatitis are different. In both forms, there are general phenomena (in the body as a whole) and a specific picture in the oral cavity.
Symptoms
Acute herpetic stomatitis
- General deterioration in health. Acute herpetic stomatitis is characterized by weakness, headache, pain in joints and muscles, malaise - general symptoms of intoxication caused by viral activity. The temperature is usually raised to 37 -41 degrees in the first or second day. The lymph nodes (especially the submandibular ones) enlarge and become painful.
In the oral cavity there are:
- swelling;
- redness of the mucous membrane;
- soreness of the mucous membrane in the cheeks, lips, tongue, palatine arches;
- small (the size of a millet grain) bubbles, usually collected in groups filled with a clear liquid; over time, the liquid becomes cloudy, and after 2-3 days the bubbles burst, and a bright red erosion forms in their place. Even later, the surface of the erosion becomes covered with a fibrinous coating (whitish or yellowish). These white spots are surrounded by a red corolla.
- Redness and swelling of the gum edge around the teeth and redness of the interdental papillae are often observed (clinic of gingivitis).
Along with rashes in the mouth, rashes are often observed at the border of the red border of the lips and skin or at the border of the nasal mucosa and skin.
Chronic herpetic stomatitis
All symptoms in the oral cavity repeat the picture of acute herpetic stomatitis, but the general condition, as a rule, does not suffer.
Factors that provoke exacerbations of chronic herpetic stomatitis:
- acute respiratory infections, acute respiratory viral infections, hypothermia;
- avitaminosis;
- allergy;
- stress;
- taking immunosuppressive drugs;
- exacerbation of chronic tonsillitis, sinusitis and other diseases;
- trauma to the oral mucosa;
- foci of infection in the oral cavity (carious teeth, hard and soft dental plaque, gingivitis);
- breathing through the mouth (due to this, drying out of the mucous membrane occurs, which provokes a decrease in local immunity, as well as the formation of cracks on the lips).
Treatment of herpetic stomatitis in a child
Be sure to consult a dentist for an accurate diagnosis. If it is not possible to see a doctor on the first day, you can start treatment, but a visit to the doctor as soon as possible is required.
Antiviral therapy (to combat the pathogen)
- Acyclovir (tablets) or Viferon (gel, suppositories) - depending on the age of the child. Suppositories are more suitable for infants and children up to one year old; older children can be given tablets or treated with gel.
- For rashes that are observed only on the skin, antiviral ointments are used (acyclovir, Viferon, Zovirax and others).
Antiviral drugs are taken according to the regimen specified in the instructions. The sooner you start taking the drug, the more active it will be against the virus. These drugs are taken on days 1-4 of the disease.
Antiseptic treatment (prevention of complications)
- Miramistin (rinse aid) is used directly as a rinse. For young children who cannot yet rinse their mouths themselves, wiping with a gauze swab dipped in a solution of the drug is used. Other antiseptics are either not used at all (since they are not effective against viruses), or are used in combination with miramistin (alternately). You can take chlorhexidine, givalex, rotokan, chlorophyllipt, but all this is only in combination with miramistin.
Keratoplasty (drugs to stimulate mucosal healing)
- solutions of vitamins A and E (you can buy an oil solution at the pharmacy). Applications are made after rinsing with an antiseptic (the drug is applied to a gauze turunda and the wound surface is lubricated).
- rosehip or sea buckthorn oil. Also in the form of applications.
- solcoseryl (after rinsing, apply a thin layer of gel using an ear stick or a clean finger).
One of these drugs to choose from.
Symptomatic treatment
- If soreness of the mucous membrane interferes with eating and hygiene - Dentol or its analogues (drugs used in children during teething) - lubricate the surface of erosions before eating or brushing teeth.
- If the temperature is above 38 degrees - paracetamol, nurofen, ibuprofen, mefenamic acid or any other antipyretics (according to the instructions).
- drinking plenty of fluids to reduce symptoms of intoxication;
- diet excluding spicy, salty, sour, hard foods, allergens (citrus fruits, chocolate, honey);
- Immunostimulants: imunal, amiksin, imudon and others - as prescribed by a doctor.
Preventive measures
Diseases characterized by the formation of ulcers on the tongue can be avoided if preventive measures are taken in a timely manner:
- If, after the measures taken, ulcers appear on the tongue again, it is recommended to undergo a more thorough examination.
visit the dentist regularly;
- Brush your teeth and mouth twice a day with high-quality toothpaste;
- teach your child to rinse his mouth after every meal to remove small particles;
- strictly adhere to restrictions regarding the consumption of foods that cause an allergic reaction;
- develop a diet so that it contains 65-70% fresh vegetables and fruits;
- take vitamin complexes to maintain immunity;
- protect the child from stress.
If, after taking measures, ulcers appear on the tongue again, it is recommended to undergo a more thorough examination. This sign may indicate problems with the digestive system or other diseases.